Sensory and motor changes
INTRODUCTION
Sensory, motor or autonomic neuropathies may affect the orofacial region. The main orofacial sensory and motor lesions are shown in Table 20.1.
Table 20.1
| Features | V | VII |
| Major | Sensory loss in face | Weak muscles of facial expression |
| Minor | Jaw movements impaired | Reduced sense of taste in anterior ⅔ of tongue |
SENSORY CHANGES
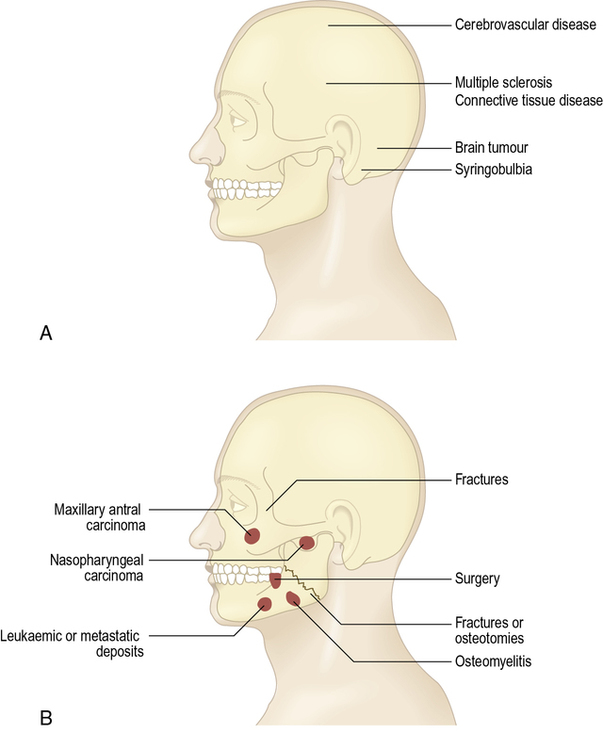
Normal facial sensation, mediated by the trigeminal nerve, is important to protect the skin, mucosae and especially the cornea of the eye from damage. Facial sensory changes, which can be caused by lesions of a sensory branch of the trigeminal nerve or the central connections (Fig. 20.1), may lead to sensory awareness that is:
 partially lost (hypoaesthesia)
partially lost (hypoaesthesia)
 altered (paraesthesia) – often ‘pins and needles’ or similar discomfort – which may arise during recovery from nerve damage
altered (paraesthesia) – often ‘pins and needles’ or similar discomfort – which may arise during recovery from nerve damage
Sensory defects may lead to unrecognized damage from trauma or burns (‘trophic lesions’), and are occasionally associated with hyperaesthesia (i.e. the patient has a decreased sensory perception, but when sensation is perceived, it may cause discomfort).
AETIOLOGY AND PATHOGENESIS
Causes of lesions affecting the trigeminal nerve are shown in Boxes 20.1 and 20.2.
EXTRACRANIAL CAUSES
Trauma
 Trauma to the mandibular division can have a variety of causes:
Trauma to the mandibular division can have a variety of causes:
 inferior alveolar local analgesic injections
inferior alveolar local analgesic injections
 fractures of the mandibular body or angle
fractures of the mandibular body or angle
 surgery (particularly surgical extraction of lower third molars, osteotomies or jaw resections) or even endodontics or implants.
surgery (particularly surgical extraction of lower third molars, osteotomies or jaw resections) or even endodontics or implants.
 Trauma to the mental nerve can have a variety of causes:
Trauma to the mental nerve can have a variety of causes:
 pressure from a denture – the mental foramen is close beneath a lower denture and there is anaesthesia of the lower lip on the affected side.
pressure from a denture – the mental foramen is close beneath a lower denture and there is anaesthesia of the lower lip on the affected side.
 Trauma to the lingual nerve can arise especially during resections or removal of lower third molars, particularly when the lingual split technique is used.
Trauma to the lingual nerve can arise especially during resections or removal of lower third molars, particularly when the lingual split technique is used.
 Trauma to branches of the maxillary division of the trigeminal nerve may be caused by direct trauma or fractures (usually Le Fort II or III middle-third facial fractures) or surgery.
Trauma to branches of the maxillary division of the trigeminal nerve may be caused by direct trauma or fractures (usually Le Fort II or III middle-third facial fractures) or surgery.
