Verrucal-Papillary Lesions
Reactive/Infectious Lesions
Squamous Papilloma/Oral Wart
Oral squamous papilloma (including the vermilion portion of the lip) is the most common papillary lesion of the oral mucosa and accounts for approximately 2.5% of all oral lesions. Similar to verruca vulgaris (warts) on the skin, many oral squamous papillomas have been shown to be associated with the human papillomavirus (HPV). The type of HPV varies, with some cases having the same subtype as cutaneous warts and others having different HPV strains. Whether all oral papillomas are of viral origin is unresolved. It has been shown that the class of HPVs is very large (more than 100 subtypes), and that individually these viruses are associated with many conditions of squamous epithelium. For example, HPV subtypes 2 and 4 have been demonstrated within cutaneous warts; flat warts of the skin have been associated with HPV subtypes 3 and 10. HPV subtype 11 has been found within papillomas of the sinonasal tract and the oral cavity. HPV subtypes 16 and 18 have been related to neoplastic changes of cervical squamous epithelium and to oropharyngeal squamous cell carcinoma (Table 6-1).
TABLE 6-1
LESIONS CAUSED BY HUMAN PAPILLOMAVIRUS SUBTYPES
| Lesion | HPV Subtype |
| Oral papilloma/wart | 2, 6, 11, 57 |
| Focal epithelial hyperplasia | 13, 32 |
| Dysplastic wart (HIV) | 16, 18, others |
| Verruca vulgaris, skin | 2, 4, 40, others |
| Flat wart | 3, 10 |
| Condyloma acuminatum | 6, 11, others |
| Laryngeal papilloma | 11 |
| Conjunctival papilloma | 11 |
HIV, Human immunodeficiency virus; HPV, human papillomavirus.
Clinical Features
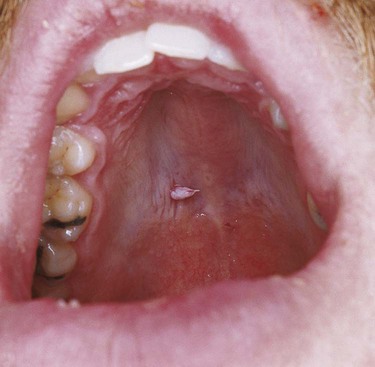
Oral squamous papillomas may be found on the vermilion portion of the lips and on any intraoral mucosal site, with predilection for the hard and soft palate and the uvula (Box 6-1; Figures 6-1 to 6-3). The latter three sites account for approximately one third of all lesions. The lesions generally measure less than 1 cm in greatest dimension and appear as pink to white exophytic granular or cauliflower-like surface alterations. They are generally asymptomatic and solitary in their presentation, although multiple lesions may occur.


Histopathology
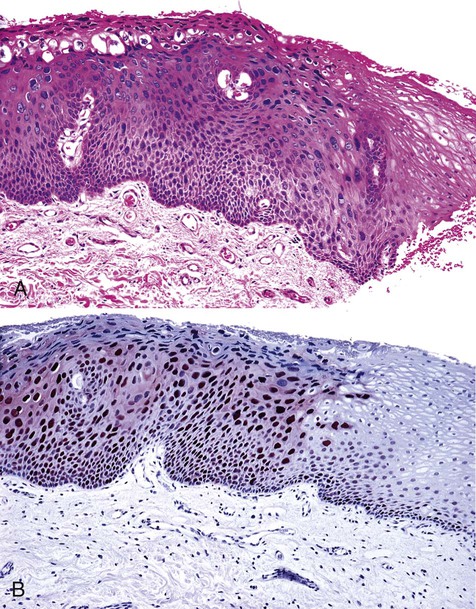
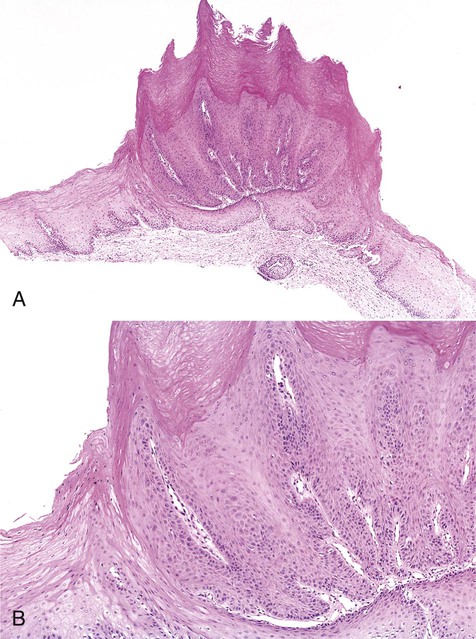
Oral squamous papillomas represent an exaggerated growth of normal squamous epithelium (Figures 6-4 to 6-6). The lesions are exophytic and are composed of finger-like extensions of epithelium, supported by a well-vascularized connective tissue core. The histologic architecture may mimic the pattern of the cutaneous wart. Upper level epithelial cells demonstrate nuclei that are pyknotic (condensed) and crenated, often surrounded by an edematous or optically clear zone, forming the so-called koilocytic cell. In the uterine cervix, this cytologic appearance represents HPV infection, which by extension is generally thought to present in the oral cavity.

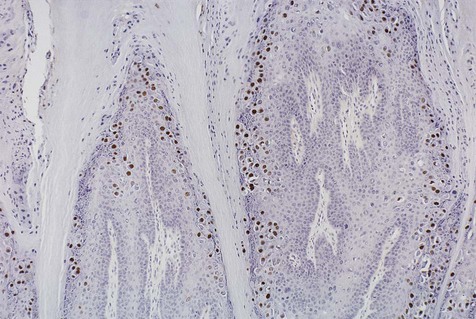
Immunohistochemical stain for common human papillomavirus in an oral wart. Positive, brown-staining nuclei are seen in upper level keratinocytes.
Dysplastic Oral Warts
A small subset of HIV/AIDS patients develop oral warts that exhibit microscopic changes that are dysplastic in appearance (Box 6-2; Figure 6-7). The degree of dysplasia ranges from mild to severe. The outcome, or natural history, of these dysplastic warts is unknown, although invasive carcinoma has yet to be reported despite several years of follow-up. A wide variety of HPV subtypes, including 16 and 18, can be demonstrated in these lesions.
Papillary Hyperplasia
Etiology
Histopathology
On perpendicular cross-section, papillary hyperplasia appears as numerous small fronds or papillary projections covered with intact parakeratotic stratified squamous epithelium (Figure 6-9). The epithelium is supported by hyperplastic central cores of well-vascularized stromal tissue. The epithelium is hyperplastic and often demonstrates pseudoepitheliomatous features, occasionally severe enough to mimic squamous cell carcinoma. No evidence of dysplasia is found in association with this lesion and risk of malignant transformation is not increased.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses