2
Cardiovascular Diseases
I. Background
Description of Disease/Condition
Cardiovascular diseases (CVDs) include a wide spectrum of signs and symptoms, and approximately one in three adults in the United States have more than one CVD at a time. In addition, many CVD patients have other systemic diseases that increase the morbidity and mortality of each disease. There are numerous well-known risk factors (see Table 2.1), and evidence is building to connect periodontal disease and chronic inflammation to CVD.1–3 It is important for patients with CVD to have optimum oral health to reduce the potential for pain that in turn may elevate endogenous epinephrine and add stress to the cardiovascular system. CVD pain may also be confused with pain of dental origin.
Table 2.1. Risk Factors for Cardiovascular Disease
| Modifiable | Nonmodifiable |
| High blood pressure Atherosclerosis/dyslipidemia Diabetes Tobacco smoking Obesity/diet Inactivity Stress Alcohol use |
Age Sex Family history |
Pathogenesis/Etiology
Ischemic heart disease is defined as a lack of oxygen to the heart muscles. It can be caused by coronary artery blockage by atherosclerotic plaque or thrombosis, narrowing because of coronary artery spasm, coronary arteritis, embolism, or shock secondary to hypotension. Other causes of ischemia include tachycardia, hyperthyroidism, catecholamine treatment, cardiac hypertrophy, anemia, advanced lung disease, congenital cyanotic heart disease, and carbon monoxide poisoning.
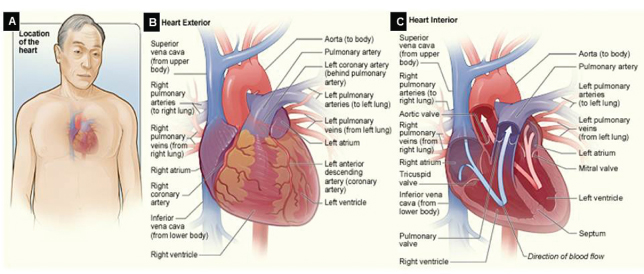
Coronary artery disease (CAD) specifies inadequate blood supply to the blood vessels in the heart: the left coronary artery (LCA) divides into the left anterior descending (LAD) and left circumflex (LCX) arteries; and the right coronary artery (RCA). See Fig. 2.1. Symptoms may include fatigue, shortness of breath, or none at all.
Figure 2.1 The healthy heart.
Source: National Heart Lungs and Blood Institute. Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/hhw/anatomy.html. Accessed December 28, 2011.
(A) Location of the heart in the body. (B) Front exterior surface of the heart, including the coronary arteries and major blood vessels. (C) Internal cross section of a healthy heart. Blue arrow shows venous blood and red arrow shows arterial blood flow pattern.
Angina pectoris (AP) is defined as sudden-onset, substernal, or precordial chest pain due to myocardial ischemia, but without infarction (necrosis). The pain often radiates to the left arm, neck, jaw, or back. Angina is classified as stable, unstable, or Prinzmetal angina:
- Stable angina is predictable, induced by exercise or exertion, and lasts for less than 15 minutes.
- Unstable angina can occur at any time, is more severe, and lasts longer.
- Prinzmetal angina occurs at rest, with electrocardiogram (ECG) changes, and is most likely due to spasm of a coronary artery.
Other less common causes of angina include aortic stenosis, arrhythmias, myocarditis, mitral valve prolapse, and hypertrophic cardiomyopathy.
Myocardial infarction (MI), or acute myocardial infarction (AMI), occurs after persistent ischemia leads to irreversible coagulative necrosis of myocardial fibers. The area of infarct loses normal conduction and contraction, and may heal with nonfunctional scar tissue. Most MIs involve the left ventricle, or by extension, to the right ventricle. Symptoms are severe substernal pain that may radiate to the left arm, neck, jaw, or back; shortness of breath; profuse sweating; loss of consciousness; or symptoms may be only very mild discomfort.
MIs are evaluated using two criteria: depth and location. If the infarct involves the full thickness of the ventricular wall, it is termed transmural; a subendocardial infarct is limited to the inner one-third to one-half of the ventricular wall. Location is reported by wall or coronary artery involvement, for example, antero-septal infarct, left ventricular anterior wall infarct, and LAD coronary infarct. Clinical evaluation of patients with MIs by ECG shows two types: those with ST elevation (STEMI) or non-ST elevation (non-STEMI).4
Acute coronary syndrome (ACS) is a relatively new term that is gaining favor. It is used to describe patients with unstable angina, STEMI, or non-STEMI. The pain associated with ACS is more severe and prolonged than AP, and signifies a worsening of the CVD.5
Hypertension (HTN) is a disease that has been defined as systolic blood pressure (BP) above 140 mmHg and/or diastolic BP above 90 mmHg. HTN is also a risk factor in many diseases, including CVD, stroke, renal failure, and heart failure (HF). The great majority of patients with HTN (90%) have no primary cause, thus the term essential HTN. The remaining 10% have an identified etiology such as pheochromocytoma, aortic regurgitation, renal artery stenosis, and preeclampsia, or are drug-induced by corticosteroids, nonsteroidal anti-inflammatory drugs, or oral contraceptives. Sustained HTN may lead to hypertrophy of the left ventricle to compensate for the elevated pressure. Symptoms may be nonexistent, or cause dizziness or headache, nosebleeds, and fatigue:
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) published HTN guidelines in 2003.6 The 8th report is expected to be more evidence based and published in 2012. The term prehypertension was introduced to draw attention to those patients whose BP was at increased risk of developing into HTN. This classification of systolic BP 120–139 mmHg and/or diastolic BP 80–89 mmHg was developed to encourage people to adapt healthy lifestyles. Dentists were specifically included in this report to help with surveillance, as most patients with HTN may have no symptoms. The earlier that patients can be diagnosed and treated, the less the extent of lasting effects7:
- normal BP for adults = <120/80 mmHg;
- prehypertension = 120–139/80–89 mmHg;
- stage 1 HTN = 140–159/90–99 mmHg;
- stage 2 HTN = >160/100 mmHg.
Heart failure (HF) occurs when the heart can no longer maintain circulation that is adequate for body tissues to function. Congestive HF describes the clinical signs of pulmonary and/or peripheral edema in addition to the inadequate circulation. Symptoms may include shortness of breath, orthopnea, fatigue, and inability to cope with physical activity.
The pathophysiology has two components:
- Due to myocardial ischemia or CAD; cardiomyopathy; myocarditis; stiff or rigid ventricles; pericardial effusion or tamponade; or severe rhythm disorders, for example, ventricular tachycardia, atrial fibrillation, or flutter.
- Due to atrial or mitral regurgitation or ventricular septal defect resulting in increased peripheral resistance and increased volume load.
- Due to anemia, obstructive or restrictive pulmonary disease, or thyrotoxicosis preventing blood from efficiently oxygenating all tissues.
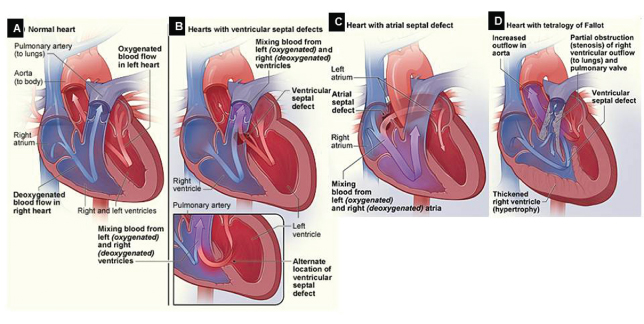
Congenital heart disease or defects are evident from birth. See Fig. 2.2. These are structural problems that range from minor holes between chambers to major malformations that require surgical intervention. Some examples include atrial–septal defects, patent ductus arteriosus, atrioventricular (AV) septal defects, tetralogy of Fallot, transposition of the great arteries, hypoplastic left heart syndrome, and coarctation of the aorta.
Figure 2.2 Congenital heart defects. (A) Normal heart. (B) Ventricular septal defect. (C) Atrial–septal defect. (D) Tetralogy of Fallot.
Source: National Heart Lungs and Blood Institute. Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/chd/types.html. Accessed December 28, 2011.
Valvular heart disease is characterized as stenosis or insufficiency:
- Stenosis means that the opening of the valve is reduced compared with normal. This limits the amount of blood volume that is able to pass through the valve.
- Some causes are fibrosis of the valve opening secondary to rheumatic heart disease, calcification of the valve leaflets, and congenital malformation of the valve leaflets.
- Insufficiency means that the valve fails to close completely. This leads to regurgitation of blood in the reverse direction of normal.
- Some causes are prolapse, ruptured papillary muscles, left ventricular hypertrophy, infective endocarditis (IE), Marfan syndrome, systemic lupus erythematosis, and congenital malformation.
Infective endocarditis (IE) is defined as microbial infection and inflammation of the endocardium including the heart valves. Damage to the valve leaflets may be part of the cause and the result of this condition. Vegetations form on the valves that consist of organisms, usually streptococci or staphylococci, fibrin, and inflammatory cells. Erosions, valve perforations, and abscesses in the myocardium can occur. Symptoms are similar to HF. Most patients recover from the infection, but injury to one or more valves persists. Rarely, other complications result, for example, septic emboli to the brain, spleen, or kidneys. In 2006, approximately 2400 U.S. adults died due to IE.8
Dysrhythmia or arrhythmia is a disruption of the electrical impulse generation or conduction in the heart that leads to an abnormal function. The disruption may be due to an area of infarction, ischemia, electrolyte imbalance, or medication. Some examples include atrial fibrillation, tachycardia, paroxysmal supraventricular tachycardia, and ventricular fibrillation. Many patients have no symptoms of arrhythmia; however, some patients have HF secondary to the arrhythmia with symptoms that can be very severe.
Epidemiology
It is estimated that about 86,600,000 U.S. adults (over age 20) have one or more types of CVD. This is approximately one of three adults8:
- 40,400,000 are over age 60 years;
- 76,400,000 have high BP;
- 16,300,000 with coronary heart disease;
- 7,900,000 have had an MI;
- 9,000,000 experience AP;
- 5,700,000 have HF;
- 650,000–1,300,000 have congenital cardiovascular defects.8
CVD accounts for about 40% of all deaths in the United States, of which 90% result from ischemic heart disease. In 2007, there were 813,800 deaths caused by CVD.8
 Coordination of Care between Dentist and Physician
Coordination of Care between Dentist and Physician
Patients with CVD will need elective and urgent dental care. The dentist must be able to ask the right questions of the physician regarding the patient’s ability to tolerate the stress of dental treatment, as well as understand the information provided by the physician. Certain medications have oral adverse drug reactions that can be managed by the dentist. Other medications cause increased bleeding. For patients with acute or severe CVD, hospital-based dental care may be necessary.
For some patients, the dentist may observe signs of CVD during a dental appointment. Reviewing the patient’s medical history and measuring the BP and assessing the heart rate and rhythm (pulse) may identify contraindications or the need for modifications in the provision of dental care. Moreover, these processes may reveal inadequate control of existing medical conditions or the onset of new problems. The dentist should feel confident in contacting the physician regarding these findings.9 A patient with poorly controlled CVD, and/or who does not follow his physician’s guidance or adhere to prescription medication regimens should not have elective dental care.
 II. Medical Management
II. Medical Management
Identification
People who have CVD may have very distinct signs and symptoms, or conversely may have no awareness of the problem. Many cases of CVD develop very insidiously so that patients are unaware of the severity until a catastrophic event happens. Ideally, everyone would have simple tests related to the cardiovascular system done on a regular basis: BP measurement, ECG, stress test, blood lipids, blood chemistry, and so on. Unfortunately, many U.S. adults have multiple risk factors that increase the incidence and prevalence of CVD including smoking, obesity, poor diet, and physical inactivity.8
Medical History
The patient who knows that he or she has CVD should identify his or her specific problems upon review of his or her medical history. Other observations may lead the dentist to understand the severity of the problems, and the degree of control or management of the problem:
- elevated BP,
- irregular or abnormal heart rate,
- abnormal respiratory rate,
- shortness of breath upon exertion,
- patient is uncomfortable in supine position,
- surgical scars,
- prolonged bleeding/easy bruising.
Reviewing the patient’s list of medications can lead the discussion to clarify the specifics of the type of CVD. Also, by understanding the pharmacological category of each drug on the patient’s list, the dentist can deduce how difficult the CVD is for the physician and patient to manage; that is, a patient who takes four different types of antihypertensive medications has a very difficult time controlling his or her disease.
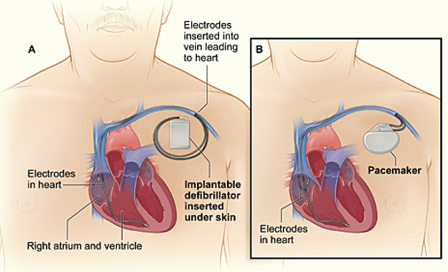
Surgical or cardiac procedural history will reveal patients who have received coronary artery angioplasty and stents, coronary artery bypass grafts (CABG), heart valve repair or prosthetic valve replacements, repair of congenital heart defects, removal of excess heart muscle (e.g., ventricular septal myotomy or myectomy), pacemakers or implantable cardioverter-defibrillator (ICD) (as shown in Fig. 2.3), or heart transplantation.
Figure 2.3 Implantable cardioverter-defibrillator (ICD) and pacemaker. (A) Location and general size of an ICD. (B) Location and general size of a pacemaker. For each device, the wires with electrodes on the ends are inserted into the right atrium and ventricle through the cephalic vein or subclavian vein in the upper chest.
Source: National Heart Lungs and Blood Institute. Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/icd/. Accessed December 28, 2011.
Physical Examination
Many patients with CVD are managed by their primary care physician or by an internist. For more severe cases, a cardiologist and/or cardiothoracic surgeon may be involved. Physical examination by the medical team may include BP, heart rate and rhythm, respiratory rate and volume, chest auscultation, ECG, echocardiography, stress test with or without radioactive agents, radiograph, magnetic resonance imaging, computed tomography (CT), cardiac catheterization, and angiography. Ejection fraction (EF) is a measurement (estimated on echocardiogram or other tests) of the degree of HF. When the left ventricle contracts, there is residual blood remaining in the chamber. Normal EF is 50–70%, and heart transplant may be considered when EF is <25%.
When treating the patient with CVD, the dentist should check the BP and heart rate before any invasive procedures, and before injecting local anesthetic. Comparing these data with baseline values may reveal a disease t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