Neoplastic disease
 Oral carcinomas may invade the jaws to cause anaesthesia.
Oral carcinomas may invade the jaws to cause anaesthesia.
 Skull base or central malignancies such as osteosarcoma may produce a similar pattern.
Skull base or central malignancies such as osteosarcoma may produce a similar pattern.
 Nasopharyngeal carcinomas may invade the pharyngeal wall to infiltrate the mandibular division of the trigeminal nerve, causing pain and sensory loss in the region of the inferior alveolar, lingual and auriculotemporal nerve distributions; invade the levator palati to cause soft palate immobility; and, by occluding the Eustachian tube, cause deafness (Trotter syndrome).
Nasopharyngeal carcinomas may invade the pharyngeal wall to infiltrate the mandibular division of the trigeminal nerve, causing pain and sensory loss in the region of the inferior alveolar, lingual and auriculotemporal nerve distributions; invade the levator palati to cause soft palate immobility; and, by occluding the Eustachian tube, cause deafness (Trotter syndrome).
 Leukaemia, myeloma or metastases (usually from breast, lung, stomach or colon cancer) may cause deposits in the mandible and labial hypoaesthesia.
Leukaemia, myeloma or metastases (usually from breast, lung, stomach or colon cancer) may cause deposits in the mandible and labial hypoaesthesia.
 Carcinoma of the maxillary antrum may produce ipsilateral upper labial hypoaesthesia or anaesthesia.
Carcinoma of the maxillary antrum may produce ipsilateral upper labial hypoaesthesia or anaesthesia.
Intracranial lesions
Intracranial lesions affecting the trigeminal nerve or connections are uncommon but often serious.
 Trauma including surgical treatment of trigeminal neuralgia.
Trauma including surgical treatment of trigeminal neuralgia.
 Neoplasms, such as brain tumours (often metastases).
Neoplasms, such as brain tumours (often metastases).
 since other cranial nerves are anatomically close, there may be associated neurological deficits in intracranial causes of facial sensory loss. Thalamic strokes in particular can cause facial sensory loss
since other cranial nerves are anatomically close, there may be associated neurological deficits in intracranial causes of facial sensory loss. Thalamic strokes in particular can cause facial sensory loss
 in posterior cranial fossa lesions, for example, there may be cerebellar features, such as ataxia
in posterior cranial fossa lesions, for example, there may be cerebellar features, such as ataxia
 in middle cranial fossa lesions there may be associated neurological deficits affecting cranial nerve VI and thus mediolateral eye movements.
in middle cranial fossa lesions there may be associated neurological deficits affecting cranial nerve VI and thus mediolateral eye movements.
 Brainstem lesions that may involve the fifth nuclei and central connections include brainstem:
Brainstem lesions that may involve the fifth nuclei and central connections include brainstem:
 syringobulbia: this leads to sensory loss spreading from the periphery of the face inwards towards the nose, plus a lower motor nerve lesion of the vagus, hypoglossal and accessory nerves, leading to disturbances of speech and swallowing, and bilateral upper motor neurone lesions affecting all limbs. A ‘syringomyelia-like’ syndrome has been infrequently reported in neurological disorders such as Tangiers disease, lepromatous leprosy and a novel syndrome termed ‘facial onset sensory and motor neuronopathy syndrome’ (FOSMN).
syringobulbia: this leads to sensory loss spreading from the periphery of the face inwards towards the nose, plus a lower motor nerve lesion of the vagus, hypoglossal and accessory nerves, leading to disturbances of speech and swallowing, and bilateral upper motor neurone lesions affecting all limbs. A ‘syringomyelia-like’ syndrome has been infrequently reported in neurological disorders such as Tangiers disease, lepromatous leprosy and a novel syndrome termed ‘facial onset sensory and motor neuronopathy syndrome’ (FOSMN).
 Cerebellopontine angle lesions that can compress the trigeminal nerve and as they enlarge, affect the neighbouring seventh and eighth nerves, producing facial weakness and deafness include:
Cerebellopontine angle lesions that can compress the trigeminal nerve and as they enlarge, affect the neighbouring seventh and eighth nerves, producing facial weakness and deafness include:
 Petrous temporal bone lesions may cause pain and also affect the sixth nerve (Gradenigo’s syndrome) and include the following.
Petrous temporal bone lesions may cause pain and also affect the sixth nerve (Gradenigo’s syndrome) and include the following.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses