Chapter 19
The supraclavicular artery island flap
The supraclavicular island flap has only recently gained popularity as a definitive option in head and neck reconstruction. The beginnings of this flap date back to Kazanjian and Converse when they described the acromial flap or “in Charretera”.1 Since this description, there has been a significant improvement in the understanding of the regional anatomy, which has led to a more predictable and robust flap. The step towards better understanding of the supraclavicular flap began with the publication of Lamberty and Cormack2 where they described the vascular anatomy of the flap and demonstrated its reliability. The supraclavicular flap continued to exist in the surgical background without gaining a foothold in the reconstructive options of most surgeons. Pallua and his colleagues are credited with the first description of the flap as a “supraclavicular artery island flap”3 and with a modification which eventually helped the establishment of this flap as a true contender in head and neck reconstruction. Since this description, there have been several publications in the literature describing the reliability of the flap in several options for reconstructing head and neck defects as well as in the anterior chest region.
The supraclavicular flap has several advantageous properties which has rendered it a preferred flap for the reconstruction of the lower face and neck for many reconstructive surgeons. One of the main advantages is that it is a thin and pliable flap. This property allows it to be used in situations where there is a need for resurfacing of the face or neck without the added bulk encountered in myocutaneous flaps. An additional advantage is that it also provides a very similar color match to the defect area and has a similar texture. The pliability of the flap allows it to be tubed when needed for pharyngeal reconstruction as well as for the reconstruction of stomal defects in cases where there is a soft tissue defect above or below the stoma following ablation of stomal recurrences. The supraclavicular flap is an easy flap to harvest. In the hands of experienced surgeons, the average time to raise the flap is less than one hour.4,5 Additionally, the supraclavicular flap remains a viable reconstructive option even in patients who have undergone a previous neck dissection.6 The use of this flap in the multiply operated and often vessel-depleted neck makes it a very attractive option for these challenging cases.
The supraclavicular island flap has relatively few disadvantages. The main one is that the quantity of tissue available for transfer is restricted to what can be harvested while still allowing for primary closure. Another disadvantage related to the tissue available for harvest is the length of the flap. The ideal is to not travel beyond the insertion of the deltoid muscle as this will begin to render the tip of flap more dependent on random perfusion and thus susceptible to ischemia and necrosis.
Anatomy
The main blood supply to the flap is the supraclavicular artery which is a branch from the transverse cervical artery. The artery can be found in a triangle formed by the sternocleidomastoid muscle, the external jugular vein, and the clavicle. The artery exits 3.0 − 0.7 cm above the clavicle at a distance of 8.2 ± 1.7 cm from the sternoclavicular joint and approximately 2.1 ± 0.9 cm dorsal to the sternocleidomastoid muscle.7 The mean diameter of the artery is 1.5 mm.
The venous drainage to the flap consists of two veins. One runs along the artery as a venae commitantes and eventually drains into the transverse cervical artery, while the other is a branch of the external jugular vein and drains into the subclavian vein.
The skin area that can be harvested with this flap ranges from 10–16 cm wide to 22–30 cm long. The distal end of this flap can extend to the midportion of the deltoid with a slight anterior placement. The design of the skin flap is usually fusiform.
Flap harvest
The flap harvest is depicted in Figures 19.1 to 19.10.

Figure 19.1 View of exposed mandible with ORN in a previously operated and radiated patient.
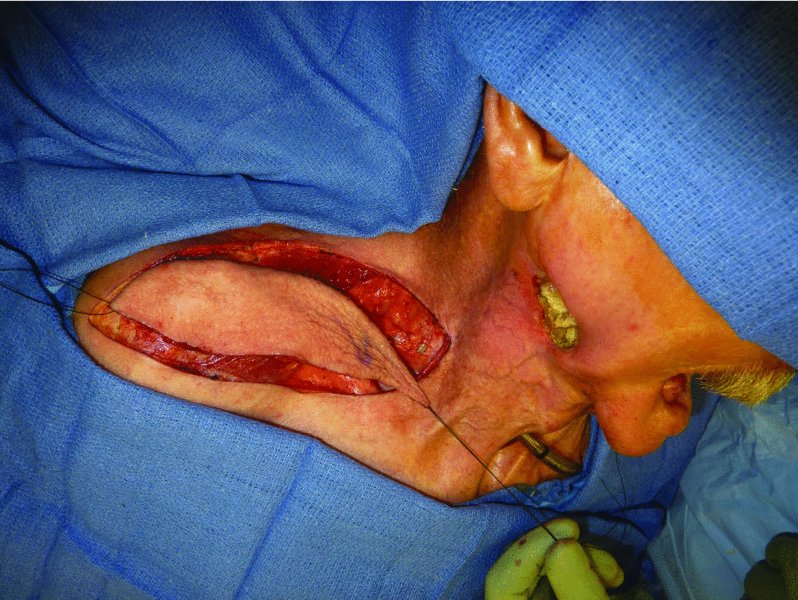
Figure 19.2 Elevation of a supraclavicular flap prior to transfer.

Figure 19.3 Elevation of the supraclavicular flap.

Figure 19.4 Exposure of the vascular pedicle of the supraclavicular flap.
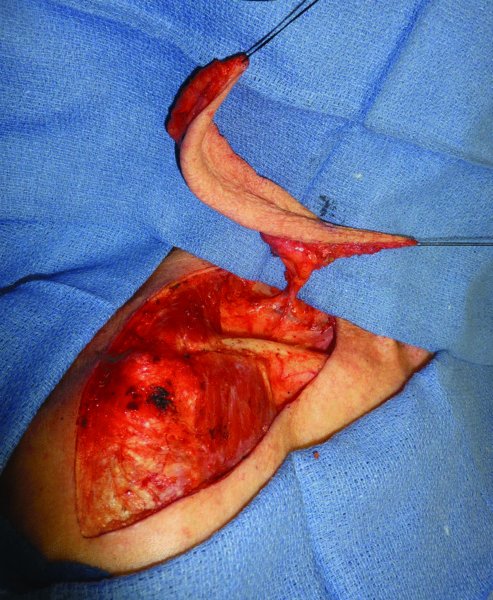
Figure 19.5 Dissected vascular pedicle demonstrating good length of the pedicle.
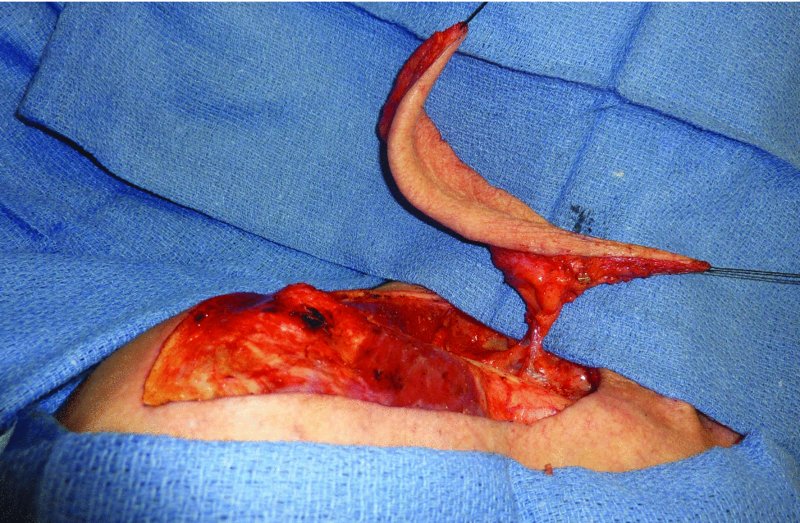
Figure 19.6 Another view of the vascular pedicle to the supraclavicular flap.
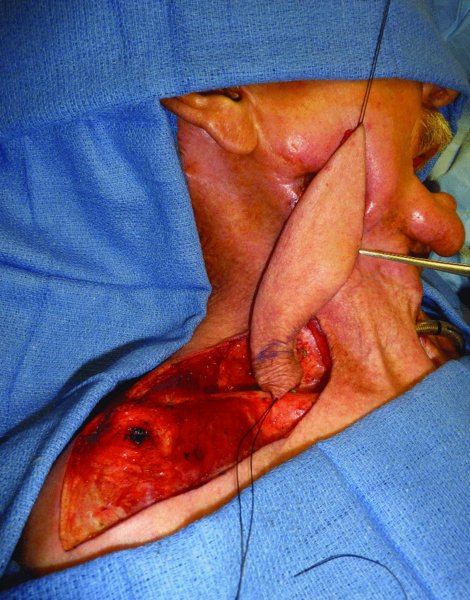
Figure 19.7 Assessment of the rotation of the flap towards the defect.

Figure 19.8 Inset of the flap, repairing the skin defect and providing coverage for the mandible.

Figure 19.9 Early postoperative view of the reconstruction.
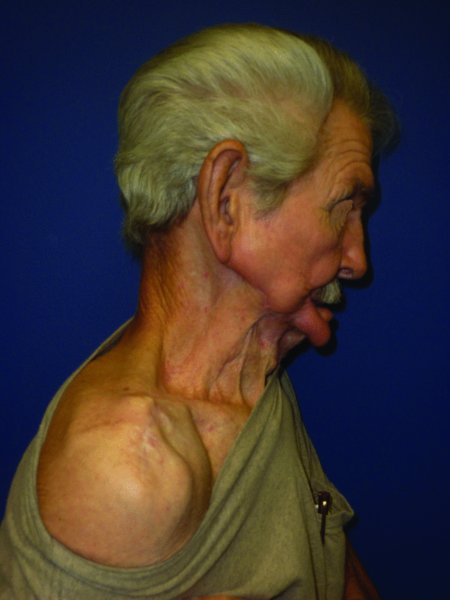
Figure 19.10 Late postoperative view of the reconstruction; note the excellent color match.
The patient is positioned in a lateral decubitous position or supine with a roll under the ipsilateral shoulder. The defect area is measured and the shape of the defect is noted and transferred to the ipsilateral shoulder directly overlying the angiosome of the flap. Using a handheld Doppler, the main pedicle is identified and traced both laterally as well as medially towards the transverse cervical artery and the thyrocervical trunk.
- The elevation of the flap begins from the distal to the medial direction.
- An incision is made at the distal tip of the flap and deepened to the fascia overlying the deltoid muscle.
- A subfascial dissection is elevated in a medial approach towards the mid-third of the clavicle.
- At this region, some deltoid perforators to the skin may be encountered. These perforators can be divided with bipolar cautery.
- Completion of the skin incision is performed circumferentially along the skin island. Care should be taken not to extend the incision deeper than the subcutaneous tissue so the vascular pedicle is not injured.
- The vascular pedicle may be seen coursing through the skin island if transilluminated.
- Dissection is continued in a medial direction in a combination of blunt and bipolar dissection.
- Once the vascular pedicle is identified, a large dominant vein and a smaller venae commitante may be seen; if the second vein from the external jugular vein is limiting the arc of rotation, a decision to sacrifice it can be made after placing an Auckland clamp on it and waiting several minutes to see if venous congestion develops on the skin flap.
- As the dissection proceeds medially and posteriorly, a small artery and vein may also be encountered; this is often the dorsal scapular artery and again, if it is limiting the arc of rotation, it too can be ligated and divided.
- Once the flap is elevated and there is sufficient pedicle dissection, adequate tension-free rotation of the flap to the defect should be checked. If the flap is able to reach the desired defect without any impediment, then dissection is complete. If there is tension or need for further reach, an attempt can be made at further freeing any restriction to the rotation and advancement of the flap along the base of the pedicle.
- The transfer of the flap to the defect side can be made by a releasing skin incision along the bridge of skin between the donor site and the defect site or, if chosen, the flap can be tunneled to the recipient site.
- In cases where a tunneled flap is chosen, particular careful needs to be taken when de-epithelializing the skin so the entire flap is not compromised. Equally important is the adequate development of a wide unrestricting tunnel. If the tunnel is too narrow, it can cause compression of the flap and potentially lead to flap loss.
- The closure of the donor site can nearly always be done primarily. Only in rare circumstances will there be a need for skin grafting.
- Prior to closing the defect, the tissues anteriorly as well as posteriorly should be widely undermined. The undermining should frequently reassessthe advancement of the two skin edges to enable closure without significant tension.
- The inset of the flap is carried out as dictated by the defect site.
Special circumstances
One of the best properties of the supraclavicular artery island flap is not only the color and texture but the thickness of the flap. This makes it an ideal flap in circumstances where a large volume of thin, pliable tissue is needed for resurfacing of the neck or face, particularly in burn contracture patients. Given that the maximum width that can be harvested from the donor site and that still allows closure is 16 cm, in cases where a greater volume of tissue is needed, consideration should be given to pre-expansion of the tissue.
The supraclavicular tissue is expanded until the desired amount of tissue is obtained. Once the expansion is complete, the patient is taken back to the operating room for the definitive reconstruction. The pseudocapsule on the undersurface of the expanded tissue is removed and the remainder of the flap harvest is executed as previously described.
Advantages
The advantages of the supraclavicular artery island flap are several. The color and texture of the skin is very similar to the surrounding area which makes it a great option for reconstructing regional defects of the head and neck. Additionally, the lack of hair on this region also renders it a good option to reconstruct non-hair bearing regions of the head and neck. The supraclavicular island flap also has the added advantage of ease of harvest, usually taking less than one hour to elevate the flap. Also, the donor site can be easily concealed with everyday clothing. These facts and the reliability of the flap, render the supraclavicular artery island flap one of the key options for the reconstruction of defects on the neck and lower face.
Disadvantages
The main disadvantage of this flap is in fact one of its advantages, that is, it is a thin flap. Often when reconstructing oncologic defects in the head and neck region, additional tissue bulk is desired to restore the defect site. Given that this is a fasciocutaneous flap, it does not allow for a true re-establishing of the lost bulk. Also, the limited quantity of tissue available for transfer without pre-expansion can be a disadvantage in certain situations.
Complications
The most feared complication of this or any other flap is the partial or full loss of the skin paddle. Bearing in mind that this is a regional axial pattern flap, the distal portion of the skin island is most at risk for ischemia and loss. In cases where the viability of the flap is in question, the surgeon may choose to trim the distal portion until viable bleeding tissue is encountered.
In patients previously treated with radiation therapy for their head and neck malignancies, the donor site may pose some additional problems. The most commonly encountered complication in this scenario is deh/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


