Chapter 19 Single-Tooth All-Ceramic Restorations
Material Options
Pressable Glass Ceramics
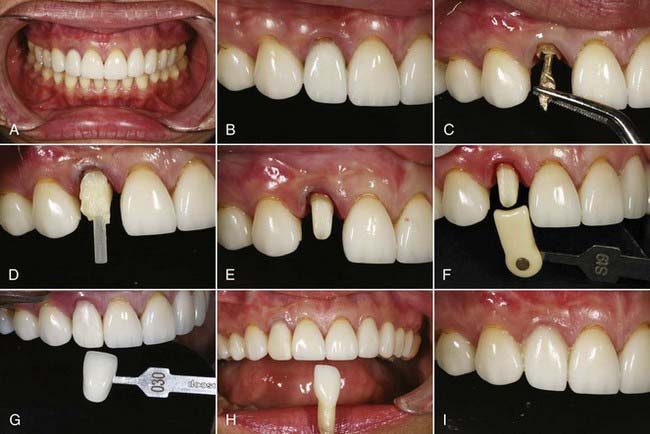
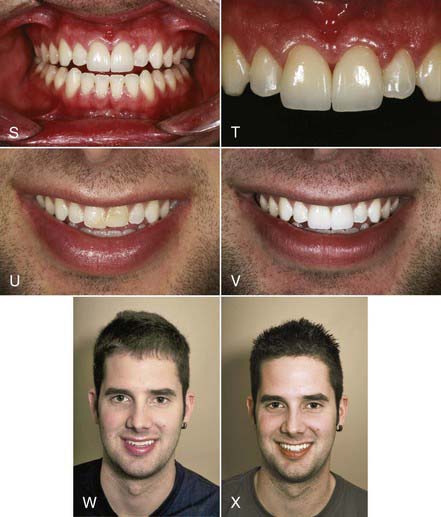
Materials such as these, with low strength, are best used in the anterior region. The strength of these restorations is supplemented by etching the internal surfaces with hydrofluoric acid, silanating, and bonding to treated tooth structure with resin cements (Figure 19-1).
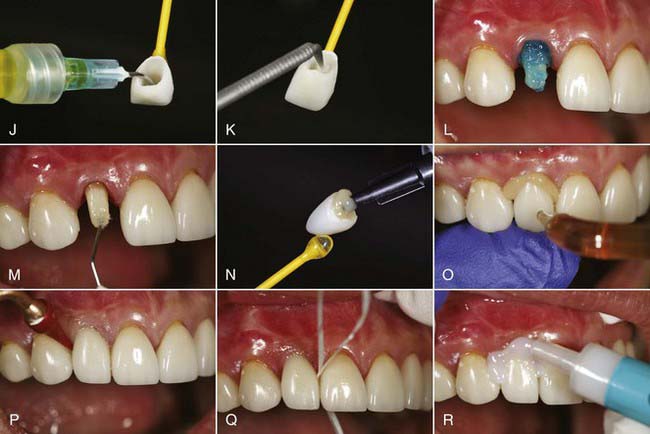
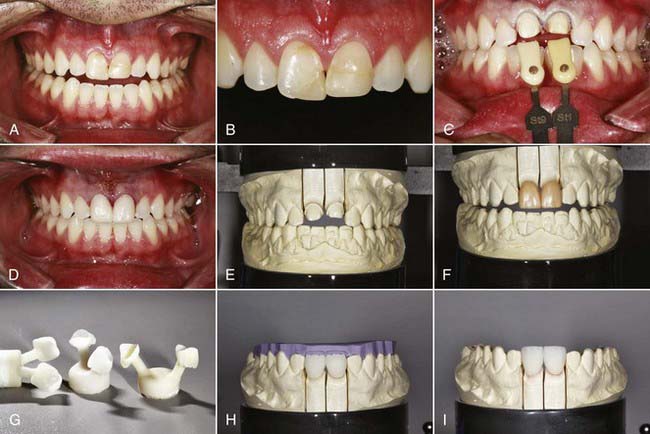
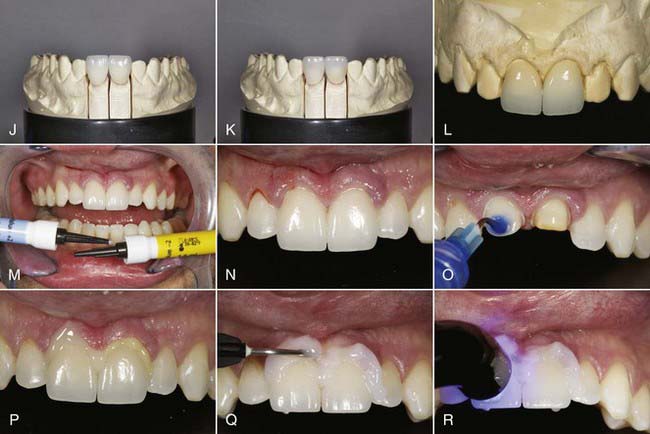
Like the LRGCs, the LDGCs have many indications and uses. The pressable lithium disilicate material (IPS e.max Press) is indicated for inlays, onlays, partial crowns, thin veneers, veneers, anterior and posterior crowns, three-unit anterior bridges, three-unit premolar bridges, telescope primary crowns, and implant restorations. In some cases in which minimal or no tooth preparation is desired (e.g., thin veneers), laboratories are able to press restorations as thin as 0.3 mm while still ensuring a strength of 400 MPa. Indications for the machinable lithium disilicate material (IPS e.max CAD) are inlays, onlays, veneers, partial crowns, anterior and posterior crowns, telescope primary crowns, and implant restorations. For a posterior crown fabricated to full contour using CAD methods, lithium disilicate offers 360 MPa of strength through the entire restoration. As a result, restorations demonstrate a “monolithic” strength unlike any other metal or metal-free restoration. With a flexural strength four times greater and a fracture toughness almost two times greater than those of LRGC, it is no wonder that use of LDGC core material in both its pressable and CAD-CAM versions (IPS e.max Press, IPS e.max CAD [Ivoclar Vivadent]) has grown in popularity (Figure 19-2).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses