20
The Dental Pulp
A healthy dental pulp ensures survival of a natural tooth and any artificial restorations. The sections below discuss recent thinking and developments for clinical management of pulpal diseases.
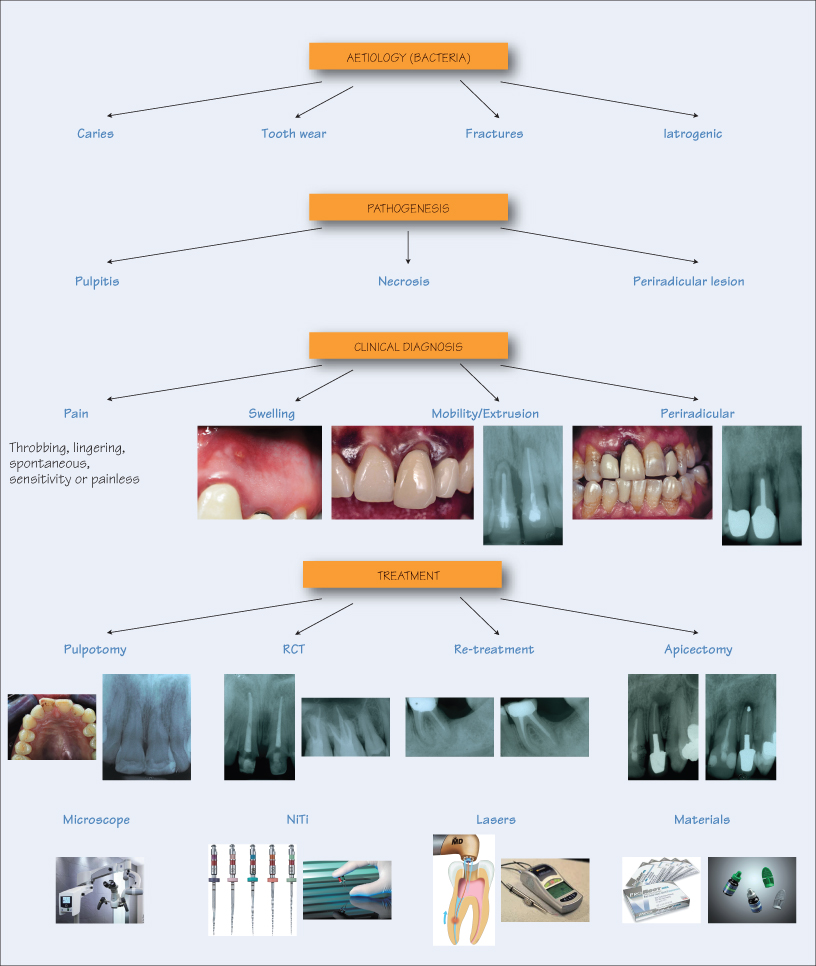
Aetiology
Pulpal diseases are bacterial in origin, from the resident oral microbiota, either directly or indirectly. Some causes include:
- Caries – direct bacterial assault of the pulp;
- Tooth wear – eventual pulpal pathosis due to attrition, abrasion, erosion and abfraction;
- Tooth fractures – pulp exposure due to extra-oral accidents or masticatory misadventures;
- Iatrogenic – pulp exposure during restorative procedures.
Examples of microbes found in root canals and periradicular lesions include Enterococcus faecalis, Candida albicans, Actinomyces israelii, Propionibacterium propionicum, cytomegalovirus and the Epstein–Barr virus.
Pathogenesis
Whatever the cause, microorganisms initiate an inflammatory response (pulpitis). Bacterial toxins precede bacterial invasion, causing a vascular response by releasing cytokines and mediators. If the bacterial insult is confined to the hard tissues, a reparative and protective secondary dentine barrier is formed. If the pulp is exposed, formation of a soft tissue barrier is impossible since the pulp is devoid of epithelial cells. Therefore, the bacterial invasion and proliferation is profuse, leading to colonisation of the root canal system and subsequently the periradicular areas. The infected periradicular areas react with a protective response by bone resorption to contain and eliminate the infection, which is visible as an osteolytic bone lesion (periapical lesion) on a radiograph.
Clinical Manifestations and Diagnosis
Precise and efficient d/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


