2
The Developing Dentition
Introduction
Human dental development consists of three stages: establishment of the primary dentition; the mixed dentition stage following eruption of the first permanent molars and incisors; and completion of the secondary (or permanent) dentition with eruption of the remaining permanent teeth, including the third molars if present.
Monitoring dental development with appropriate intervention (interceptive treatment) is an important aspect of orthodontics. Problems that can occur in either the primary or mixed dentitions are essentially anomalies in the developmental process, functional problems or early presentation of an underlying malocclusion, all of which may warrant early treatment. These include:
- Delay or failure of eruption of teeth
- Developmentally absent teeth (hypodontia)
- Supernumerary (extra) teeth
- Anomalous teeth (abnormal morphology)
- Early tooth loss due to dental trauma or caries (often resulting in space loss)
- Anterior and posterior crossbites with or without displacement
- Persistent habits such as digit sucking
- Early manifestation of tooth/arch size discrepancies (e.g. spacing or crowding)
- Early manifestation of skeletal discrepancies (moderate-to-severe class II and III cases).
Examples of interceptive treatment include:
- Elective extraction of primary teeth to encourage favourable eruption of permanent teeth, which may be ectopic in position; e.g. removal of maxillary primary canines to encourage an improvement in the position of ectopic maxillary canines.
- Elective extraction of first permanent molars of poor prognosis, with a view to encouraging the second permanent molars to erupt further forward in the arch.
- Space maintenance following early loss of primary teeth or for maintenance of the Leeway space.
- Treatment with removable or fixed appliances: to correct anterior or posterior crossbites associated with a significant displacement.
- Surgical exposure of impacted maxillary incisors, followed by removable or fixed appliances to apply traction to the impacted tooth or teeth, in order to facilitate eruption.
- Attempts at ‘growth modification’ may include functional appliances to address skeletal discrepancies in class II or class III cases, or the use of protraction headgear for management of maxillary hypoplasia, (with or without rapid maxillary expansion) in skeletal class III cases.
The merits of initiating orthodontics in the early mixed dentition has been debated and researched (Jolley et al., 2010). Generally, early or interceptive treatment should aim either to eliminate a problem or to simplify subsequent treatment. Focused aims and objectives avoid unnecessary or protracted treatment.
Advocates of early treatment claim that it optimizes growth potential when addressing skeletal problems, leads to better compliance, reduces risk of trauma in class II division 1 malocclusions, enhances psychological wellbeing and limits or even eliminates the need for a second course of treatment in adolescence.
While all of these claims have merit and may be applicable to individual cases, the majority of orthodontic treatment can be successfully and efficiently carried out in the late mixed and early permanent dentition.
There is more positive evidence for early correction of some aspects of malocclusion than others. For example, it is generally accepted practice to correct an anterior or posterior crossbite early if there is a functional displacement. Maintenance of the Leeway space during the transition from the mixed to permanent dentition has also been shown to be an effective way of providing space to treat mild crowding (Little et al., 1990; Brennan and Gianelly, 2000). Some early treatments are less widely accepted, e.g. there appears to be less evidence for early treatment designed to expand the dental arches in the mixed dentition to treat crowding.
The long-term results of early treatment for class II division 1 malocclusions are no better if treatment is started in the late mixed dentition in relation to growth or occlusal outcome. The only reported differences are the additional cost and duration of the treatment (Tulloch et al., 2004).
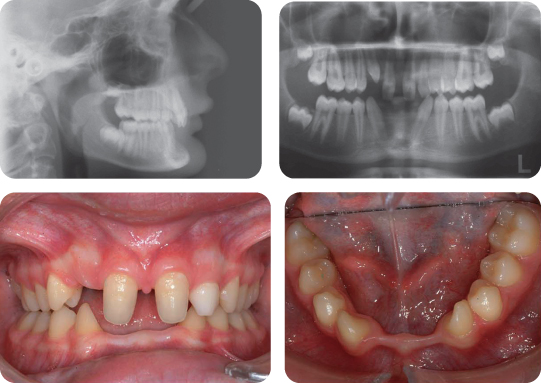
Case 2.1
At What Stage of Development Is Her Dentition in the clinical photographs?
She is in the early permanent dentition. The second permanent molars are unerupted, with the exception of the LL7, which is partially erupted.
What Are the Main Features of Her Malocclusion?
- Class II division 1 incisor relationship with an increased overjet and increased overbite, which is complete to the palate
- Molar relationship is 1/2 unit class II on the right and class I on the left
- Centre lines are coincident
- Erupted supplemental UL2
Why Is the Molar Relationship Not the Same on Both Sides?
The presence of an additional tooth in the upper left quadrant, but essentially coincident centre lines, means that the UL6 is positioned more distal than it would normally be – hence a class I relationship rather than class II.
How Common Are Supernumerary Teeth?
In the permanent dentition supernumerary teeth are seen in 0.1–3.2% of individuals. Caucasian males are more commonly affected than females in a ratio of 2 : 1 (Fleming et al., 2010). The reported prevalence in the primary dentition ranges from 0.06% to 0.8% with no associated sexual dimorphism.
Where Are Supernumerary Teeth Most Likely to Be Seen?
In the anterior maxilla.
What Other Forms of Supernumerary Teeth Are Seen in the Permanent Dentition?
The other forms are conical, tuberculate and odontome (complex and compound).
What Consequences Can Supernumerary Teeth Have for the Developing Dentition?
If a supernumerary tooth erupts, it can cause localized crowding or spacing. If it remains unerupted, it can cause impaction or displacement of teeth, or occasionally may become cystic.
In the Case Described, What Is the Likeliest Course of Action?
The underlying malocclusion will require treatment to reduce the overjet and overbite, and align and co-ordinate the dental arches. To achieve this, the supernumerary tooth will require extraction; otherwise a tooth-size discrepancy would be present between the arches, making it impossible to achieve a co-ordinated class I occlusion.
When deciding which tooth to extract, generally the supernumerary tooth is chosen; however, the coronal and root anatomy of both the normal and supernumerary teeth should be evaluated carefully before making the final extraction decision. In this case the most distal (supplemental) lateral incisor was extracted. Following functional appliance treatment and fixed appliances the final occlusion is shown in Figure 2.2.
Case 2.2
Summary
A 9-year-old female presented in the mixed dentition with a class II division 1 malocclusion on a mild skeletal class II pattern with average vertical facial proportions (Figure 2.3).
What Is the Most Likely Cause of the Anterior Open Bite?
The most likely cause is a persistent digit sucking habit.
Treatment Plan
- Stop the digit sucking habit
- Monitor further dental development and plan comprehensive treatment upon cessation of the habit
What Are the Typical Effects of a Digit Sucking Habit on the Developing Dentition?
- Increased maxillary and relative prognathism
- Increased maxillary length
- Proclination of maxillary incisors
- Retroclination of mandibular incisors
- Increased overjet
- Reduced overbite
- Unilateral posterior crossbite
What Factors Influence the Outcome of Digit Sucking?
The outcome of digit sucking is governed by the nature, frequency, intensity and duration of the habit (Larsson, 1987). A minimum threshold of 4–6 hours per day is believed to be required to produce a significant malocclusion. Specific effects are variable and often asymmetric, being mediated directly by the position of the digit or indirectly by alteration to tongue position.
What Is the Prevalence of Digit Sucking?
The prevalence of digit sucking is age-related. It has been reported as 12% of 9-year olds and 2% of 12-year olds (Brenchley, 1991).
What Conservative Techniques May Be Used to Stop Digit Sucking?
Conservative methods of habit dissuasion are usually preferable to physical intervention in the first instance. Patient and parental education are instrumental (Levine, 1999). Non-invasive methods include:
- Positive reinforcement by reward and habit reversal where the child is taught to carry out an alternative activity when the urge to suck arises
- Use of plasters, gloves or bitter flavoured agents applied to the digit to make the habit less satisfying.
These non-invasive techniques should be attempted for 3–6 months and can be very successful in improving the occlusion.
What Interceptive Procedures May Be Performed to Dissuade Digit Sucking?
Where the habit persists despite conservative measures, simple fixed orthodontic appliances including palatal arches, with one of a variety of projections (inverted goalposts, beads or cribs), may be used for 6–12 months. Use of removable orthodontic appliances may also be effective in these cases (Figures 2.4 and 2.5); however, they may be unsuccessful due to poor co-operation.
Case 2.3
Summary
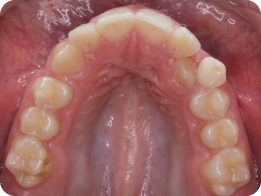
- Well-aligned arches in the late mixed dentition
- Retained, immobile maxillary primary canines
- Maxillary canines not palpable buccally
What Information Does the Panoramic Radiograph Provide (Figure 2.6)?
The UR3 is ectopic:
- Cusp tip of the UR3 crosses the UR2
- There is no evidence of root resorption of the URC
- There is no evidence of pathology.
Treatment Plan
- Extraction of both maxillary primary canines
- Review after 12 months
How Common Is Impaction of the Maxillary Canine?
With the exception of the third molars, the maxillary canine is the most frequently impacted tooth with an incidence of 2–3% and a female predilection. The majority (up to 85%) lie palatal to the arch. Bilateral occurrence accounts for 8% of cases with ectopic maxillary canines (Ericson and Kurol, 1988).
The UR3 erupted 12 months after removal of the URC (Figure 2.7).
How Useful Is the Interceptive Removal of a Primary Maxillary Canine in Cases of Maxillary Permanent Canine Ectopia?
Interceptive removal of retained primary canines has been shown to promote favourable spontaneous alignment of the canine. In a prospective study, 78% of ectopic canines improved their position following removal of the upper primary canines in 10–13-year olds with well-aligned dental arches (Ericson and Kurol, 1988). The prognosis for spontaneous alignment reduces with greater mesial displacement of the canine tip (Ericson and Kurol, 1988; Power and Short, 1993). It is important to note that improvement in the eruption path of the permanent canine is unlikely to arise later than 12 months after the extraction of the primary canine.
How Is Maxillary Canine Ectopia Diagnosed?
- Clinical inspection and palpation.
- Radiographs are a secondary measure. A survey of 505 Swedish schoolchildren has shown the prevalence of non-palpable and unerupted canines where radiographic examination was necessary to be just 3% between 11 and 15 years (Ericson and Kurol, 1988).
What Clinical Features May Be Indicative of an Ectopic Maxillary Canine?
- Non-palpable permanent canines in the buccal sulcus at 11–12 years of age
- Firm, immobile primary canine when the contra-lateral permanent canine has erupted 6 months earlier
- Significant displacement, including tipping and abnormal inclination of adjacent lateral incisors
- A palatal bulge in the presence of a firm retained primary canine
- Diminutive maxillary lateral incisors. Palatal impaction of canines is also associated with ectopic development, with 42% arising adjacent to diminutive or congenitally absent maxillary lateral incisors (Becker, 1984)
What Other Interceptive Measures May Be Useful to Encourage Eruption While Avoiding Mechanical Eruption?
Techniques, including expansion, space redistribution and distal molar movement, have all demonstrated higher levels of spontaneous eruption when compared with removal of primary canines in isolation (Baccetti et al., 2008; 2009).
Comment on the Quality of Evidence in Relation to Interceptive Removal of Primary Canines and Spontaneous Eruption of Canines
In a systematic literature review it has been suggested that the evidence in support of removal of primary canines to intercept ectopic development is unreliable (Parkin et al., 2009a). While a number of prospective studies have been published, the reviewers felt that they were poorly reported. Factors that should be considered when conducting trials in this area include: concealed random allocation, blind assessment, homogeneity of the groups at the beginning of the trial, correct statistical analysis taking into account clustering in patients with bilateral ectopic canines, and appropriate management of withdrawals.
Case 2.4
How Old Do You Think She Is?
Around 9–10 years of age.
Root development of the first molars is complete, which usually occurs around the age of 9.5 years.
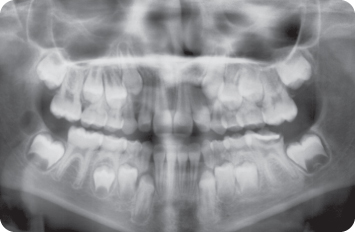
What Are the Main Features Seen on the Panoramic Radiograph?
- Mixed dentition
- Incisors have erupted
- LL6 is grossly carious; there is evidence of periapical infection on the distal root and a temporary restoration is in place
- All the permanent teeth are present except the third molars (although there is some evidence of early follicular development of the LR8)
- Crown formation of the second molars is complete. In the mandibular arch, early development of the inter-radicular region has begun
The Dentist Does not Believe the LL6 Can Be Restored. What Advice Would You Give?
Extract the LL6 and consider a compensating extraction of the UL6 to prevent over-eruption of this tooth. The lack of third molar development on the left side means that extraction of the UL6 is not ideal. However, there is early evidence of third molar development in the lower right quadrant and this, combined with the relatively young age of the patient, means that third molar development may well subsequently occur.
Alternatively, extraction of the UL6 might be delayed and the eruptive position monitored following extraction of the LL6.
The timing of extraction also needs to be considered, although in this case extraction should not be delayed because the patient is in pain. However, to ensure the best eruptive position for the lower second permanent molars, their development should be slightly more advanced and extraction of the LL6 carried out ideally in around 6 months’ time. This is also dependent on the space requirement in the lower arch as if there is crowding that will require extractions to treat, it may be better to delay the extraction of the LL6 until the LL7 has erupted, so the space created can be used to relieve the crowding.
Other local problems
What Dental Abnormality Is Apparent in Figure 2.9?
Bilateral transposition of mandibular lateral incisors and canines.
How Is This Anomaly Classified?
Transpositions are classified by jaw of occurrence, tooth type and site. This bilateral transposition is classified as Mn.C.I2.
What Is the Difference between a True Transposition and a Pseudotransposition?
A true transposition involves both the crowns and roots of the affected teeth. A pseudotranspositon involves positional interchange of the crowns only.
What Is the Aetiology of Dental Transposition?
Transposition is a multifactorial disorder with both genetic and environmental contributions (Ely et al., 2006).
Comment on the Regional Distribution of Transpositions
Transpositions are most common in the maxillary arch and typically involve the canine. Involvement of the central incisors or molar teeth is uncommon. Bilateral transposition is less common than unilateral transposition in both arches. In bilateral cases, asymmetrical bilateral transposition is very rare.
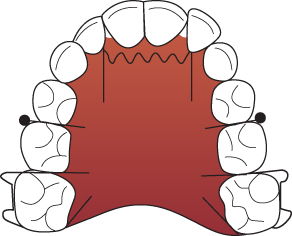
Describe the Appearance of the Maxillary Dental Arch in Figure 2.10
A patient in the early permanent dentition with the UL3 erupted into a palatally-displaced position. The overlying ULC is retained. There is mild hypoplasia associated with the UR6.
What Treatment Is Required?
Consideration should be given to removal of the primary canine as it is retained and likely to be displacing the permanent successor.
At What Stage of Root Development Do Permanent Teeth Usually Erupt?
A permanent tooth should erupt when approximately 75% of its root has formed.
What Dental Anomaly Is Apparent in Figure 2.11?
Infra-occlusion of the ULE and LLE.
How Common Is Infra-Occlusion?
Infra-occlusion most commonly affects primary molars with a prevalence of 5–11%.
How Is the Severity of Infra-Occlusion Classified?
Infra-occlusion may be classified as mild, moderate or severe. It is diagnosed if the tooth had lost its vertical position relative to the neighbouring teeth. Moderately infra-occluded teeth lie below the level of adjacent contact points. Severely infra-occluded teeth are located at the level of or below the alveolar crest.
What Two Factors Are Most Critical When Planning Treatment?
- Degree of infra-occlusion
- Presence of a permanent successor
If the Permanent Successor Is Present and the Degree of Infra-Occlusion Is Mild, What Treatment Is Usually Required?
No active treatment is usually necessary, as the primary molar will normally exfoliate within the expected timeframe. Indications for removal of the involved primary tooth in such cases include severe infra-occlusion, beneath the adjacent contact points with a resultant risk of tipping of the adjacent teeth, and over-eruption of the opposing teeth.
Describe the Dental Features Seen in This 15-Year-Old Boy (Figure 2.12)
- Upper central and lateral incisors are double teeth
- LL5 is absent
- UL5, UR5 and LR5 are impacted
- LLE, ULE and LRE are retained
- Root formation associated with the canine and premolar dentitions is developmentally delayed
What Is the Difference between a Double Tooth and a Megadont Tooth?
A megadont tooth is one that is more than two standard deviations larger than the mean. It can be distinguished from a double tooth by an absence of coronal notching, relatively normal morphology and the presence of an appropriate number of teeth in the dental arch overall. Megadontia most commonly affects maxillary permanent central incisors and second premolars.
A double tooth occurs when there is hard tissue continuity between adjacent teeth.
Describe the Dental Features in Figure 2.13
- Primary dentition
- Class I incisor relationship
- Lower centre line displaced to the left
- Double tooth involving the LLB and LLC
What Is the Condition Seen in Figure 2.14?
Molar–incisor hypo-mineralization (MIH) – a condition associated with demarcated, qualitative defects of enamel of systemic origin affecting one or more permanent molars with or without involvement of the incisor teeth.
What Is the Cause of This Condition?
The cause is currently unknown; however, there is some evidence to suggest that polychlorinated biphenyl/dioxin exposure is involved in the aetiology of MIH. Weaker evidence exists for the role of nutrition, birth and neonatal factors, and acute or chronic childhood illness/treatment; and there is very weak evidence to implicate fluoride or breastfeeding (Crombie et al., 2008).
How Can MIH Complicate Future Orthodontic Treatment?
In severe cases:
- Difficulty bonding incisor teeth
- Need for first molar extraction (either enforced or elective).
Case 2.5
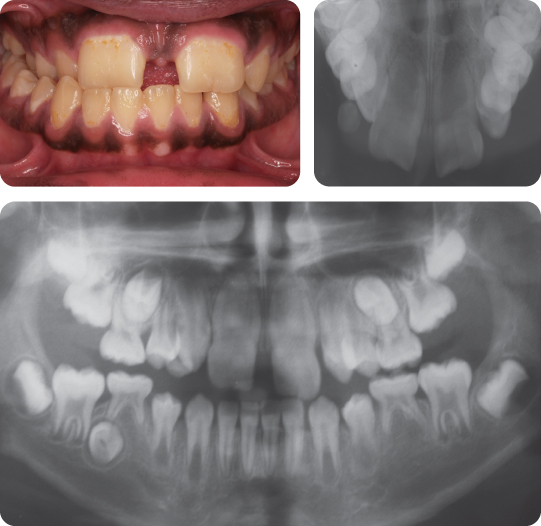
What Are the Main Features of the Occlusion?
- Mixed dentition
- Class II division 1 incisor relationship
- Absence of the UR1
- Crowding of the labial segments
What Is the Differential Diagnosis?
- Impaction/failure of eruption of the UR1
- Previous loss of the UR1 following trauma
- Congenital absence of the UR1
What Are the Possible Local Causes of Tooth Impaction in the Anterior Maxilla?
- Supernumerary tooth
- Crowding
- Trauma and dilaceration
- Ectopic tooth germ position
- Retained primary teeth
- Local pathology
In This Case, the UR1 Was Lost Following Trauma and Avulsion. What Potential Problems Are There in the Long-Term Management of This Malocclusion?
- There has been space loss in the anterior maxilla. This has occurred primarily by forward movement of the UR2 into the UR1 space, as the centre lines are coincident.
- Space could be regained at this stage with a simple fixed or removable appliance (possibly with extraction of the primary canines), followed by space maintenance with a removable retainer and pontic for the UR1. Definitive treatment could be undertaken in the permanent dentition with restoration of the UR1 space with a resin-retained bridge or dental implant.
- Alternatively, the space could be allowed to close spontaneously and the occlusion managed definitively in the early permanent dentition. This strategy has the advantage of maintaining alveolar bone height in the upper labial segment, which facilitates implant placement after space opening.
- In both strategies, extractions are likely to be required because of the underlying crowding.
Case 2.6
Summarize the Main Clinical Features of This Malocclusion
- A class III incisor relationship in the mixed dentition with a reduced and complete overbite
- Molar relationship is 1/2 unit class II bilaterally
- Upper centre line is displaced to the left
- UL1 is rotated mesio-palatally
Why Is the Molar Relationship Class II?
The lower Es are still present. These are larger in the mesio-distal dimension than the second premolars; consequently, the mandibular first molars are held in an artificial distal position.
What Is the Cause of the Rotated UL1?
The UL1 has rotated due to the presence of an unerupted upper midline supernumerary tooth.
Comment on the Morphology and Position of the Supernumerary Tooth
This is an upper midline supernumerary. It is conical in morphology and is inverted. It is likely to be a mesiodens.
How Should This Case Be Managed?
Treatment will involve surgical removal of the supernumerary tooth. Fixed appliances will be required to de-rotate the UL1. Consideration will also need to be given to the removal of two upper premolars to relieve crowding and facilitate arch alignment. Following removal of the appliances, an upper bonded retainer will be necessary to prevent relapse of the rotational correction.
Case 2.7
What Has Happened During This Time?
The permanent lateral incisor teeth have erupted.
Describe the Malocclusion
There is a class I incisor relationship, with the UR1 in crossbite. There is crowding in both arches, with the UR2 erupted palatally.
