Chapter 2
The Role of Crown-Lengthening Therapy
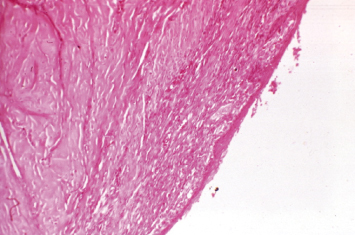
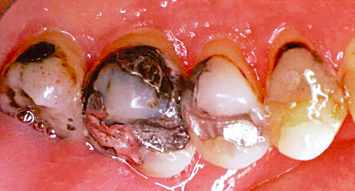
In an effort to deliver high-quality, predictable restorative dentistry to patients, all treating practitioners must consider the dynamic interplay of tooth restoration, the restorative procedure itself, and the health of the surrounding hard and soft tissues. Every restoration, whether it be a Class II amalgam or a full-mouth fixed reconstruction, places added demands on the supporting periodontium (Figs. 2.1, 2.2). The most ideal marginal adaptation results in increased plaque accumulation at the restorative margin-tooth interface. Poorly contoured restorations will inhibit proper plaque control procedures, thus hastening periodontal breakdown and recurrent caries at the restorative margin-tooth interface (Figs. 2.3–2.6). Should such margins be placed subgingivally, the destructive process is accelerated by the inability of the patient to adequately carry out plaque control measures.
Fig. 2.1 Twenty-three years after restoration, a patient presents with a 14-unit maxillary fixed prosthesis supported by two first molars and two cuspids, and a mandibular overdenture retained by two cuspid roots with attachments. Such a successful therapeutic outcome requires an understanding and management of periodontal restorative interrelationships.

Fig. 2.2 Periodontal restorative interrelationships must also be appropriately understood and managed when placing an isolated Class II restoration on a tooth.

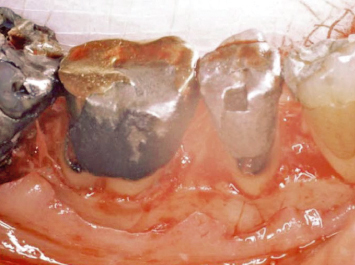
Fig. 2.3 Flap reflection reveals significant plaque and calculus accumulation at the restorative margin tooth interface, where the restoration extended subgingivally.

Fig. 2.4 A poor understanding of the periodontal ramifications of ill fitting restorative dentistry has led to the demise of a first molar. An aluminum shell crown was placed; subsequent decay developed at the restorative margin tooth interface and was repaired with a subgingival amalgam; the situation was not conducive to home-care efforts and continued plaque and calculus accumulation resulted in periodontal bone loss and additional caries on the distal root of the tooth; another restoration was placed, extending deeper subgingival. The net result was loss of the tooth.

Fig. 2.5 A patient presents with older restorations which extend subgingivally. The tissues appear firm and pink. No clinical evidence of inflammation exists.

Fig. 2.6 Flap reflection reveals extensive subgingival caries around all restorations. Note the developing furcation involvement on the first molar, due in large part to the nonideal morphology of the subgingival restoration in the area. Failure to intervene in an appropriate, timely manner has resulted in poor prognoses for these teeth.
While many practitioners speak of the “self-cleansing zone” below the gingival margin, and the maintainability of a subgingival restoration if monitored carefully (1), Waerhaug has shown that even a well-fitting restoration will harbor plaque and bacteria (2).
Several clinical investigators have demonstrated the detrimental effects of poorly finished and/or incorrectly positioned restorations with subgingival margins on the periodontal tissues. Local gingival inflammation and loss of periodontal attachment are the results of such therapy (3–7). It has additionally been demonstrated that it is plaque accumulation in relation to an overhanging restorative margin, and not merely the subgingival restoration, that causes promotion of the periodontal disease process (7–9).
Nowhere is the delicate balance of the restored tooth and the health of the surrounding periodontium more evident than in the restoration of an interproximal area. A multitude of factors—periodontal, restorative, and geometric in nature—work together to render this a primary area of concern in the successful management of any dentition compromised by oral bacteria. To properly manage the embrasure space, the area must be visualized as the fluid, three-dimensional entity it is.
Management of the Apico-occlusal Dimension
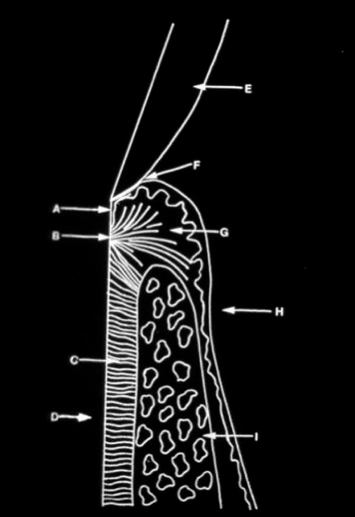
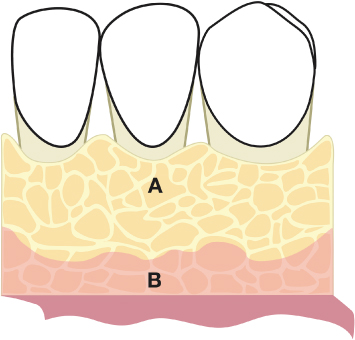
The concept of biologic width is paramount in understanding the apico-occlusal relationship of the restorative margin to the osseous crest. Proceeding coronally from the osseous crest, the attachment apparatus consists of Sharpey fiber insertion into the root surface, followed by a junctional epithelial adhesion to root surface, followed by the gingival sulcus (Fig. 2.7). The combined dimensions of the connective tissue and junctional epithelium are, on average, 2.04 mm in humans (10). Impingement upon this dimension by the restorative margin results in soft-tissue inflammation and eventual periodontal break down. In addition, postsurgical healing of tissues is impaired in the face of a compromised biologic width.
Fig. 2.7 A diagrammatic representation of a healthy attachment apparatus. A = junctional epithelium; B = supracrestal connective tissue insertion; C = periodontal ligament; D = root; E = enamel; F = gingival sulcus; G = gingival connective tissue; H = covering epithelium; I = alveolar bone.
VIOLATING THE BIOLOGIC WIDTH
Violation of the biologic width can occur due to tooth preparation, which may damage the junctional epithelium and the supra-alveolar connective tissues. A progressive inflammatory process may also occur following soft tissue retraction procedures, various impression techniques, electrosurgery (Fig. 2.8), and the placement of a temporary restoration.
Fig. 2.8 Injudicious use of electrosurgery has resulted in irreversible damage to the root surface and the attachment apparatus. Note the inflammatory lesion in the soft tissues, the damaged root cementum, and the loss of periodontal attachment to the tooth.
Fortunately, Löe and Silness have shown that injuries created by insertion of a retraction cord are reversible, as long as the lesions are allowed to heal against a clean tooth surface (11). Duncan (12) found that damage attributed to poorly contoured provisional restorations was reversible, as long as the provisional restorations were modified and placed correctly. However, if inflammation occurs and is not resolved, the inflammatory process is perpetuated when the final restoration is cemented in the previously injured and inflamed area (13). Irreversible damage results, characterized by the development of a periodontal pocket, with apical migration of the junctional epithelium and loss of attachment. Placement of restorations prior to total healing and development of the supracrestal attachment apparatus postsurgically is also highly problematic, as it is impossible to know in advance where the most coronal position of the attachment apparatus will be (Fig. 2.9). The net result is violation of the biologic width, impingement upon the attachment apparatus and development of an inflammatory lesion.
Fig. 2.9 Following periodontal osseous surgery, impressions were taken and full coverage restorations were fabricated and inserted prior to development and maturation of the supracrestal attachment apparatus. Note the inflamed, rolled nature of the marginal soft tissues.

