Chapter 2
Principles and Practice of Periodontal Surgery 2:
Basic Surgical Principles
Aim
The aim of this chapter is to explore the principles underpinning contemporary periodontal surgery by guiding the reader through the various stages of surgery. The text will describe modern surgical equipment and methods and contrast this with more traditional armamentaria and approaches.
Outcome
Having read this chapter, the reader will be aware of general surgical techniques applicable to all aspects of periodontal surgery. The practitioner will understand the value and use of microsurgical methods and how these principles can be transferred to their own surgical practice.
Introduction
Periodontal surgery encompasses a broad range of procedures involving the supporting tissues of the teeth. These vary in complexity from simple exodontia to technically demanding periodontal plastic surgery and include the management of periodontal and endodontic disease, preparation for and placement of implants, and preparatory treatment for fixed and removable prostheses (preprosthetic surgery).
Periodontal surgical methods were practised in Roman times when diseased gingival tissues were excised with crude instruments and without local anaesthetic. Burning of the tissue was considered an important step in the cure of disease. The last five years, however, have embraced rapid changes in therapeutic techniques owing to our greater understanding of the biological principles of healing and the consequences of surgical insult. Modern surgical management reflects both a move towards evidence-based practice and the introduction of improved techniques and instrumentation.
Whilst the complexity of microsurgery may not be routinely necessary in general dental practice, many of the principles and equipment used do improve the ease and predictability of standard surgical management.
Tenets of Halsted
Many of the principles of modern day surgery are based on the teaching of William Halsted from the late nineteenth century. He scorned common surgical practices that relied on brute strength and in their place espoused careful and gentle tissue handling. His mastectomy operation for breast cancer revolutionised what was once a uniformly fatal disease. He also introduced the use of rubber gloves to surgery.
Contemporary surgical practice recognises the “Tenets of Halsted” (Box 2-1). These tenets still stand as guiding principles in periodontal surgery.
Box 2-1 Tenets of Halsted
The gentle handling of tissues.
An aseptic technique.
Sharp anatomic dissection of tissues.
Careful haemostasis, using fine, non-irritating suture material in minimal amounts.
The obliteration of dead space in the wound.
The avoidance of tension.
The importance of rest.
Operative Management
Meticulous technique and careful tissue-handling married with microsurgical instrumentation will provide predictable and aesthetic healing in the majority of cases. Magnification using loupes is invaluable for periodontal surgery. The limited field of the operating microscope can make periodontal surgical management taxing where a broader visual field is required. Specific surgical techniques will be applicable to particular flap designs and procedures. The following form generic guiding principles for operative surgical management.
Flap Design
A myriad of flap designs exist in periodontal surgery. Commonly used flap types and their synonyms are presented in Table 2-1 (pages 15, 16 and 17).
| Flap descriptor | Secondary descriptor | Description detail | Advantages | Disadvantages | Uses |
| Flap geometry | Marginal | Incision follows gingival margins | |||
| Simple replaced flap (envelope flap) Modified Widman flap |
Intrasulcular incision around teeth of interest (modified Widman involves a parasulcular incision prior to the sulcular incision) | Simple, quick Replacement and suturing is simple |
Access is limited to coronal aspects of root in most instances | Exodontia. Simple root surface debridement (RSD) Guided tissue regeneration (GTR) |
|
| Two-sided flap (triangular flap) | Intrasulcular incision with one vertical relieving incision | Better access to deep periodontal lesions or root apices | Access is limited where roots are long or horizontal component of flap is short | Exodontia. Periradicular surgery RSD deep sites Root resection |
|
| Three-sided flap | Intrasulcular incision with bilateral vertical relieving incisions | Best access of all flap types | Replacement may be demanding Where horizontal component of flap is short, blood supply may be compromised |
Any periodontal surgery where maximum access is required | |
| Submarginal | Incision apical to marginal gingivae | ||||
| Semilunar flap | Incision made over roots of interest | Quick and simple No marginal recession |
Access is usually fairly limited and these flap designs are now relatively outmoded for this reason | Used for periradicular surgery | |
| Trapezoidal flap | |||||
| Ochsenbein–Luebke flap | |||||
| Flap thickness | Full thickness (muco-periosteal) | Incision down to bone, flap raised from bone with blunt dissection | Good access to bone and root surface Simple procedure Minimal post-operative discomfort |
Unsuitable for grafting – does not offer vascular bed Limited mobility of flap |
Most periodontal surgical procedures |
| Split thickness (mucosal) | Most often a three-sided design but variable Sharp dissection of tissues leaves periosteum intact |
Provides good blood supply for grafts Avoids exposure dehiscence |
Technically demanding Greater post-operative discomfort No access to underlying bone or root surface |
Used for free gingival or connective tissue grafting | |
| Replacement position | Replaced flap | Flap margins are replaced in original position | Best closure and haemostasis Healing by primary intention |
Not suitable for grafting or some crown-lengthening procedures | Used for most periodontal surgery |
| Repositioned flap (coronally, apically, laterally) | Margins replaced in altered relationship | Allows coverage of defects, grafts or exposure of tooth substance | Healing by secondary intention Technically demanding |
Used for mucogingival surgery and crown lengthening | |
In general most flaps can be described as having a horizontal and a vertical component. The horizontal component of the flap normally involves an intrasulcular or parasulcular incision around the gingival margins of the teeth of interest. The vertical component of the flap is also known as a relieving incision. This helps to relieve tissue tension and allow greater access to the periradicular tissues. Ideally a flap should solely involve an intrasulcular incision for surgical access (envelope flap). This design is also referred to as a simple replaced flap and is utilised for open root surface debridement or where simple access for surgical exodontia is required. Where there is a need for greater access or relief of tissue tension, vertical relieving incisions may be employed. In general, two relieving incisions (a three-sided flap) provide optimal access to the surgical site and reduce tissue tension (Fig 2-1).
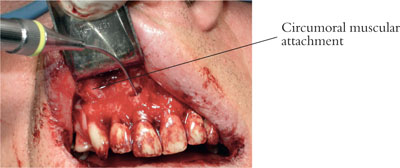
Fig 2-1 A large three-sided flap provides excellent access for root-end filling during periradicular surgery. Muscle attachment is visible on the right-hand side.
One relieving incision (a two-sided flap), however, may provide adequate access and improved blood supply and may reduce the number of sutures required for closure (Fig 2-2).

Fig 2-2 Atwo-sided flap with a wide horizontal component can provide excellent access.
Animal research has demonstrated that gingival blood vessels tend to have a relatively vertical orientation (Fig 2-3a,b). Incisions, therefore, should be as vertically orientated as possible to minimise bisecting these vessels. This approach will reduce intra-operative bleeding and also m/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


