2
Chemical Mediators f the Vascular Response
Officers control troops with predetermined strategies and regulations. Sometimes, external forces dictate and control military actions and reactions, but usually the internal chain of command sets the pace. Inflammation is controlled by the presence of a group of substances called chemical mediators, each with a specific role at some definite stage of the inflammatory reaction. These mediators may be exogenous (arise from bacteria or chemical irritants) or endogenous in origin. In this section we will be dealing with the latter.
It is important to note that the exact sequence of the appearance of various mediators and their dependence on, or independence of, each other is still largely speculative. Furthermore, other mediators have probably not yet been identified.
Before we get into a description of the endogenous chemical mediators, it might be helpful to understand that:
- The body needs some mechanism for “immediate” action on the battle front, which will also initiate other events. The first mediator in this section, histamine, serves this function. In order to be immediately effective (as in “ready to go”) this mediator is already present in the tissues before the damage occurs. Histamine just sits tight and usually exerts its effect only after injury releases it. (Note: Some allergic reactions also cause its release.)
- Other mediators must be produced at the site, or by migrating leukocytes attracted to the injury.
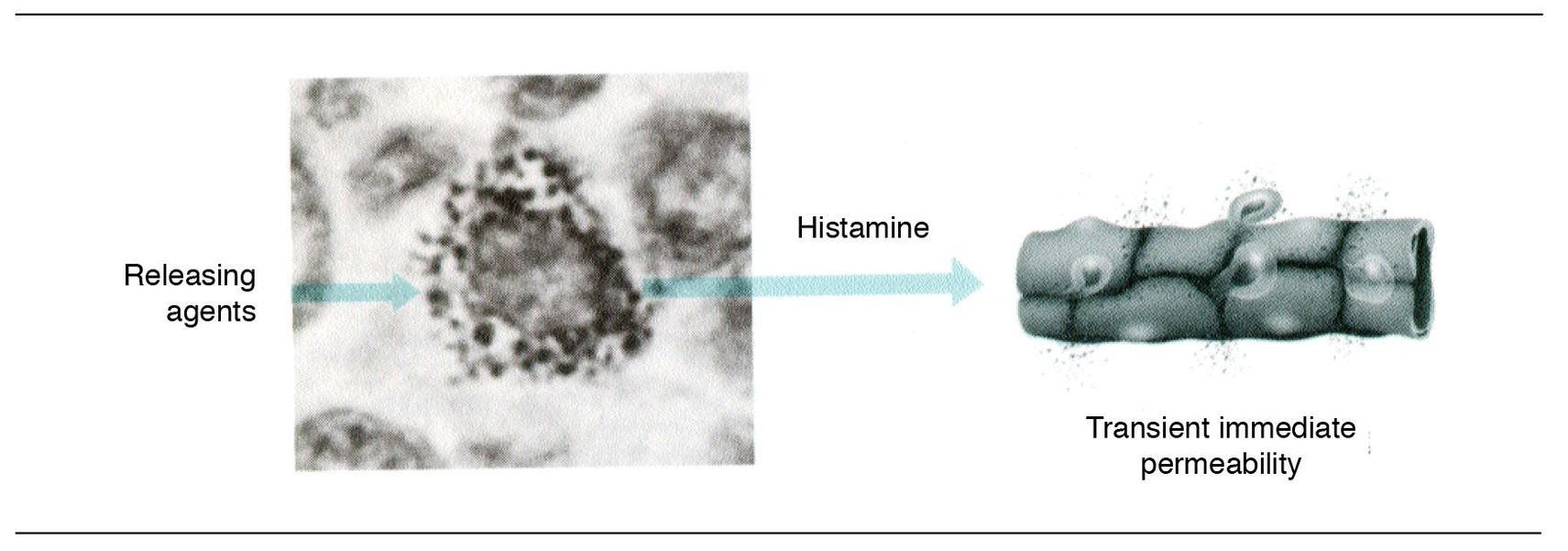
Fig 2-1 Histamine release.
The mediators we will be considering in this chapter include:
- The vasoactive amines histamine and serotonin
- The kinin system
- The fibrinolytic system
- The complement system
- The arachidonic acid metabolites (prostaglandins and leukotrienes)
- Platelet activating factor
- Nitric oxide
- Neuropeptides
- Other mediators
Histamine (“ready to go”)
The functional requirements for the front guard are to be available immediately, be wherever they are needed, and react with initiation of the defensive system—the “call to arms.”
The vasoactive amine histamine is important in the initiation of the early phases of acute inflammation as it mediates the monophasic response of increased vascular permeability. It is stored in the granules of mast cells and basophils as a heparin–protein–histamine complex. Mast cells are widely distributed in connective tissues and are strategically located near venules and cutaneous and mucosal surfaces. Histamine is released when the mast cells degranulate (Fig 2-1) (see p. 66). The mechanism of degranulation will be discussed later.
In order to produce increased vascular permeability, histamine must attach to a receptor, H1, located on endothelial cells. Attachment causes the endothelial cells to contract, thus producing intercellular gaps through which substances can pass.
Histamine is often the first mediator to act, but its action is transient because it is rapidly inactivated. In addition to its effects on blood vessels, it mediates smooth muscle contraction in airways and the gastrointestinal tract and induces nasal mucus production. Agents that are capable of releasing histamine include:
- Mechanical trauma
- Radiant energy
- Ultraviolet radiation
- Bacterial toxins
- Components of the complement system
- Certain proteolytic enzymes released from cells
- Basic peptides from neutrophilic leukocytes
- Certain allergens
What follows here is part of your training in the operations of the defensive system. As in any well-prepared armed service, there is built-in redundancy. Several of these redundant systems will be discussed later. While working through this information, you should also note that some of these redundant systems share mediators and activators, as well as overlap of functions. This makes a lot of tactical sense when you consider that the defensive battle was initiated by a common factor, and so, the reaction to it should be similar.
The kinin system
Bradykinin is capable of (1) inducing arteriolar dilatation, (2) increasing the permeability of venules, and (3) causing pain. Like histamine, bradykinin increases gaps between endothelial cells and causes a transient increase in venular permeability. Bradykinin is formed from inactive precursors (Fig 2-2):
- Kinin production involves a cascade commencing with activation of Hageman factor (factor XII), a key component of the blood clotting system.
- Hageman factor is activated during injury when it binds to negatively charged surfaces in the walls of damaged blood vessels (eg, basement membrane components). Hageman factor can also be activated by proteolytic cleavage by kallikrein and by bacterial lipopolysaccharide (LPS). LPS is also referred to as endotoxin.
- Activated Hageman factor converts prekallikrein to kallikrein. Then kallikrein can activate more Hageman factor. This is an example of one of the many positive feedback loops one finds in inflammatory reactions.
- Kallikrein is a protease that cleaves kininogen, an inactive precursor of bradykinin, to produce bradykinin.
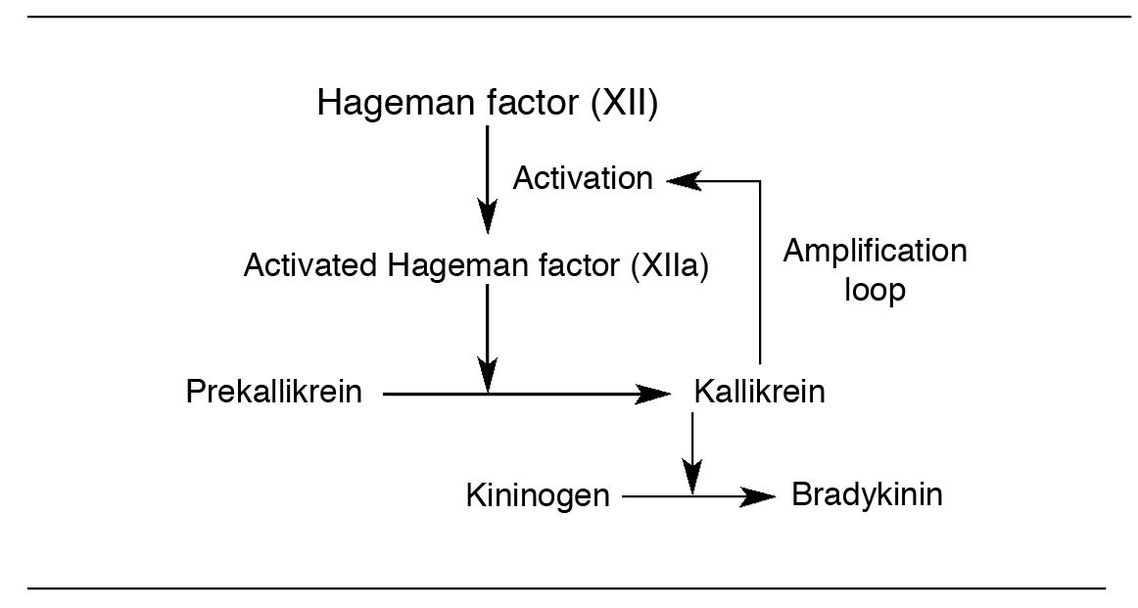
Fig 2-2 Kinin system.
In addition to the production of bradykinin, kallikrein is active in other reactions:
- Activation of plasminogen (see page 23)
- Activation of C1q in the complement system (also coming up)
- Found in plasma, tissues, and secretions, such as saliva
The fibrinolytic system
Following the formation of a thrombus (a blood clot formed during life), the fibrinolytic system (Fig 2-3) is activated to dissolve the fibrin deposit. When fibrin is degraded, fibrin “split products” are formed, and these fibrinopeptides can induce increased vascular permeability. Initiation of the fibrinolytic system involves the activation of a plasma protein, plasminogen, by plasminogen activators (urokinase and tissue plasminogen activator) to generate plasmin, whose basic function is to digest fibrin clots and thrombi.
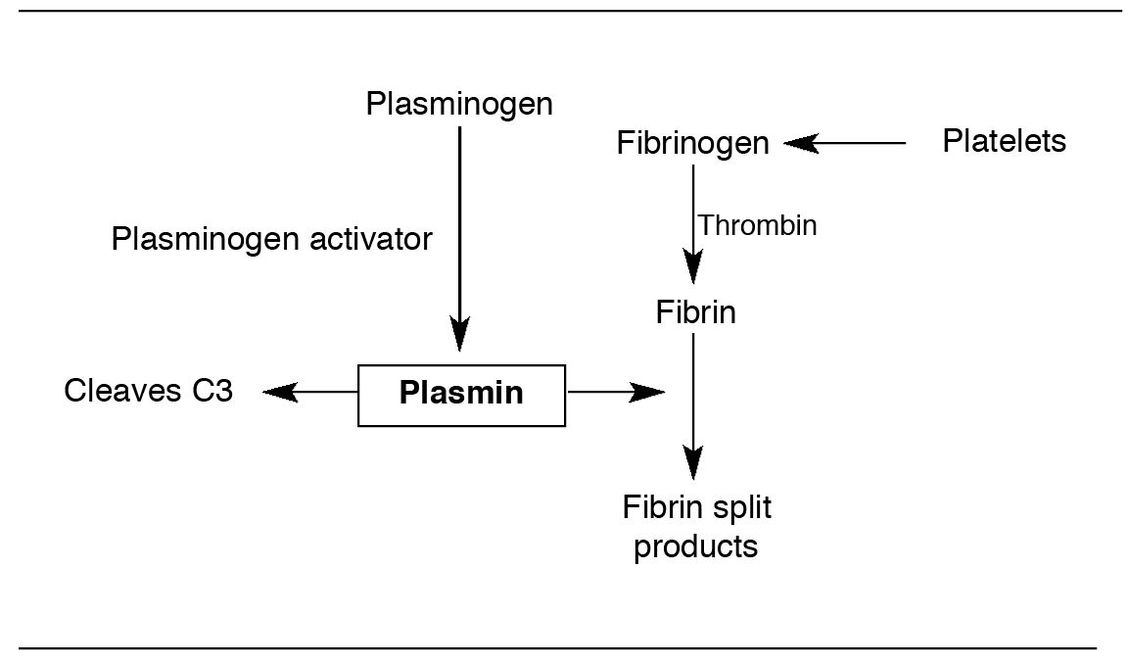
Fig 2-3 Fibrinolytic system.
Prourokinase can be converted to urokinase by kallikrein, thus linking the kinin system to the fibrinolytic system. In this way, it is possible for Hageman factor to start the cascade of events in the fibrinolytic system.
Substrates of plasmin include fibrinogen, fibrin, and prothrombin. Fibrinogen is released from platelets after they adhere to sites of endothelial cell injury. Thrombin causes the conversion of fibrinogen to fibrin. The removal of fibrin is important, as formation of a fibrin thrombus within a blood vessel decreases blood flow, leading to ischemia.
The generation of thrombin promotes platelet aggregation and secretion of inflammatory mediators by platelets, as well as endothelial cells.
In inflammation, plasmin does several important things:
- It can produce vasodilation by generating fibrinopeptides (fibrin split products).
- It can digest fibrin and thus aid in the removal of fibrin deposited during an inflammatory reaction.
- It can split activated Hageman factor (factor XIIa) into subunits that activate prekallikrein to turn on the kinin system.
- It can activate the complement system by cleaving C3 to produce C3 fragments (coming up!).
There are several plasmin activating factors besides urokinase and tissue plasminogen activator:
- Bacterial substances (eg, streptokinase)
- Cell-derived activators (eg, trypsin)
- Macrophage plasminogen activator
- Hageman factor
Note: Plasmin was formerly known as fibrinolysin; this old name is still used for this system.
Advice from some old friends
If you hurried through, or even ignored, the figures associated with the last two sections (see Figs 2-2 and 2-3), you really missed out. In fact, the figures really do explain a lot about these two systems. There are a whole lot of people in Kansas who specifically remember these two systems simply because they took the time to study the figures. If you are from Kansas, we apologize for this delay, please move right on….
Self-test 2-1
- Name a chemical mediator in inflammation that is preformed and stored in cells.
- Name as many mast cell degranulating agents as you can.
- What role does Hageman factor play in the activation of kinins?
- How is Hageman factor activated?
- What is the duration of action of histamine?
- What three mediator systems are associated with plasma proteases?
- What role does tissue damage play in the activation of kinins?
- What is the mechanism of action of bradykinin in inflammation?
- What is the role of plasmin in the vascular response to injury?
- Which substance(s) mediate(s) the so-called immediate transient phase of vascular permeability?
- What is the role of kallikrein in inflammation?
Answers on pages 212–213.
Things may become a little complicated for the next few pages. The reason is that the next two groups of mediators (ie, arachidonic acid metabolites and complement) both have mediator effects on the vascular response, and they do a number of other things in inflammation as well. Remember, the defensive system not only needs to activate the transport system and deliver supplies to the battleground, it also needs to sustain the process and start to get active fighting units “on-line,” in place, and actually fighting, after identifying the enemy of course. We thought we would try to explain the vascular response parts here and hit the other functions later in this book. Unfortunately, it doesn’t break out very cleanly, so you will find “pieces” of things stuck around. It’s not time to ask for a refund yet….
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