Studies by Fugazzotto and Parma-Benfenati (14) and Parma-Benfenati et al. (15) examined the effects of restorative margin positions on the development and health of the supracrestal attachment apparatus postsurgically, as well as the role that quantity and quality of alveolar housing played in such attachment apparatus development. At the control sites, Class V amalgam restorations were placed 4 mm coronal to the osseous crest in beagle dogs, and the teeth were notched at the osseous crest. In the experimental sites, Class V amalgam restorations were placed at osseous crest.
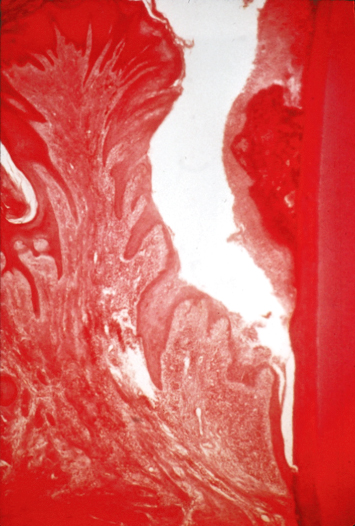
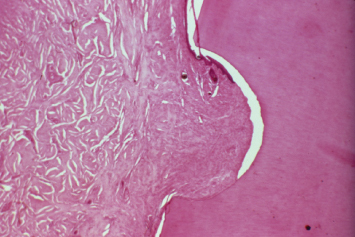
Histological examination 12 weeks post-therapy underscored the effects of restorative margin position on postsurgical attachment apparatus development. At the control sites, all tissues healed uneventfully. Histologic specimens were characterized by connective tissue reattachment to the root surface supracrestally for approximately 1 mm, followed by 1–1.5 mm of junctional epithelial adhesion. Minimal alveolar bone crest resorption was evident (Figs. 2.10, 2.11). This crestal resorption was more pronounced in specimens where thinner preoperative bone had been present.
Fig. 2.10 In control sites, an amalgam restoration was placed at least 4 mm coronal to the crestal bone, and the root surface was notched at the crestal bone at the time of periodontal flap surgery. A 12-week postoperative histologic specimen demonstrates no signs of inflammation, and a healthy periodontal attachment apparatus crestal to the alveolar bone.
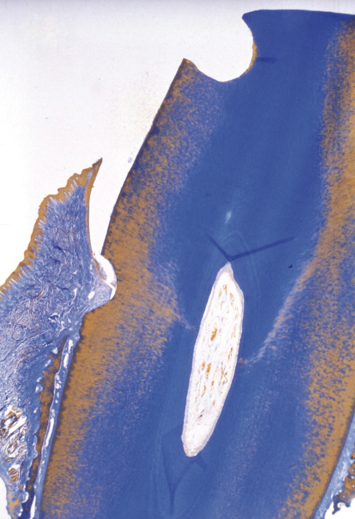
Fig. 2.11 A close-up of the notched area of the root demonstrates connective tissue attachment and a lack of inflammatory cells in control sites.
In the experimental sites, the tissues coronal to the restoration were characterized by a thin atrophic epithelial lining, which was not attached to the root surface, and a localized inflammatory reaction in the gingival soft tissues. This epithelium extended slightly apical to the restoration (Figs. 2.12–2.14). In all histological specimens of experimental sites, bone resorption was present to a varying degree, depending upon the quantity and quality of the preoperative bony septum. Thinner preoperative septa demonstrated greater loss of bone height than their thicker counterparts. Connective tissue attachment to the root surface always occurred apical to the restoration following the bone loss.
Fig. 2.12 In experimental sites, a restoration was placed at the alveolar crest during periodontal flap surgery. A 12-week histologic specimen demonstrates significant loss of alveolar crest height, apical positioning of the connective tissue insertion into the root, and ulcerated, inflamed tissues over the restoration.
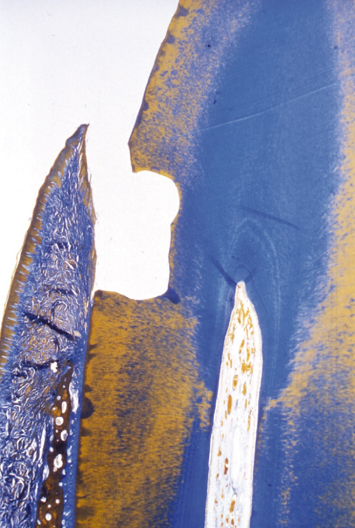
Fig. 2.13 The epithelium is thin or nonexistent in the experimental site. A heavy inflammatory infiltrate is noted in the gingival connective tissue.
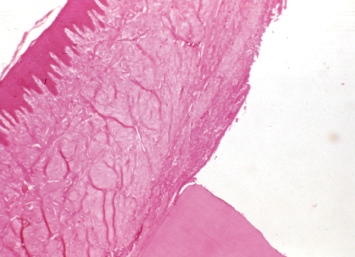
Fig. 2.14 A close-up demonstrates the ulcerated epithelium in the area of the restoration. Note the significant inflammatory infiltrate in the gingival connective tissue.
Clinically, the healed tissues in the control sites appeared healthy and did not bleed upon probing. The postoperative tissues at the experimental sites demonstrated significant clinical inflammation and bleeding upon probing.
The study demonstrated that:
1. Following surgical intervention, osseous resorption occurs. This pattern of resorption is influenced by the preoperative bone morphology.
2. When the biologic width is violated, inflammation not only will result in osseous resorption in an attempt to afford space for connective tissue insertion into the root supracrestally, but also will perpetuate the ongoing pathological process.
3. The presence of subgingival restorations will result in greater plaque accumulation.
4. Histologically, the findings adjacent to a subgingival restoration will correspond to those encountered when examining an inflammatory periodontal lesion.
5. When a restoration impinges upon the needed dimensions for development of the attachment apparatus during healing after periodontal surgical therapy, the extent of osseous loss encountered will be greater than when such a compromise is not present.
6. When a subgingival restoration is present, the inflammatory lesion encountered in the healed periodontal tissues postsurgically will be walled off by the establishment of a new “dentoperiosteal” fiber system. This “dentoperiosteal” fiber system will be more apical than it would be if the restoration were not present, and will occur in the presence of greater loss of osseous structures crestally.
In light of the fact that a continuing inflammatory lesion is present when a subgingival restoration exists that impinges upon the necessary dimensions for reestablishment of a healthy attachment apparatus postsurgically, and because this attachment apparatus will establish itself regardless of osseous loss, crown-lengthening procedures to establish adequate biologic width to ensure that restorations are not placed too close to the osseous crest are usually justifiable.
In situations where the septa consisted of both thin and thick components, the thinner portions of the septa were resorbed to a greater extent. These findings are in agreement with widely accepted understanding regarding postsurgical periodontal healing. Ruben et al. (16) postulated that thinner septa would demonstrate greater liability than their thicker counterparts due to their biological and histological characteristics. Thin bony septa predominantly consist of cortical plates with a small marrow component. As a result, such septa are deficient in their primary source of pluripotential cells, which have the ability to differentiate into blastic cells of both hard- and soft-tissue natures. Thus, the osteogenic reaction expected following initial postsurgical resorption is attenuated or absent altogether in the presence of thin osseous septa. The initial resorptive phase itself may often be enough to eliminate a thin osseous septum because of its buccolingual dimension.
Parma-Benfenati et al. (14,16) found this to be the case in most of the thin septal specimens examined. The osseous septum began to resorb progressively from the external aspect of the septum inward (i.e., from the periosteal aspect toward the periodontal ligament). Simultaneously, resorption occurred from its thin coronal aspects. As the septum resorbed in the presence of the postsurgical chronic inflammatory process which is associated with any surgical procedure, the bone was replaced by connective tissues. These connective tissues served to join the periosteum with the remaining components of the periodontal ligament, which remained inserted into the cementum of the tooth (17).
When thicker bony septa had been present preoperatively, the biological and histological characteristics of the postoperative bone, and hence the postoperative results, were markedly different. Thicker septa contain greater amounts of marrow components than their thinner counterparts, and are thus capable of a more exuberant osteogenic response to surgical insult. When the cortical plate is resorbed, a pluripotential cell population is unmasked, yielding the expected result of new bone and other tissues. A highly exaggerated initial resorptive phase would be necessary to result in the obliteration of a thick bony septum. As a result, significantly less occluso-apical osseous loss was found when thick bony septa were present preoperatively, as compared to thin bony septa specimens.
Prior to the work of Parma-Benfenati et al. (14,15), no well-controlled clinical or histological studies had been performed that compared the extent and pattern of osseous resorption following a given surgical procedure in a thin septal scenario to that of a thicker septal scenario. Authors had discussed these considerations following gingival autograft placement (18,19). Friedman has shown that 0.5 mm of osseous resorption occurred during healing following osseous resective surgery when a thick bone septum was present, but did not compare his findings to those when a thin bony septum was present presurgically (20).
CROWN-LENGTHENING SURGERY
Although specific instances exist where nothing more than recontouring of the soft tissues is necessary to affect appropriate crown-lengthening osseous surgery, such a clinical scenario is infrequent. Rather, osseous resective therapy is usually required, in conjunction with appropriate soft-tissue management, to expose the desired clinical crown, ensure the development of an appropriate post-therapeutic attachment apparatus, and help establish the most ideal milieu for reception of the planned restorative dentistry.
CLINICAL EXAMPLE ONE
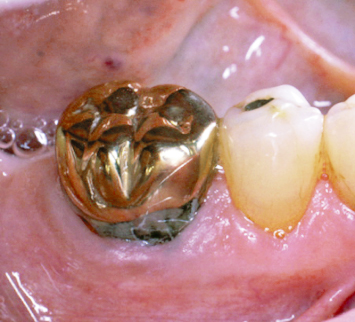
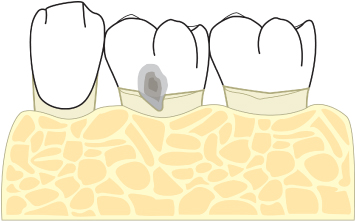
A patient presents with subgingival recurrent caries around an amalgam “patch” which had previously been placed to treat recurrent caries around a gold crown. The amalgam restoration extends deep subgingival (Fig. 2.15).
Fig. 2.15 A patient presents with recurrent subgingival caries around an amalgam “patch” on a first molar.
Flap reflection demonstrates the nonideal contours of the amalgam patch that had previously been placed (Fig. 2.16). Note the recurrent caries on the distal aspect of the subgingival extension of the amalgam patch, and the plaque trap that has been created in the furcation area. Failure to intervene appropriately would result in a poor prognosis for the first molar. Following recontouring of the amalgam restoration to eliminate its nonideal contours and appropriate osseous resective therapy, the buccal mucoperiosteal flap is sutured at osseous crest with interrupted gut 4-0 silk sutures (Fig. 2.17). Eight weeks postoperatively, the tissues have healed well, there is no evidence of a buccal furcation involvement, and the recurrent caries is exposed and accessible for appropriate restoration and subsequent patient plaque control measures (Fig. 2.18).
Fig. 2.16 Following flap reflection, recurrent caries around the amalgam restoration is evident. Note the “furcation involvement” due to the inability to appropriately contour the amalgam restoration deep subgingivally.
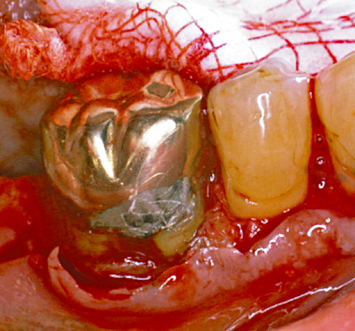
Fig. 2.17 Following appropriate osseous crown-lengthening surgery and reshaping of the amalgam restoration, the flaps are sutured at osseous crest with interrupted silk sutures.
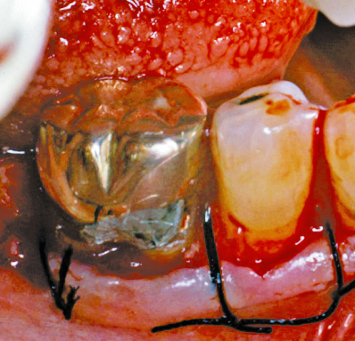
Fig. 2.18 All caries and older restorations are supragingival and accessible for appropriate restorative intervention following healing.

CLINICAL EXAMPLE TWO
A patient presents with numerous older subgingival restorations and recurrent subgingival caries on the mesiopalatal aspect of the maxillary first molar, and the palatal aspect of the maxillary first premolar (Fig. 2.19). Following appropriate flap design and reflection, including thinning and crestal anticipation of the palatal mucoperiosteal flap followed by the necessary osseous resective therapy, the buccal and palatal mucoperiosteal flaps are sutured at osseous crest with interrupted 4-0 silk sutures (Fig. 2.20). Eight weeks postoperatively, all subgingival restorations and/or recurrent caries are exposed and accessible for both appropriate restorative intervention and subsequent patient plaque-control efforts (Fig. 2.21).
Fig. 2.19 A patient presents with older restorations, recurrent subgingival caries on the mesial palatal aspect of the maxillary first molar, and recurrent caries on the palatal aspect of the first premolar.

Fig. 2.20 Note the position of the palatal soft tissues following appropriate flap design and reflection, including crestal anticipation, osseous resection, and suturing with interrupted 4-0 silk sutures.
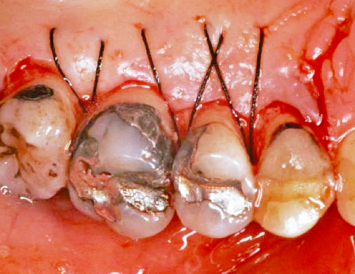
Fig. 2.21 Following appropriate crown-lengthening osseous surgery, all recurrent caries and older restorations are accessible for restorative intervention.
CLINICAL EXAMPLE THREE
A patient presents with a temporary full coverage restoration on the maxillary second premolar. Following removal of the temporary restoration, inadequate clinical crown length is present for appropriate restorative intervention. Crown-lengthening osseous surgery is performed in the manner already described, exposing adequate tooth structure and establishing biologic width. Following healing, the soft-tissue margin of the crown-lengthened tooth and the adjacent teeth are confluent and easily cleansable. More than adequate tooth structure is now exposed for appropriate restorative intervention (Figs. 2.22–2.24).
Fig. 2.22 A patient presents with a provisional restoration on the maxillary second premolar. Note the inflamed nature of the surrounding soft tissues.

Fig. 2.23 Following removal of the provisional restoration, it is obvious that inadequate clinical tooth structure is present for appropriate reception of restorative therapy. Note the inflamed and nonideally shaped interproximal soft tissues.

Fig. 2.24 Crown-lengthening osseous surgery has been performed, and the buccal and palatal flaps have been sutured at the alveolar osseous crest with interrupted plain gut sutures.

CLINICAL EXAMPLE FOUR
A patient presents with marked incomplete passive eruption and a problem with retention of the final full coverage restorations on her maxillary first and second premolars. Incomplete passive eruption will be subsequently discussed. The restorative dentist has attempted to improve retention of the restorations utilizing various permutations of grooves and pins in the prepared teeth. Periodontal crown-lengthening osseous surgery is carried out in the previously described manner, eliminating the incomplete passive eruption that is present and exposing adequate tooth structure for fabrication of restorations with ideal contours and the necessary retention. Following healing, more than adequate tooth structure is exposed for such therapeutic intervention. The final restorations demonstrate the desired restorative contours. No problem has been encountered with the retention of the final restorations (Figs. 2.25–2.28).
Fig. 2.25 A patient presents with final restorations on the maxillary first and second premolars. These restorations continue to dislodge. Note the incomplete passive eruption that is present.

Fig. 2.26 Following crown-lengthening osseous surgery, adequate tooth structure is exposed for appropriate restorative intervention, and a more ideal gingival margin position has been attained. Note the unprepared enamel that was subgingival on the second premolar, due to the incomplete passive eruption that was present.

Fig. 2.27 Approximately 4 weeks post-therapy, the soft tissues have healed at the desired levels.

Fig. 2.28 Following final restoration, ideal, acceptable crown contours and gingival margin levels are evident. There were no retention problems with the final restorations.

All too often, a discussion of crown-lengthening osseous surgery focuses immediately and almost exclusively upon osseous resection to establish the desired dimension between the alveolar crest and the planned restorative margin. Such focus, with the exclusion of other considerations, is ill-advised. Any comprehensive discussion of the technical aspects of crown-lengthening surgery must begin with enumeration of the various components of appropriate soft-tissue flap design.
Incision Design
INITIAL INCISION
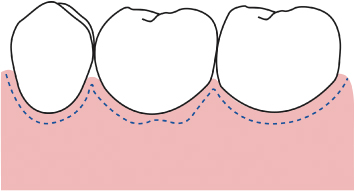
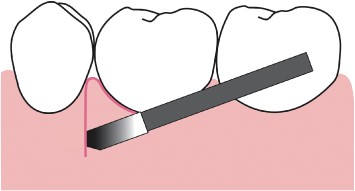
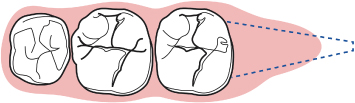
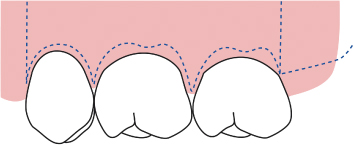
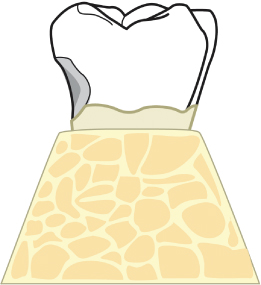
Either an intrasulcular or subsulcular buccal incision is employed, which extends at least one tooth mesial and distal of the tooth to be crown lengthened. If an intrasulcular incision is utilized, a 15 blade is angled in such a manner as to remove the sulcular epithelium. The incision is carried to osseous crest, with care being taken to scallop the buccal incision appropriately. In the case of a single-rooted tooth, the incision is scalloped so that long interproximal papillae are created. The buccal aspect of the incision mimics the ideal scallop of the buccal bone in health (Figs. 2.29, 2.30). As such, the slope and width of the scallop will vary from tooth to tooth. When an incision is made on the buccal aspect of a multirooted tooth, the incision is scalloped in such a way as to mimic the ideal scallop of the buccal alveolar bone, thus creating a “furcal papilla” (Figs. 2.31, 2.32).
Fig. 2.29 A presurgical diagrammatic representation of a mandibular premolar area.
Fig. 2.30 The parabolae of the initial subsulcular incision mimic the contours of ideally scalloped buccal alveolar bone.
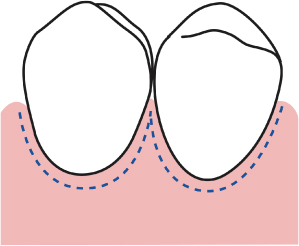
Fig. 2.31 A presurgical diagrammatic representation of a mandibular molar and premolar region.
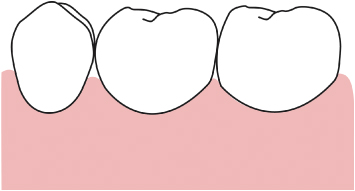
Fig. 2.32 Once again, the outline of the initial subsulcular incision mimics the ideal scallop of the buccal bone in health. Note the “double parabola” created in the furcation area.
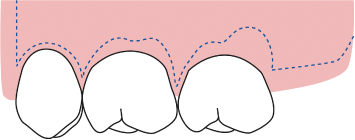
If adequate keratinized tissue is present on the buccal aspects of the teeth to be treated, the initial incision is placed subsulcularly, taking care to leave at least 3 mm of keratinized tissue between the incision and the mucogingival junction.
RELEASING INCISIONS
Mesial and distal releasing incisions are placed in such a manner as to ensure that the most mesial incision is placed on the distal aspect of the interproximal papilla, and the most distal incision is placed on the mesial aspect of the interproximal papilla (Fig. 2.33). The scalpel blade is angled so as to create a beveled incision, which will blend into the body of the papilla. A common technical error is to place the most mesial releasing incision on the mesial aspect of the papilla and/or the most distal releasing incision on the distal aspect of the interproximal papilla. In such a situation, the vertical releasing incision must be beveled into thinner buccal radicular soft tissues, rather than the thicker interproximal papilla. The net result will be more postoperative scarring and greater evidence of the incision upon healing.
Fig. 2.33 The releasing incisions always bevel into the thicker tissues of the papilla, rather than the thinner buccal radicular tissues.
Vertical releasing incisions must be of adequate extension to allow repositioning of the buccal mucoperiosteal flap at the desired level following osseous resective therapy, as will be discussed.
The buccal flap is now reflected in a full thickness manner beyond both the mucogingival junction and the level of expected osseous recontouring. Reflection of the most apical few millimeters of the buccal mucoperiosteal flap is carried out in a split thickness manner, utilizing a 15 blade. Retention of periosteum over the apical bone will facilitate apical repositioning of the buccal flap, and flap retention in this position following suturing (Figs. 2.34 to 2.36).
Fig. 2.34 A presurgical diagram of a mandibular cuspid and premolar region.
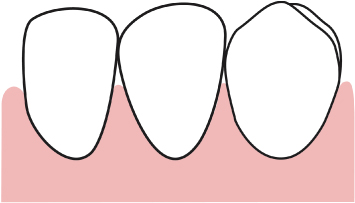
Fig. 2.35 Following the aforementioned sulcular and releasing incisions, a full thickness reflection is performed apical to the anticipated extent of osseous resective therapy. A = exposed alveolar bone.
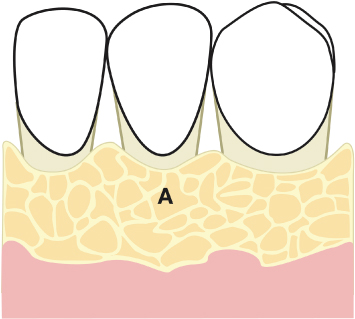
Fig. 2.36 Flap reflection is continued apically in a split-thickness manner, to afford retention of periosteal fibers and thus aid in flap repositioning and periosteal suturing. A = exposed alveolar bone; B = retained periosteum following split-thickness reflection.
A subsulcular palatal incision is made at such a level as to anticipate the final position of the osseous crest following crown-lengthening osseous surgery and bone recontouring. This crestally anticipated incision is scalloped in the same manner as already described for the buccal flap. Mesial and distal palatal vertical releasing incisions are placed, as previously described for the buccal mucoperiosteal flap design.
If the tooth to be crown lengthened is the terminal tooth in the arch, an internally beveled distal wedge procedure is performed. Buccal and palatal incisions are made on the distal aspects of the tooth (Figs. 2.37, 2.38). The incisions are beveled in such a manner as to undermine and thin the buccal and palatal tissues (Figs. 2.39, 2.40). The width between these incisions is determined by a combination of the amount of soft tissue to be removed and the expected reduction of buccal and/or palatal bony width during the crown-lengthening procedure. These “railroad track” incisions are carried beyond the tuberosity into the mucosal tissues distal to the terminal molar (Fig. 2.41). If the most terminal tooth present is a premolar, and it requires crown lengthening, these incisions are carried approximately 8–10 mm distal to the premolar.
Fig. 2.37 A presurgical view of a maxillary molar and premolar region.
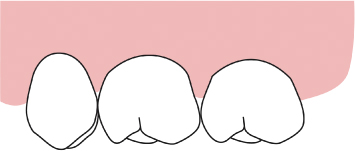
Fig. 2.38 An occlusal view of the same area demonstrating the distal wedge region.
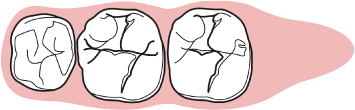
Fig. 2.39 A diagrammatic representation of a cross section of the tuberosity area distal to the second molar.
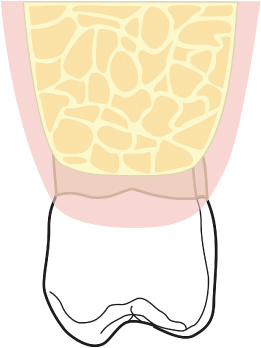
Fig. 2.40 The incisions in the tuberosity area are beveled so as to undermine and thin the buccal and palatal tissues distal to the second molar.
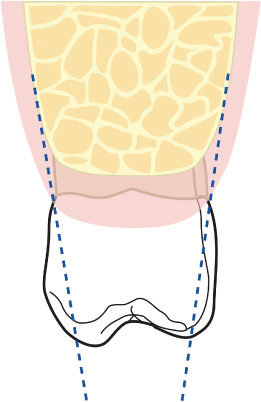
Fig. 2.41 The “railroad track” incisions are carried beyond the tuberosity into the mucosal tissue distal to the second molar.
Buccal and palatal vertical releasing incisions are placed as previously described, to facilitate flap reflection and debridement.
Even if a distal wedge procedure is to be performed, the aforementioned releasing incisions are placed on the mesial and distal aspects of the buccal and palatal flaps. Such an approach allows positioning of the buccal flap independent of the final soft-tissue position of the buccal distal wedge flap, as well as providing greater access and visualization for management of the distobuccal and distopalatal line angles of the terminal tooth in the arch (Fig. 2.42).
Fig. 2.42 A vertical releasing incision is placed on the distobuccal aspect of the second molar, to both provide greater visibility of the area and allow repositioning of the buccal flap independent of closure of the distal wedge region.
Failure to place a distobuccal vertical releasing incision in conjunction with performance of a distal wedge procedure leaves the treating clinician with two options : (1) an exaggerated submarginal scallop is employed as the incision rounds the buccal line angle of the most terminal molar, to allow suturing of the distal wedge soft-tissue flaps without unduly positioning the buccal flap more coronally than desired at the distobuccal line angle of the molar; or (2) the soft tissues are positioned in such a manner after suturing that soft-tissue repocketing will occur. A highly scalloped incision is not practical unless the patient presents with an exaggerated band of keratinized tissue on the distobuccal aspect of the molar in question (Fig. 2.43). Utilization of a distobuccal releasing incision to render closure of the distal wedge and positioning of the buccal flap independent of each other eliminates this concern.
Fig. 2.43 If a distobuccal vertical releasing incision is not placed, an exaggerated scallop must be created on the distobuccal aspect of the second molar, so as to avoid soft-tissue repocketing following closure of the distal wedge area.
The palatal flap is thinned, utilizing tissue forceps or a 1–2 pickup, to its most apical extent. This “internal wedge” of tissue is scored at its base with a 15 blade or Goldman-Fox 7 gingivectomy knife. The separated internal wedge of soft tissue is removed. If concomitant mucogingival therapy is required on the buccal aspects of the teeth being treated, the internal distal wedge tissue will be employed as a connective tissue graft beneath a buccal flap. This technique will be discussed in Chapter 5.
The purpose of thinning the palatal flap is to ensure an even thickness of palatal tissues, which will conform to the created osseous contours upon suturing (Figs. 2.44, 2.45). Such thinning of the palatal flap helps ensure that a soft-tissue “ledge” will not be created on the palatal aspects of the treated teeth (Fig. 2.46). If a soft-tissue “ledge” did result following therapy, subsequent healing would lead to a more coronal final position of the palatal soft-tissue margin, a greater extent of palatal soft-tissue repocketing, and a compromised outcome to the crown-lengthening surgery. Soft tissues do not heal at sharp angles. Failure to manage soft-tissue morphologies during surgery has significant, undesirable posthealing ramifications.
Fig. 2.44 A patient presents requiring crown-lengthening osseous surgery around the maxillary first molar.

Fig. 2.45 Following appropriate flap design and osseous resection, the crestally anticipated palatal flap is sutured at osseous crest. Note the long papillae that have been created between the premolar and molar, so as to cover the alveolar bone as much as possible. Following healing, adequate tooth structure will be exposed for appropriate restorative intervention.

Fig. 2.46 A 10-day postoperative view following crown-lengthening osseous surgery demonstrates the ramifications of improper flap design. Note the palatal ledge of tissue, due to inadequate thinning of the palatal flap at the time of surgical therapy. As healing continues, the soft-tissue margin will develop more coronally than desired, resulting in a subgingival restorative margin and soft-tissue repocketing.

OSSEOUS RESECTIVE THERAPY
Osseous resective surgery is performed around the tooth to be crown lengthened, so as to obtain the endpoints previously described. A #8 round diamond bur is first utilized to reduce buccal and palatal/lingual osseous ledging to the degree determined to be necessary to help ensure appropriate soft-tissue position and contour following healing (Figs. 2.47–2.49). In patients who present with a dense cortical plate of bone, a #8 round carbide bur is utilized under copious irrigation. It is important to realize that not all ledging and tori must be wholly eradicated. Rather, such bony protuberances must be reduced and contoured in such a manner as to allow the soft tissues to migrate over the established bony contours and heal in the desired manner and position. Osseous ledging may need to be reduced to the marginal crest, or simply reduced away from the marginal crest, depending upon the preexisting bony contours. In similar fashion, tori do not usually have to be completely eliminated. Recontouring tori so that their bulk does not interfere with the desired soft-tissue migration and final healing position is all that is required. Bony tori may be encountered in one of four situations.
1. The first is the instance where the bony torus is in such a position as to play no role in either the ability to eliminate osseous defects or to influence soft-tissue healing. In such a situation, the torus is left untouched.
Fig. 2.47 A diagrammatic representation of buccal and lingual ledging, found following flap reflection.
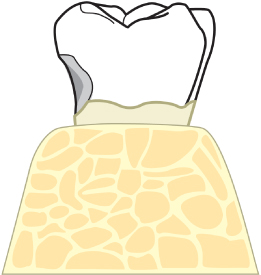
Fig. 2.48 The buccal and lingual ledging are reduced utilizing a #8 round diamond bur.
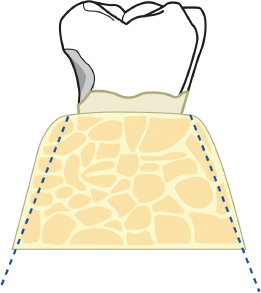
Fig. 2.49 A diagrammatic representation of the bone following reduction of the buccal and lingual ledging.
2. When the bony torus is in a position to have no influence on the ability to eliminate a bone crater or infrabony defect, but will influence soft-tissue healing, it should be reduced and sloped appropriately (Figs. 2.50–2.52).
Fig. 2.50 A lingual torus is present, which does not approach the osseous crest, but will affect the final soft-tissue contours following healing of the overlying soft tissues.
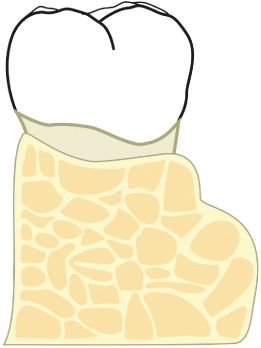
Fig. 2.51 The lingual torus is reduced.
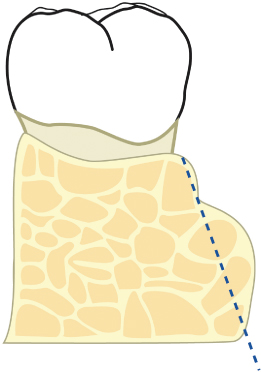
Fig. 2.52 Appropriate osseous contours are evident following reduction of the lingual torus of bone.

3. In the third instance, the bony torus approximates the alveolar crest but does not mask an infrabony defect. In these cases, the bony torus is reduced significantly and essentially eliminated in its most crestal half. The bone is then contoured so that a gentle flow is obtained between the reduced crestal area of the bony torus and the more apical portion of the torus (Figs. 2.53–2.55).
Fig. 2.53 A lingual torus is present which is confluent with the marginal alveolar bone. Failure to reduce this torus will result in soft-tissue healing in a more coronal position than desired, and subsequent repocketing.
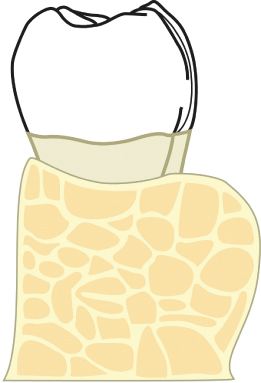
Fig. 2.54 The lingual torus is reduced.
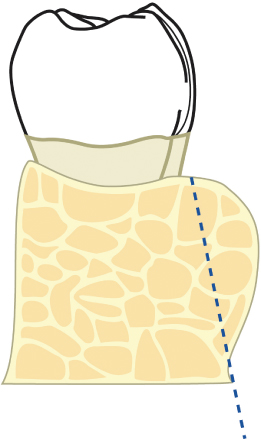
Fig. 2.55 Appropriate osseous contours are evident following reduction of the lingual torus of bone.

4. Finally, a bony torus may be in position to either make up the buccal, lingual, or palatal wall of an infrabony defect, or to preclude elimination of this defect without treating the torus. In such a situation, the torus is completely resected in its most crestal half, and the contours are carried into a gentle slope to be confluent with the more apical half of the torus (Figs. 2.56–2.58).
Fig. 2.56 A lingual torus is present, which is confluent with an osseous defect.
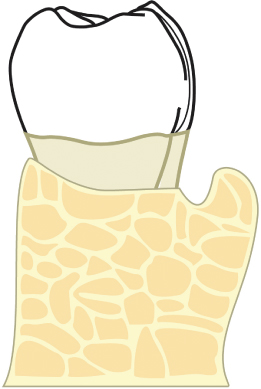
Fig. 2.57 The lingual torus is reshaped in such as manner as to eliminate the lingual component of the osseous defect.
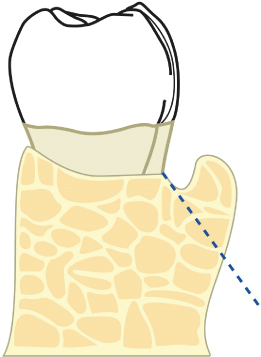
Fig. 2.58 Appropriate osseous contours are evident following reduction of the lingual torus of bone.

Reduction of osseous ledging and/or tori is accomplished within the context of developing desired osseous contours and “positive architecture.” Failure to do so will result in repocketing, and a nonideal treatment result (Figs. 2.59–2.65).
Fig. 2.59 A patient presents with 5–6-mm interproximal pockets, subgingival interproximal restorations, and bleeding upon probing. A palatal view demonstrates a “bulge” in the soft tissues between the first and second molar.

Fig. 2.60 Flap reflection reveals a palatal torus. This torus is in such a position as to render appropriate osseous therapy impractical without its elimination.
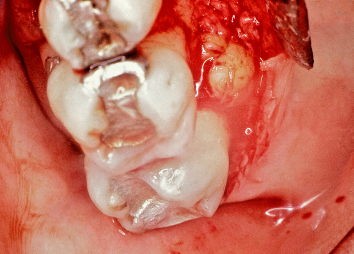
Fig. 2.61 The palatal torus is eliminated and ideal osseous contours are attained. Following suturing of the mucoperiosteal flaps at the appropriate positions, the resultant attachment apparatus and minimal probing depths will be highly maintainable by the patient.
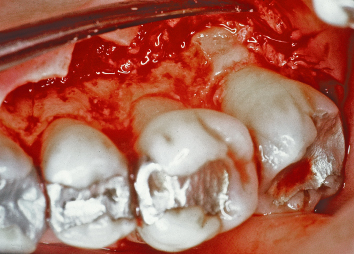
Fig. 2.62 A patient presents requiring crown-lengthening osseous surgery around the mandibular second molar.

Fig. 2.63 Flap reflection reveals a significant lingual bony torus. If this torus is not reduced appropriately, the soft tissues will heal in a position more coronal than desired.
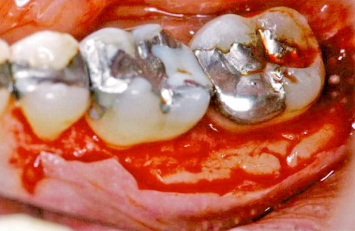
Fig. 2.64 The mandibular torus has been reduced and reshaped to both anticipate and participate in soft-tissue healing, and to contribute to attainment of the desired postoperative tissue contours.

Fig. 2.65 Following suturing, it is evident that the soft tissues will heal at the desired levels.

The principles of osseous resective therapy have been well elucidated in the past. These principles include:
- Elimination and/or reshaping of osseous ledging and/or tori to such an extent that the bony contours will not hinder the development of ideal soft-tissue form following healing.
- Elimination of all interproximal osseous defects through resection, regeneration, or a combination of the two.
- Establishment of positive architecture, defined as development of appropriate parabolae on the buccal and lingual/palatal aspects of the roots, so that the bases of the parabolae are apical to the interproximal bone heights.
- Elimination of furcation involvements: This topic will be discussed in detail in Chapter 3.
A crown-lengthening bur is now employed in a circumferential manner around the tooth to be crown lengthened, ensuring that at least 4 mm of dimension is present between the planned final restorative margin position and the osseous crest (Figs. 2.66, 2.67). Any “moats” created by the crown-lengthening bur on the buccal or lingual/palatal aspects of the teeth are eliminated with the #8 round diamond bur (Figs. 2.68–2.70). If the tooth to be treated has not already been temporized for a full coverage restoration, thus limiting access to the mid-interproximal bone on the mesial and distal aspects of the tooth being crown lengthened, the crown-lengthening bur is utilized as far interproximally as possible. A #2 round diamond bur is then employed to remove the small (approximately 1–1.5 mm in dimension) peak of bone which will remain at the mid-interproximal points of the tooth following utilization of the crown-lengthening bur.
Fig. 2.66 Following flap reflection, the position of the carious lesion with regard to the alveolar crest, and the need for crown-lengthening surgery, are evident.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