What Are the Advantages of Correcting the Crossbite at This Stage?
- Removal of any mandibular displacement
- Prevention of any gingival recession occurring in association with the LR1
- Likely to be stable because of the presence of a positive overbite
What Is the Dental Health Component of the Index of Orthodontic Treatment Need (IOTN) of This Case?
It depends upon the size of the mandibular displacement between retruded contact position (RCP) and inter-cuspal position (ICP). In this case it was greater than 2 mm, which indicates an IOTN of 4.c. If it had been between 1 and 2 mm, the IOTN would have been 3.c, and if less than 1 mm, 2.c.
How Would You Manage This Case?
With a removable appliance to procline the UR1 and correct the crossbite. A sectional fixed appliance or 2 × 4 appliance could also be used, but the position of the UR2 complicates this.
How Would You Design a Removable Appliance?
- Adams clasps for the 6D/D6 (or a double clasp for 6E/E6) (0.7-mm stainless steel wire) for retention
- Z spring (0.5-mm stainless steel wire) to procline the UR1
- Acrylic base plate with posterior capping (to open the bite and allow movement of the UR1)
What Is Selective Tooth Agenesis?
Selective tooth agenesis (STHAG) is a failure of tooth development in either dentition. It has a number of alternative descriptors, with the most common being hypodontia, the precise definition of which is the developmental absence of six or fewer permanent teeth (not including the third molars).
What Are the General Characteristics of This Condition in European Populations?
- Prevalence is reported to be approximately 4–6% in the permanent dentition and 1–2% in the primary dentition.
- It is more common in females than males.
- Severity can vary from absence of one tooth to all the permanent teeth (anodontia), although this is rare.
- Severe hypodontia (oligodontia) is the term used where more than six permanent teeth (excluding third molars) are absent.
- The teeth reported as being most commonly absent are the mandibular second premolars, maxillary lateral incisors and maxillary second premolars. This has led to the term ‘incisor–premolar’ hypodontia being used.
- Hypodontia and microdontia (reduction in the size of teeth) are often associated. Generalized microdontia can occur in some cases and is often complicated by conical-shaped teeth, resulting in generalized spacing. In some cases microdontia only affects certain teeth, with diminutive (or peg-shaped) lateral incisors being most common.
What Is the Aetiological Basis of This Condition?
The aetiology of STHAG is still unclear. It is thought that both environmental and genetic factors may be involved (Cobourne, 2007; Parkin et al., 2009b).
Two main forms of hypodontia have been identified:
- Non-syndromic (familial) STHAG
- Tooth agenesis associated with syndromic conditions.
How Can Familial (Non-Syndromic) STHAG Be Inherited?
The pattern of inheritance is variable, occurring as an autosomal dominant, autosomal recessive or sex-linked trait. STHAG can occur in the primary and permanent dentitions; however, it is more common in the permanent dentition. When occurring in the primary dentition, it often indicates the possibility of tooth agenesis in the permanent dentition.
Give Some Examples of Syndromes Associated with tooth agenesis
- Down syndrome
- Ectodermal dysplasia
- Incontinentia pigmenti
- Ellis–van Creveld syndrome
What Are the Main Clinical Features Associated with severe STHAG (Figure 2.18)?
- Severe STHAG is often associated with a retrusive facial profile and reduced lower anterior face height. In cases where there are reduced vertical proportions, this often results in an increased overbite.
- The intra-oral features vary from mild cases where there is one congenitally absent tooth to more severe forms with more than six teeth missing. In severe cases there is often generalized spacing and retention of primary teeth.
- There is often an associated microdontia, either localized (peg-shaped lateral incisors) or generalized.
- Retained primary teeth can remain in situ until adulthood in many cases. Submerging primary molars are often an indication that the permanent successor may be absent.
- In cases where there are multiple teeth missing, the absence of a permanent successor results in underdevelopment of the alveolar bone with narrow alveolar ridges. This can occasionally manifest as lateral open bites.
What Are the Main Options When Treatment Planning Cases with tooth agenesis?
There are two main approaches to managing hypodontia:
- Redistribution of space using orthodontics to allow restorative replacement of the missing teeth and restorative build-up of diminutive teeth
- Orthodontic space closure, which eliminates the need for restorations.
What Factors Can Influence Treatment Planning Decisions in Cases with tooth agenesis/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses