Principles and Techniques of Disinfection
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Explain why dental treatment room surfaces need barriers or disinfection.
• List the types of surfaces in the dental office that are typically covered with barriers.
• Describe two methods to deal with surface contamination.
• Name types of items that are single-use only.
• Name the types of items that may be single-use or reusable.
• Explain the difference between disinfection and sterilization.
• Explain the difference between a disinfectant and an antiseptic.
• Name the government agency that is responsible for registering disinfectants.
• Demonstrate the process of cleaning and disinfecting a treatment room.
• Demonstrate the process of precleaning contaminated dental instruments.
• Explain the precautions that should be taken when chemical sterilants/disinfectants are used.
• Describe the CDC guidelines for disinfecting clinical contact surfaces.
• Describe the CDC guidelines for disinfecting housekeeping surfaces.
Performance Outcomes
On completion of this chapter, the student will be able to meet competency standards in the following skills:
Electronic Resources
![]() Additional information related to content in Chapter 20 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 20 can be found on the companion Evolve Web site.
![]() and the Multimedia Procedures DVD
and the Multimedia Procedures DVD
Key Terms
Antiseptic Substance for killing microorganisms on the skin.
Bioburden Blood, saliva, and other body fluids.
Broad-spectrum activity Capable of killing a wide range of microbes.
Chlorine dioxide Effective, rapid-acting environmental surface disinfectant or chemical sterilant.
Clinical contact surface Surface touched by contaminated hands, instruments, or spatter during dental treatment.
Disinfectant Chemical used to reduce or lower the numbers of microorganisms on inanimate objects.
Fungicidal (fun-ja-SI-dal) A product that is capable of killing fungi.
Greener Infection Control Minimizing the environmental impact of infection control products and procedures.
Glutaraldehyde (gloo-tuh-RAL-duh-hide) Environmental Protection Agency (EPA)–registered high-level disinfectant.
High-level disinfectant Hospital disinfectant with tuberculocidal activity.
Hospital disinfectant Disinfectant with the ability to kill Staphylococcus aureus, Salmonella choleraesuis, and Pseudomonas aeruginosa.
Housekeeping surface Surface that is not contaminated during dental treatment (e.g., floors, walls).
Immersion disinfectant Disinfectant used for immersion (soaking) of heat-sensitive instruments.
Intermediate-level disinfectant Liquid disinfectant with EPA registration as a hospital disinfectant with tuberculocidal activity. It is used for disinfecting operatory surfaces.
Iodophor (eye-oe-doe-FOR) EPA-registered, intermediate-level hospital disinfectant.
Low-level disinfectant Disinfectant that destroys certain viruses and fungi; used for general housecleaning (e.g., walls, floors).
Precleaning Removal of bioburden before disinfection.
Residual activity Action that continues long after initial application, as with disinfectants.
Reuse life Time period that a disinfectant should remain effective during use and reuse.
Shelf life How long a product may be stored before use.
Single-use items Items that are used on only one patient and then are thrown away.
Sodium hypochlorite (hye-poe-KLOR-ite) Surface disinfectant commonly known as household bleach.
Splash, spatter, and droplet surface Surface that does not contact members of the dental team or contaminated instruments or supplies.
Sporicidal Capable of killing bacterial spores.
Sterilant (STER-i-lunt) Agent that kills all microorganisms.
Sterilization (ster-i-li-ZAY-shun) Process that kills all microorganisms.
Surface barrier Fluid-resistant material used to cover surfaces likely to become contaminated.
Synthetic phenol (sin-THEH-tik FEE-nol) compound EPA-registered intermediate-level hospital disinfectant with broad-spectrum disinfecting action.
Touch surface Surface directly touched and contaminated during procedures.
Transfer surface Surface not directly touched but often contacted by contaminated instruments.
Tuberculocidal (too-bur-kyoo-loe-SYE-dul) Capable of inactivating tuberculosis-causing microorganisms.
Virucidal Capable of killing some viruses.
During patient treatment, dental equipment and treatment room surfaces are likely to become contaminated with saliva or aerosol containing blood and saliva. Surfaces that are touched frequently (e.g., light handles, unit controls, drawer handles) can act as reservoirs for microorganisms. When these surfaces are touched, microbial agents can be transferred to instruments; to charts; or to the nose, mouth, or eyes of dental team members or of other patients. A primary source of cross-contamination can be seen when a member of the dental team touches surfaces with contaminated gloved hands.
Laboratory studies have determined that microorganisms may survive on environmental surfaces for different lengths of time. For example, Mycobacterium tuberculosis may survive for weeks, whereas the herpes simplex virus dies in a matter of minutes. It is impossible to predict accurately the life span of microorganisms on the surfaces of dental equipment. Therefore, the safest approach for avoiding contamination is to assume that if the surface has had contact with saliva, blood, or other potentially infectious material, live microorganisms are present.
Note: Throughout this chapter, recommendations of the Centers for Disease Control and Prevention (CDC) are indicated, and the category of scientific evidence is noted at the end of each recommendation.
Environmental Infection Control
The CDC Guidelines for Infection Control in Dental Healthcare Settings—2003 divide environmental surfaces into clinical contact surfaces and housekeeping surfaces. Housekeeping surfaces include floors, walls, and sinks. Because these have a much lower risk for disease transmission, cleaning and decontamination techniques are not as rigorous as those used for clinical areas and for patient treatment items.
Things to consider when one is planning for cleaning and disinfection of patient treatment areas include the following:
• Amount of direct patient contact
• Type and frequency of hand contact
Clinical Contact Surfaces
Clinical contact surfaces can be directly contaminated by direct spray or spatter generated during dental procedures, or by contact with the dental professional’s gloved hands.
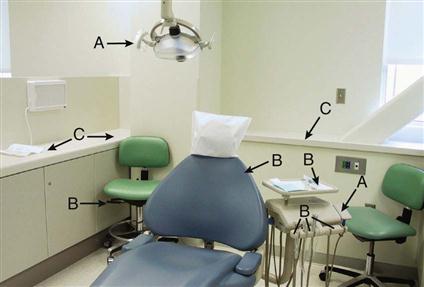
Current infection control guidelines of the Organization for Safety and Asepsis Procedures (OSAP) recommend that clinical surfaces should be classified and maintained under three categories: (1) touch, (2) transfer, and (3) splash, spatter, and droplet (Fig. 20-1).
Touch surfaces are directly touched and contaminated during treatment procedures. Touch surfaces include dental light handles, dental unit controls, chair switches, chairside computers, pens, telephones, containers of dental materials, and drawer handles.
Transfer surfaces are not directly touched but often are touched by contaminated instruments. Transfer surfaces include instrument trays and handpiece holders.
Splash, spatter, and droplet surfaces do not actually contact members of the dental team or contaminated instruments or supplies. Countertops are a major example.
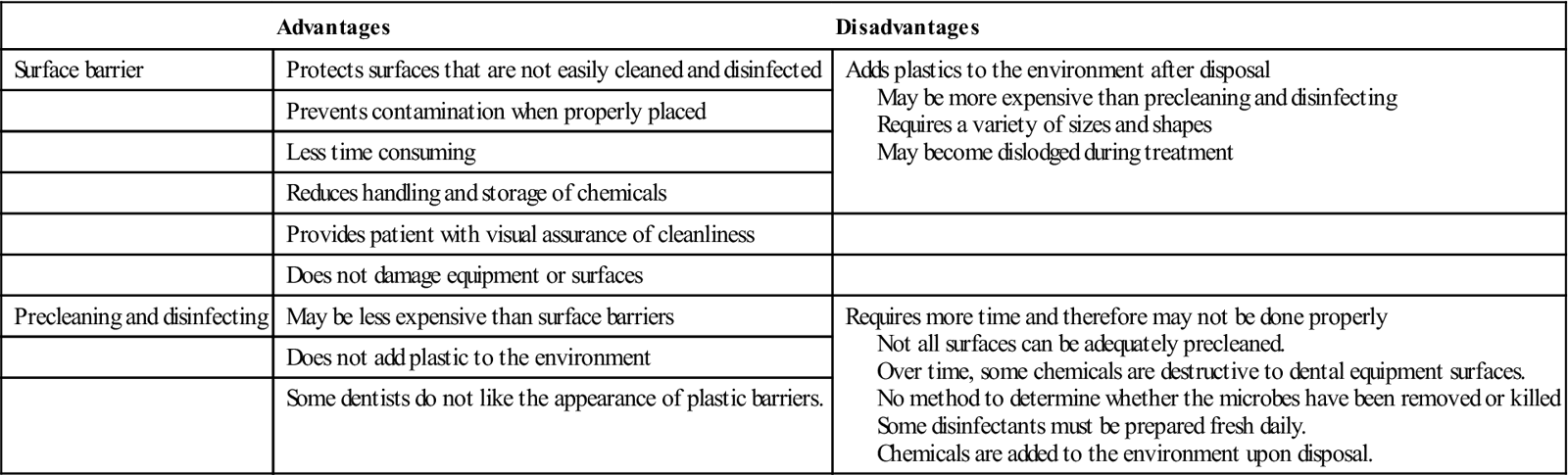
Touch and transfer surfaces should be barrier protected or cleaned and disinfected between patients. Splash, spatter, and droplet surfaces should be cleaned at least once daily (Table 20-1).
TABLE 20-1
Comparison of Surface Barriers and Precleaning/Disinfection
< ?comst?>
| Advantages | Disadvantages | |
| Surface barrier | Protects surfaces that are not easily cleaned and disinfected | Adds plastics to the environment after disposal May be more expensive than precleaning and disinfecting Requires a variety of sizes and shapes May become dislodged during treatment |
| Prevents contamination when properly placed | ||
| Less time consuming | ||
| Reduces handling and storage of chemicals | ||
| Provides patient with visual assurance of cleanliness | ||
| Does not damage equipment or surfaces | ||
| Precleaning and disinfecting | May be less expensive than surface barriers | Requires more time and therefore may not be done properly Not all surfaces can be adequately precleaned. Over time, some chemicals are destructive to dental equipment surfaces. No method to determine whether the microbes have been removed or killed Some disinfectants must be prepared fresh daily. Chemicals are added to the environment upon disposal. |
| Does not add plastic to the environment | ||
| Some dentists do not like the appearance of plastic barriers. |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Surface Contamination
Two methods that may be used to deal with surface contamination are (1) to prevent the surface from becoming contaminated with the use of a surface barrier, and (2) to preclean and disinfect the surface between patients. Each has advantages and disadvantages, and most dental offices use a combination of surface disinfection and surface barriers.
Smooth, hard surfaces such as countertops, handles, supply containers, and bottles can be quickly and easily cleaned (Fig. 20-2). Surfaces with crevices, knobs, or other difficult-to-clean features, such as light handles, air-water syringe handles, and electrical switches (which can short-circuit), are better protected with surface barriers.
It is the responsibility of the dental assistant to make certain that equipment and treatment room surfaces are properly managed to prevent patient-to-patient disease transmission.
Surface Barriers
Placing barriers on surfaces and equipment can prevent contamination of clinical contact areas, but barriers are especially important for those areas that are difficult to clean.
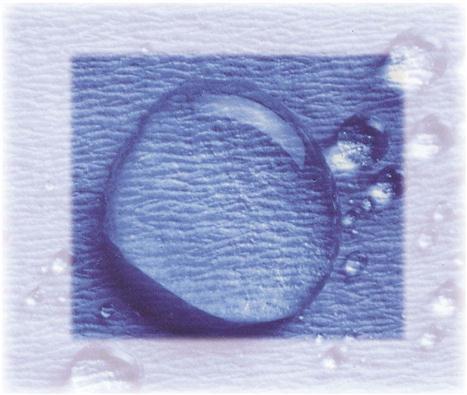
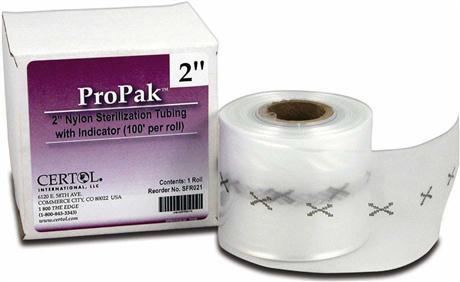
All surface barriers currently on the market should be resistant to fluids. Fluid-resistant barriers prevent microorganisms in saliva, blood, and other liquids from soaking through the barrier material to contact the surface underneath (Fig. 20-3). Some plastic bags are specially designed to fit the shapes of dental chairs, air-water syringes, hoses, pens, and light handles (Fig. 20-4). Other types of barrier materials include clear plastic wrap, bags, tubing, plastic tape, and plastic-backed paper (Figs. 20-5 and 20-6). Sticky tape is frequently used as a plastic barrier to protect smooth surfaces, such as touch pads on equipment or electrical switches on chairs and x-ray equipment. Aluminum foil can also be used because it is easily formed around any shape. Procedure 20-1 reviews the steps to be followed in placing and removing barriers.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses