Ulcerative Conditions
An ulcer is defined simply as loss of epithelium. Ulcers that are preceded by blisters (vesicles or bullae) represent a distinct set of oral conditions, which are discussed in Chapter 1. Ulcerative lesions are commonly encountered in dental patients. Although many oral ulcers have similar clinical appearances, their etiologies encompass many disorders, including reactive, infectious, immunologic, and neoplastic diseases.
Reactive Lesions
Traumatic Ulcerations
Etiology
Ulcers are the most common oral soft tissue lesions. Most are caused by simple mechanical trauma, and a cause-and-effect relationship is usually obvious. Many are a result of accidental trauma and generally appear in regions that are readily trapped or abraded between the teeth, such as the lower lip, tongue, and buccal mucosa. A traumatic ulcer in the anterior portion of the tongue of infants with natal teeth is known as Riga-Fede disease. Prostheses, most commonly dentures, are frequently associated with traumatic ulcers, which may be acute or chronic.
In unusual circumstances, lesions may be self-induced because of an abnormal habit, and in these circumstances there is some psychological problem. These so-called factitial injuries are often as difficult to diagnose as they are to treat. They may prove to be frustrating clinical problems, especially if there is no clinical suspicion of a self-induced cause. Psychological counseling may ultimately be required to help resolve the problem.
Traumatic oral ulcers may also be iatrogenic (induced inadvertently by a health care practitioner, by medical treatment, or by diagnostic procedures). Naturally, respect for the fragility of oral soft tissues is of paramount importance in the treatment of dental patients. Overzealous tissue manipulation or concentration on treating primarily hard tissues may result in accidental, and avoidable, soft tissue injury. Ulcers induced by the removal of adherent cotton rolls, by the negative pressure of a saliva ejector, or by accidental striking of mucosa with rotary instruments are uncommon but entirely preventable.
Chemicals may also cause oral ulcers because of their acidity or alkalinity, or because of their ability to act as local irritants or contact allergens. These may be patient induced or iatrogenic. Aspirin burns are still seen, although they are much less common than in the past. When acetylsalicylic acid is placed inappropriately against mucosa in an attempt by the patient to relieve toothache, a mucosal burn or coagulative necrosis occurs. The extent of injury is dependent on the duration and number of aspirin applications. Many over-the-counter medications for toothache, aphthous ulcers, and denture-related injuries have the ability to damage oral mucosa if used injudiciously. Dental cavity medications, especially those containing phenol, may cause iatrogenic oral ulcers. Tooth-etching agents have been associated with chemical burns of mucosa. Endodontic and vital bleaching procedures, which use strong oxidizing agents such as 30% hydrogen peroxide, have also produced burns.
Intraoral ulcers following heat burns are relatively uncommon intraorally. Pizza burns, caused by hot cheese, have been noted on the palate. Iatrogenic heat burns may also be seen after injudicious use of thermoplastic tooth impression material.
Oral ulcerations are also seen during the course of therapeutic radiation and certain types of chemotherapy for head and neck cancers. In those malignancies—particularly squamous cell carcinoma—that require large (60 to 70 Gy) doses of radiation, oral ulcers are invariably seen in tissues within the path of the beam. Where chemotherapy is a component of treatment, a more widespread ulcer distribution is noted within the oral cavity and oropharynx. For malignancies such as lymphoma, in which lower (40 to 50 Gy) doses are tumoricidal, ulcers are likely but are less severe and of shorter duration. Radiation-induced ulcers persist throughout the course of therapy and for several weeks afterward. If the ulcers are kept clean, spontaneous healing occurs without scarring. The etiology of ulceration and mucositis is related to many factors and involves five biological phases: initiation, primary damage response, signal amplification, ulceration, and healing. The destructive tissue effects are related to the release of active biomolecules secondary to treatment that in turn induce a cascade of inter-related events affecting the extent of damage and repair.
Clinical Features
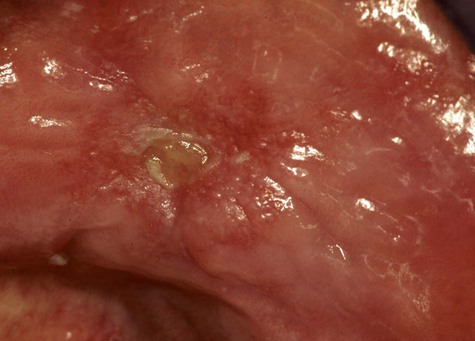
Acute reactive ulcers of oral mucous membranes exhibit the clinical signs and symptoms of acute inflammation, including variable degrees of pain, redness, and swelling (Box 2-1; Figures 2-1 to 2-7). The ulcers are covered by a yellow-white fibrinous exudate and are surrounded by an erythematous halo.



Chronic reactive ulcers may cause little or no pain. They are covered by a yellow membrane and are surrounded by elevated margins that may show hyperkeratosis. Induration, often associated with these lesions, is due to scar formation and chronic inflammatory cell infiltration.
Mucosal ulceration related to cancer management usually begins at approximately 10 days following initiation of radiation (at 20 to 30 Gy) and /or chemotherapy. With radiation, lesions are noted at all sites through which radiation passes, but with chemotherapy, lesions are seen predominantly in movable mucosa (buccal mucosa, lateral and ventral tongue, soft palate and oropharynx).
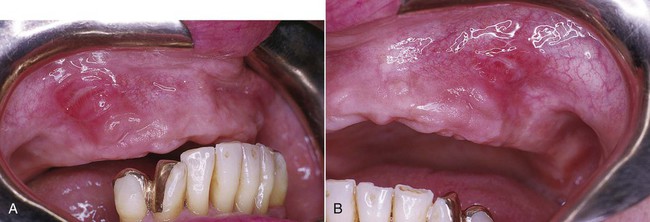
A particularly ominous-appearing but benign chronic ulcer known as traumatic granuloma (traumatic ulcerative granuloma with stromal eosinophilia) occasionally may be seen in association with deep mucosal injury (Figure 2-8). This crateriform ulcer may measure 1 to 2 cm in diameter, and healing may take several weeks to a few months. It is usually found in the tongue with an associated inflammatory infiltrate rich in eosinophils and a subpopulation of CD30+ T lymphocytes.
Another ominous-appearing chronic ulcer, characteristically seen in the hard palate, is known as necrotizing sialometaplasia. It is associated with trauma-induced ischemic necrosis of a minor salivary gland and heals spontaneously in several weeks (see Chapter 8).
Histopathology
Acute ulcers show loss of surface epithelium that is replaced by a fibrin network containing predominantly neutrophils (Figure 2-9). The ulcer base contains dilated capillaries and, over time, granulation tissue. Regeneration of the epithelium begins at the ulcer margins, with proliferating cells moving over the granulation tissue base and under the fibrin clot.
Chronic ulcers have a granulation tissue base, with scar found deeper in the tissue. A mixed inflammatory cell infiltrate is seen throughout. Epithelial regeneration occasionally may not occur because of continued trauma or because of unfavorable local tissue factors. It has been speculated that these factors are related to inappropriate adhesion molecule expression (integrins) and/or inadequate extracellular matrix receptors for the keratinocyte integrins. In traumatic granulomas, tissue injury and inflammation extend into subjacent skeletal muscle. Here a characteristic dense macrophage infiltrate with eosinophils may dominate the histologic picture. The term granuloma as used here reflects the large numbers of macrophages that dominate the infiltrate, but this is not a typical granuloma as seen in an infectious process, such as tuberculosis.
Diagnosis
With acute reactive ulcers, the cause-and-effect relationship is usually apparent from the clinical examination and history. When there is a factitial etiology, diagnosis becomes a challenge.
The cause of chronic reactive ulcers may not be as readily apparent. In this circumstance, it is important that a differential diagnosis be developed. Conditions to consider are infection (syphilis, tuberculosis, deep fungal infection) and malignancy. If the lesion is strongly suspected to be of traumatic origin, the cause should be sought. A 2-week observation period is warranted, together with an effort to keep the mouth clean using a bland mouth rinse such as sodium bicarbonate in water. If no change is seen, or if the lesion increases in size, a biopsy should be performed.
Treatment
Most reactive ulcers of oral mucous membranes are simply observed. If pain is considerable, topical treatment may be beneficial, such as in the form of a topical corticosteroid. Healing of traumatic granuloma is spontaneous, but topical and intralesional steroids can accelerate healing and reduce symptoms.
Bacterial Infections
Syphilis
Syphilis is a sexually transmitted disease that was virtually incurable until Dr. Paul Ehrlich developed his “magic bullet,” arsphenamine, around the turn of the twentieth century. A stunning change in the control of syphilis followed the introduction of penicillin in the early 1940s. By then, approximately 600,000 new cases were reported annually in the United States; during the next 15 years, the rate declined to 6000 cases per year. An increase in the number of new cases (peaking at about 50,000 in 1990), due in part to an association with human immunodeficiency virus (HIV) infection and drug abuse, followed until today, when there seems to be some measure of control of this disease. A significant number of new cases of syphilis are reported in gay men, having a strong association with HIV coinfection and high-risk sexual behavior. In cases with concurrent HIV disease, an atypical clinical course may be noted, including more severe constitutional symptoms, necrotic cutaneous ulcerations, organ and ocular involvement, and a greater tendency to develop neurosyphilis.
Etiology and Pathogenesis
Syphilis is caused by the spirochete Treponema pallidum (Figure 2-10). It is acquired by sexual contact with a partner with active lesions, by transfusion of infected blood, or by transplacental inoculation of the fetus by an infected mother.
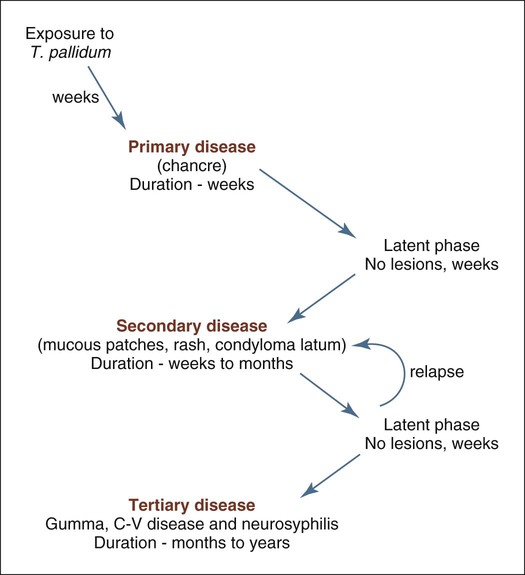
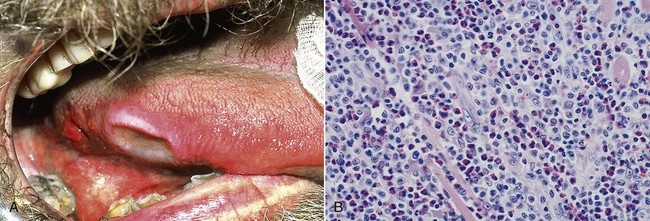
When the disease is spread through direct contact, a hard ulcer, or chancre, forms at the site of spirochete entry (Box 2-2). The ulceration is typically deep with a red, brown, or purple base and an irregular raised border, with resemblance to a chronic traumatic ulcer, squamous cell carcinoma, and non-Hodgkin’s lymphoma. Later, a painless, nonsuppurative regional lymphadenopathy develops. The chancre heals spontaneously after several weeks without treatment, leaving the patient with no apparent signs of disease. After a latent period of several weeks, secondary syphilis develops (patients infected via transfusion bypass the primary stage and begin with secondary syphilis) as a result of hematogenous spread of the spirochete. This stage is marked by a spirochetemia with wide dissemination. Fever, flulike symptoms, mucocutaneous lesions, and lymphadenopathy are typical. In secondary disease, oral lesions are rarely deeply ulcerated, but rather show mucoid exudate (mucous patches). At the labial commissures, split papules may form, while lateral tongue lesions may manifest as deep fissures. This stage also resolves spontaneously, and the patient enters another latency period. Relapses to secondary syphilis may occur in some patients. In about one third of those who have entered the latency phase and have not been treated, tertiary, or late-stage, syphilis develops. These patients may have central nervous system (CNS) involvement, cardiovascular lesions, or focal necrotic inflammatory lesions, known as gummas, of any organ.
Congenital syphilis occurs during the latter half of pregnancy, when the T. pallidum organism crosses the placenta from the infected mother. The spirochetemia that develops in the fetus may cause numerous inflammatory and destructive lesions in various fetal organs, or it may cause abortion.
Clinical Features
Primary syphilis results in painless indurated ulcer(s) with rolled margins at the site of inoculation (Box 2-3; Figures 2-11 to 2-15). The lesion does not produce an exudate. The location is usually on the genitalia. Depending on the site of primary infection, lip, oral, and finger lesions also occur and exhibit similar clinical features. Regional lymphadenopathy, typified by firm, painless swelling, is also part of the clinical picture. The lesion heals without therapy in 3 to 12 weeks, with little or no scarring.
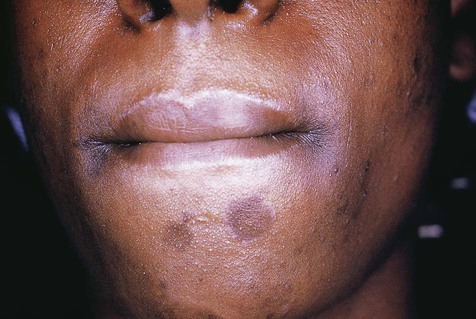
Cutaneous macular lesions.

In untreated syphilis, secondary disease begins after about 2 to 10 weeks. The spirochetes are now disseminated widely and are the cause of a reddish brown maculopapular cutaneous rash and mucosal ulcers covered by a mucoid exudate (mucous patches). Elevated broad-based verrucal plaques, known as condylomata lata, may appear on the skin and mucosal surfaces. Inflammatory lesions may occur in any organ during secondary syphilis.
Manifestations of tertiary syphilis take many years to appear and can be profound, because there is a predilection for the cardiovascular system and the CNS. Fortunately, this stage of syphilis has become a rarity because of effective antibiotic treatment. In untreated disease, approximately one third of patients progress into a tertiary stage.
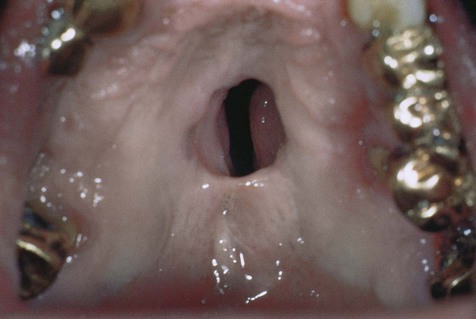
Manifestations of neural syphilis include general paresis (paralysis) and tabes dorsalis (locomotor ataxia). Inflammatory involvement of the cardiovascular system, especially the aorta, may result in aneurysms. Focal granulomatous lesions (gummas) may involve any organ. Intraorally, the palate is typically affected, which can lead to palatal perforation. Development of generalized glossitis with mucosal atrophy has been well documented in the tertiary stage of this disease. Although patients with so-called syphilitic or luetic glossitis are thought to have an approximately fourfold increased risk of oral squamous cell carcinoma, it is unclear whether this is a result of the disease, or whether it is due to the carcinogenic agents that were formerly used to treat the condition, such as arsenicals and heavy metals.
The generalized spirochetemia of congenital syphilis may result in numerous clinical manifestations that may affect any organ system in a developing fetus. A mucocutaneous rash may be seen early. When the infectious process involves the vomer, a nasal deformity known as saddle nose develops; when periostitis of the tibia occurs, excessive anterior bone growth results in a deformity known as saber shin. Other late stigmata of congenital syphilis include conditions known collectively as Hutchinson’s triad: (1) an inflammatory reaction in the cornea (interstitial keratitis), (2) eighth-nerve deafness, and (3) dental abnormalities consisting of notched or screwdriver-shaped incisors and mulberry molars, presumably occurring because of spirochete infection of the enamel organ of teeth during amelogenesis.
Histopathology
The basic tissue response to T. pallidum infection consists of a proliferative endarteritis and infiltration of plasma cells. Endothelial cells proliferate within small arteries and arterioles, producing a concentric layering of cells, which results in a narrowed lumen. Plasma cells, along with lymphocytes and macrophages, are typically found in a perivascular distribution. Spirochetes can be demonstrated in the tissues of various lesions of syphilis using silver stains, although they may be scant in tertiary lesions. Gummas may show necrosis and greater numbers of macrophages, resulting in a granulomatous lesion that is similar to other conditions, such as tuberculosis (TB).
Differential Diagnosis
Clinically, as well as microscopically, syphilis is said to be the great imitator or mimicker because of its resemblance to many other unrelated conditions. When it presents within the mouth, the chancre may be confused with and must be differentiated from squamous cell carcinoma, chronic traumatic lesions, and other infectious diseases, such as TB and histoplasmosis. The differential diagnosis of secondary syphilis would include many infectious and noninfectious conditions marked by a mucocutaneous eruption. Palatal gummas, although rarely seen, may have a clinical appearance similar to the destructive lesions of NK/T-cell lymphoma.
Definitive diagnosis of syphilis is based on laboratory test confirmation of the clinical impression. Among several tests available are (1) darkfield examination of scrapings or exudate from active lesions; (2) special silver stain or immunologic preparation of biopsy tissue; (3) serologic tests for antibodies to T. pallidum, such as the Venereal Disease Research Laboratory test (VDRL), rapid plasmin reagin (RPR), and the enzyme-linked immunosorbent assay (ELISA); and (4) direct fluorescence microscopy of lesional tissue with fluorescein-labeled anti-Treponema serum.
Gonorrhea
Etiology
Gonorrhea is one of the most prevalent bacterial diseases in humans. It is caused by the gram-negative diplococcus Neisseria gonorrhoeae, which infects columnar epithelium of the lower genital tract, rectum, pharynx, and eyes. Infection is transmitted by direct sexual contact with an infected partner. Containment of the spread of infection in sexual partners is enhanced by the short incubation period of less than 7 days, permitting contact tracing, but is hampered by the absence of symptoms in many individuals, especially females.
Genital infections may be transmitted to the oral or pharyngeal mucous membranes through orogenital contact. Pharyngeal mucosa is more likely to be infected than oral mucosa because of the type of epithelium and its reduced resistance to trauma, with pharyngitis as the chief complaint. Developing this form of disease is apparently much more likely with fellatio than with cunnilingus. Individuals may have concomitant genital and oral or pharyngeal infections that result from direct exposure to these areas rather than from being spread through blood or lymphatics.
Transmission of gonorrhea from an infected patient to dental personnel is regarded as highly unlikely because the organism is very sensitive to drying and requires a break in the skin or mucosa to establish an infection. Gloves, protective eyewear, and a mask should provide adequate protection from accidental transmission.
Clinical Features
No specific clinical signs have been consistently associated with oral gonorrhea. However, multiple ulcerations and generalized erythema have been described. Symptoms range from none to generalized stomatitis.
In the more common pharyngeal gonococcal infection, presenting signs are usually seen as general erythema with associated ulcers and cervical lymphadenopathy. The chief complaint may be sore throat, although many patients are asymptomatic.
Differential Diagnosis
Because of the lack of consistent and distinctive oral lesions, other conditions that cause multiple ulcers or generalized erythema should be included in a differential diagnosis. Aphthous ulcers, herpetic ulcers, erythema multiforme, pemphigus, pemphigoid, drug eruptions, and streptococcal infection should be considered. Diagnosis of gonorrhea is traditionally based on demonstration of the organism with Gram stain or culture on Thayer-Martin medium. Rapid identification of N. gonorrhoeae with immunofluorescent antibody techniques and other laboratory tests may be used to support clinical impressions.
Treatment
Uncomplicated gonorrhea responds to a single dose of appropriately selected antibiotic. In the West, infections are susceptible to penicillins and treatment is effective with a single parenteral dose of 2.0 to 3.5 g of ampicillin. In the Far East and parts of Africa, up to 50% of cases are resistant to penicillins and can be managed with a single 500-mg dose of ciprofloxacin. This regimen is also appropriate for pharyngeal gonorrhea, for which ampicillin is generally ineffective. Concerns have been expressed about the development of gonococcal resistance to antibiotics. Some strains already have been reported to be resistant to cephalosporins and fluoroquinolone, including multidrug-resistant forms. Thus, fewer treatment options are available.
Tuberculosis
Etiology and Pathogenesis
Tuberculosis (TB) infects about one third of the world’s population and kills approximately 3 million people per year, making it one of the most important cause of death in the world. In developed countries, a significant decrease in the incidence of TB has occurred as the result of improvements in living conditions, reductions in overcrowding, and antibiotic use. However, the 1980s saw a re-emergence of significant numbers of cases of TB, many in association with HIV infection and acquired immunodeficiency syndrome (AIDS), in Europe and Africa. In addition, the issue of multidrug resistance has proved to be a growing problem in management of the disease.
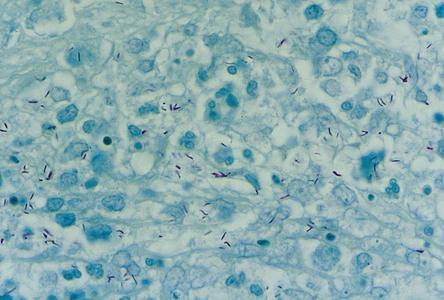
TB is caused by the aerobic, non–spore-forming bacillus Mycobacterium tuberculosis (Figure 2-16). The organism has a thick, waxy coat that does not react with Gram stains but retains the red dyes (Ziehl-Neelsen and Fite techniques). With these stains, the organisms do not decolor with acid-alcohol and therefore are also known as acid-fast bacilli. Two major forms of Mycobacterium are recognized: M. tuberculosis and M. bovis. M. tuberculosis is an airborne infection that is transmitted by inhalation of infected droplets. M. bovis is primarily a disease of cows that is transmitted to humans through infected milk, producing intestinal or tonsillar lesions. Two other closely related forms of Mycobacterium are recognized: M. avium and M. intracellulare. Both are nonvirulent in healthy individuals but cause disseminated disease in immunocompromised individuals, such as those with HIV infection or AIDS.
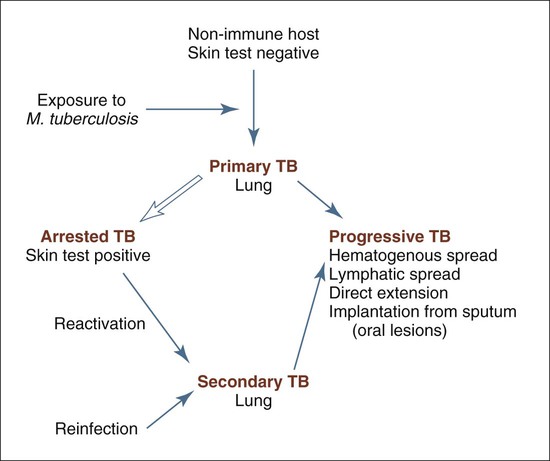
M. tuberculosis infection is spread through small airborne droplets, which carry the organism to pulmonary air spaces. Phagocytosis by alveolar macrophages follows, and the battle between bacterial virulence and host resistance begins. The pathogenicity of M. tuberculosis is due both to its ability to resist degradation by macrophages and to the development of a type IV hypersensitivity reaction. This latter feature explains the destructiveness of lesions in the host tissues and the emergence of drug-resistant strains. As the immune system is sensitized by mycobacterial antigens, positive tuberculin reactivity develops. The Mantoux and tine skin tests, which use a tubercle bacillus antigen called purified protein derivative (PPD), determine whether an individual is hypersensitive to antigen challenge. A positive inflammatory skin reaction indicates that the individual’s cell-mediated immune system has been sensitized and signifies previous exposure and subclinical infection. It does not necessarily imply active disease.
A granulomatous inflammatory response to M. tuberculosis follows sensitization. In most cases, the cell-mediated immune response is able to control the infection, allowing subsequent arrest of the disease. Inflammatory foci eventually may undergo dystrophic calcification, but latent organisms in these foci may become reactivated at a later date. In a small number of cases, the disease may progress through airborne, hematogenous, or lymphatic spread, so-called miliary spread.
Oral mucous membranes may become infected through implantation of organisms found in sputum or, less commonly, through hematogenous deposition. Similar seeding of the oral cavity may follow secondary or reactivated TB.
Clinical Features
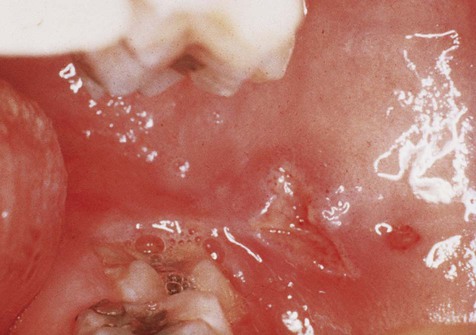
Unless the primary infection becomes progressive, an infected patient will probably exhibit no symptoms (Box 2-4; Figure 2-17). Skin testing and chest radiographs may provide the only indicators of infection. In reactivated disease, low-grade signs and symptoms of fever, night sweats, malaise, and weight loss may appear. With progression, cough, hemoptysis, and chest pain (pleural involvement) occur. As other organs become involved through the spread of organisms, a highly varied clinical picture appears and is dependent on the organs involved.
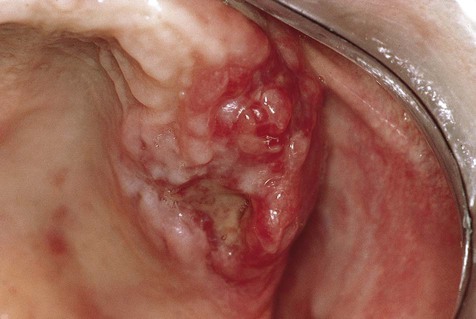
Oral manifestations that usually follow implantation of M. tuberculosis from infected sputum may appear on any mucosal surface. The tongue and the palate are favored locations. The typical lesion is an indurated, chronic, nonhealing ulcer that is usually painful. Bony involvement of the maxilla and mandible may produce tuberculous osteomyelitis. This most likely follows hematogenous spread of the organism. Pharyngeal involvement results in painful ulcers, which may cause dysphagia, odynophagia, and voice changes.
Histopathology
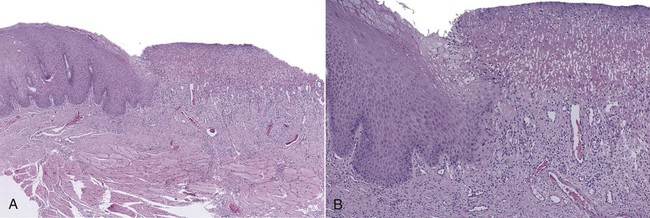
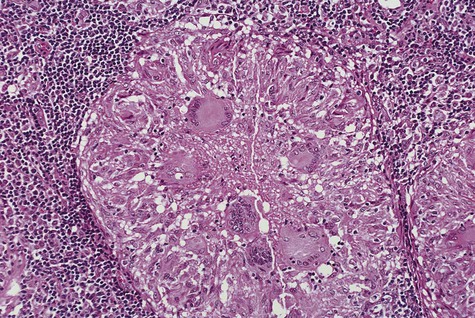
The basic microscopic lesion of TB is granulomatous inflammation, in which granulomas show central caseous necrosis (Figure 2-18). In tissues, M. tuberculosis incites a characteristic macrophage response, in which focal zones of macrophages become surrounded by lymphocytes and fibroblasts. The macrophages develop an abundant eosinophilic cytoplasm, giving them a superficial resemblance to epithelial cells; for this reason, they are frequently called epithelioid cells. Fusion of macrophages results in the appearance of Langerhans giant cells, in which nuclei are distributed around the periphery of the cytoplasm. As the granulomas age, central necrosis occurs; this is usually referred to as caseous necrosis because of the gross cheesy texture of these zones.
A Ziehl-Neelsen or Fite stain must be used to confirm the presence of the organism in the granulomas, because several infectious and noninfectious conditions may produce a similar granulomatous reaction (Figure 2-19). In the absence of acid-fast bacilli, other microscopic considerations would include syphilis, cat-scratch disease, tularemia, histoplasmosis, blastomycosis, coccidioidomycosis, sarcoidosis, and some foreign body reactions, such as those induced by beryllium.
Differential Diagnosis
On the basis of clinical signs and symptoms alone, oral TB cannot be differentiated from several other conditions. A chronic indurated ulcer should prompt the clinician to consider primary syphilis and oral manifestations of deep fungal diseases. Noninfectious processes that should be considered clinically are foreign body reaction, sarcoidosis, Crohn’s disease, orofacial granulomatosis, squamous cell carcinoma, and chronic traumatic ulcer. Major aphthae might be included, although a history of recurrent disease should help separate this condition from the others. In approximately half of cases, the diagnosis or oral manifestation of oral tuberculosis has led to a diagnosis of undiagnosed systemic infection. Rarely, carcinomas may coexist at the same lesion site.
Treatment
First-line drugs likely to be used for treatment of TB include isoniazid, rifampin, pyrazinamide, and ethambutol. Drug combinations are often used in 6-, 9-, or 12-month treatment regimens that may be extended as long as 2 years. Streptomycin is rarely used for first-line treatment except in multidrug-resistant cases. Oral lesions would be expected to resolve with treatment of the patient’s systemic disease. Unfortunately, infection with multidrug-resistant organisms is a serious clinical problem that appears to be on the increase. Development and testing of new classes of drugs are necessary to meet the challenge of resistant organisms.
Patients who convert from a negative to a positive skin test response may benefit from prophylactic chemotherapy, typically using isoniazid for 1 year. This decision is dependent on risk factors involved, such as age and immune status, and on the opinion of the attending physician.
Bacille Calmette-Guérin (BCG) vaccine is effective in controlling childhood TB, but it loses efficacy in adulthood. New vaccines that are under investigation offer hope for at-risk populations.
Leprosy
Etiology and Pathogenesis
Leprosy, also known as Hansen’s disease, is a chronic infectious disease caused by the acid-fast bacillus, Mycobacterium leprae. Worldwide, 20 million individuals are thought to be infected. It is the most common cause of peripheral neuritis in the world. Because the causative organism is difficult to grow in culture, it has been maintained in the footpads of mice and in the armadillo, which has a low core body temperature. Leprosy is only moderately contagious; transmission of the disease requires frequent direct contact with an infected individual for a long period, with an incubation period ranging up to 5 years for the tuberculoid form versus up to 12 years in the lepromatous form of the disease. Inoculation through the respiratory tract is believed to be a potential mode of transmission.
Clinical Features
Oral lesions appear in the lepromatous form of the disease in 20% to 60% of cases as multiple nodules (necrotic and ulcerated) with associated slow healing and atrophic scarring. A clinical spectrum of disease ranges from a limited form (tuberculoid leprosy) in those with a well-functioning immune system, to a generalized form (lepromatous leprosy) in individuals with reduced levels of cell-mediated immune reactivity; the latter has a more seriously damaging course. Generally, skin and peripheral nerves are affected because the organism grows best in temperatures less than the core body temperature of 37° C. Cutaneous lesions appear as erythematous plaques or nodules, representing a granulomatous response to the organism. Similar lesions may occur intraorally or intranasally. In time, severe maxillofacial deformities may appear, producing the classic destruction of the anterior nasal spine and anterior maxillary alveolus, as well as intranasal inflammation and tissue destruction called facies leprosa. Damage to peripheral nerves results in anesthesia, leading to trauma to the extremities and consequent ulceration, as well as bone resorption.
Histopathology
Microscopically, a granulomatous inflammatory response, in which macrophages/epithelioid histiocytes and multinucleated giant cells predominate, is usually seen. Infiltration of nerves by mononuclear inflammatory cells is also noted. Well-formed granulomas, similar to those present in the tissue lesions of TB, are typically seen in tuberculoid leprosy. Poorly formed granulomas with sheets of macrophages reflect the pattern more typical of le/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses