18
Planning and Placing Temporary Anchorage Devices with the Aid of Cone Beam Computed Tomography Imaging
Introduction
Advances in medicine usually are driven by new developments in other basic sciences, which then are adapted to medical use. After a new technology has been used successfully in the medical field, it often finds its way into dentistry. Three-dimensional (3D) craniofacial imaging using cone beam computed tomography (CBCT) technology is no exception. Dental implantologists were early adopters of 3D CBCT imaging (Benjamin, 1987; Weinberg, 1993; Cavalcanti et al., 2002). This should come as no surprise, since it can be beneficial to have maximum information on a given implant site to ensure that the implant is placed in the most ideal spatial relationship to the surrounding anatomical structures of relevance with the goal of improving the treatment outcome.
The same rationale can be applied to use of orthodontic miniscrew implants and other endosseous temporary anchorage devices (TADs). However, the simple fact that a certain technology such as CBCT or treatment approaches such as TADs are available does not mean these have to be used on a routine basis. The only way to decide if and when a certain procedure should find application in the diagnosis and treatment of patients is by conducting a diligent risk (cost)-benefit analysis as discussed in Chapters 1 and 6 and as described previously (Pochin, 1982; Zarin & Pauker, 1984; Cassidy et al., 1993). It is the purpose of this chapter to illustrate if and when 3D imaging with CBCT technology should be used for planning and placing endosseous orthodontic TADs, and how best to utilize CBCT-based information for refined diagnosis and treatment planning for TADs.
Advantages and Disadvantages of CBCT Imaging for TAD Application
This part of the chapter is not intended to be a complete disquisition of the general advantages and disadvantages of CBCT imaging, which are discussed elsewhere in this book (Chapters 1 and 6), but is simply a brief overview of the important factors to consider when deciding if image acquisition with this technology is appropriate for placing TADs in the specific case at hand.
Advantages
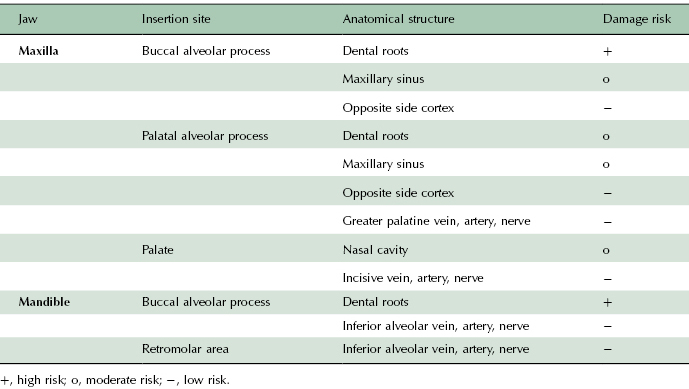
When placing an endosseous orthodontic TAD, the objective is to anchor the miniscrew securely in the surrounding bone and to avoid any damage to adjacent anatomical structures (Table 18.1). In other words, the miniscrew needs to be navigated through a volume of bone that is restricted by certain anatomical boundaries, which should not be violated by the implant. Depending on the selected insertion site, those spatial restrictions can be more or less pronounced. Some sites, such as the palate, come with only a single boundary in one direction, that is, the floor of the nose in the cranial direction. Other sites, such as the maxillary buccal alveolar process, for example, will come with mesial and distal limitations in terms of dental roots, with a lingual boundary in terms of the lingual cortex of the alveolar process and even cranial and caudal boundaries in terms of the maxillary sinus and dental roots or the alveolar crest, respectively. Obviously, the more boundaries that an insertion site has, the greater the level of precision required for a successful insertion and the greater the degree of difficulty of the insertion.
Table 18.1 Anatomical structures that may be at risk during a miniscrew implant insertion.
Without a doubt, it seems beneficial to visualize the different boundaries of a given insertion site, for only if it is known where the obstacle lies can you predictably avoid it. Plain film radiography does not afford that possibility. In the example of the maxillary buccal alveolar insertion site using a periapical or panoramic radiograph, the buccal and lingual surfaces are invisible and the mesial and distal boundaries may be prone to distortion. The same applies for the cranial and caudal boundaries. These limitations arise from the 2D nature of plain film radiography: structures lying in various planes all are depicted on the radiograph as lying in one plane of space (Figure 18.1).
CBCT technology overcomes these limitations. It is possible to view all aspects of the insertion site on the computer screen, virtually, noninvasively, as though you are dissecting your actual patient. Modern software packages generally provide various perspectives that usually are customizable and adjustable based on the clinician’s preference. It is possible to view a 3D model (volumetric view) of the entire scanned object or only parts of it or to create tomographic slices in all three planes of space and navigate through the volume in increments of designated thicknesses, which also are customizable (Kau et al., 2005).
Going back to the example of the complex insertion site, CBCT technology allows an exact visual identification of the location, shape, and divergence of the mesial and distal dental roots, the floor of the maxillary sinus, and the buccal and lingual wall of the alveolar process. Qualitative assessments, therefore, can be made with much greater accuracy than on a regular 2D radiograph. Also, in contrast to plain film radiographs, CBCT data can be quantified using the appropriate software packages. Thus distances between two points such as interradicular distance or buccal bone thickness can be measured with considerable accuracy (Timock et al., 2011); angulation between three points can be calculated (e.g., to determine root divergence); and the density of objects including bone can be assessed (Marquezan et al., 2012). This additional information allows for a more detailed approach to planning and placing of the miniscrew implants. The use of this information in placing TADs will be discussed in the following section of this chapter.
Disadvantages
As can be expected, there are few disadvantages of CBCT imaging that relate directly to the planning and placement of an orthodontic miniscrew implant. More information can be helpful if used properly. Besides the general caveats of CBCT imaging noted elsewhere (see Chapters 1 and 6), which require a careful assessment of risk to benefit for each case prior to scanning for TAD placement, the only major disadvantage is that a large amount of information provided by the CBCT can lead to confusion or, even worse, may provide a false sense of security and override the clinical chairside assessment for inexperienced clinicians.
The transfer of the information obtained on the virtual model to the real patient also can be difficult. Imagine a runner that mapped a 5-mile run on his computer using one of the readily available mapping services, but then failed to take the exact route he or she had designed at the runner’s computer once the run is begun. The reasons might be plentiful and the deviation could be attributed to distraction, confusion, false landmark identification, or imprecision—but the final result will be the same: the runner potentially either will run too far or will end up short. The same applies to the insertion of a miniscrew implant. Having all the information at the computer still does not guarantee a proper insertion, as many confounding factors can come into play, which can be referred to as the “virtual reality gap.” How to mitigate the effect of such confounders will be explained in the section on evaluation of macroanatomical structures of this chapter.
Approaches for Optimal Clinical Utilization of CBCTs for TADs
CBCT Imaging Protocol for TAD Placement
Unless a large field of view (FOV) CBCT scan is needed for other purposes such as in individuals with skeletal discrepancies, asymmetries, or craniofacial anomalies (see Chapters 1 and 8), generally a small FOV, high resolution scan is recommended for placement of TADs. The image then should be utilized preferably in an interactive manner rather than as 2D printouts to define boundary conditions, to determine the location and angulation of insertion, to assess cortical dimensions and quality, and to derive an optimal treatment plan. Typically, a routine radiograph should suffice post-operatively to determine that the TAD has been placed in the desired location and does not impinge on other anatomical structures such as dental roots.
Macro- and Microanatomical Determinants for Successful TAD Insertion
We now will focus on the specifics of treatment planning for orthodontic miniscrew implant placement, which includes discussing how CBCT-generated information impacts the utilization of TADs in practice.
In order for an orthodontic miniscrew implant to be stable, it should be placed clear of dental roots and other sensitive anatomical structures, which forms the basis for macroanatomical diagnosis for TADs. Additionally, it needs adequate primary and secondary stability that, in turn, requires intimate contact between the bone and the implant surface immediately upon insertion and over the long-term duration of the miniscrew use, respectively. This stability likely is dependent on the microanatomical bone phenotype.
Evaluation of Macroanatomical Structures to Minimize Adverse TAD Placement
Several anatomic structures may pose challenges to or limit the placement of TADs. These include dental roots, nasomaxillary cavities, nerves, and blood vessels. The limitations posed by these structures are discussed below together with strategies to minimize potential damage to or encroachment on these structures.
Dental Roots
While it theoretically seems necessary to avoid the dental roots during a miniscrew insertion, the long-term sequelae for the roots are less detrimental as might be assumed (Kim & Kim, 2011). However, multiple publications have suggested that in terms of miniscrew stability and success, contact of the implant to the dental root substantially increases the likelihood of failure (Kuroda et al., 2007; Asscherickx et al., 2008; Chen et al., 2008). Contact of the miniscrew and the roots of the adjacent teeth, hence, should be avoided under all circumstances.
Various studies have provided recommendations for suitable interradicular implant sites based on 3D imaging of either dry skulls or live untreated human jaws (Poggio et al., 2006; Hu et al., 2009; Kim et al., 2009; Monnerat et al., 2009). Because of differences in findings of various studies, the contradictory or conflicting conclusions and recommendations can be confusing to the practitioner. A major shortcoming of all these studies is clearly that root morphology can be extremely variable, rendering averages less useful. Also, the majority of miniscrews seem to be placed after the leveling and alignment phase of treatment, where root divergence or convergence can be introduced iatrogenically, creating a situation that has little relationship to the pre-treatment situation. It seems sensible, therefore, to perform pre-insertion imaging of the interradicular implant site to verify its suitability for TAD placement.
Planning an insertion with CBCT technology allows an accurate assessment of the spatial relationship of roots and the bone surface, which should result in a more precise insertion and a reduced probability of implant-to-root contact. In order to interpret the interradicular measurements accurately, however, the question of minimal safety distance or the minimal distance between the implant and a neighboring structure must be determined. For an interradicular insertion, this is the distance between the implant and the periodontal ligament (PDL). The relationship between interradicular distance (IR) and safety distance (SD) is as follows:
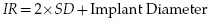
Here, recommendations in the literature once again are variable. Maino and associates (2003) suggest a 2.5–3.0 mm distance between the roots for the use of the Spider Screw implant, which amounts to a safety distance of 0.5–0.75 mm depending on the diameter. On the other end of the spectrum, Liou and colleagues (2004) recommend a safety distance of 2 mm between the implant and the PDL due to their observation that miniscrews may migrate under load. Therefore, the overall recommended interradicular distances according to published sources range from 2.5 to 5.5–6.0 mm depending on the implant diameter. Thus, an example that represents a realistic clinical scenario in the author’s practice is that a minimum interradicular distance of 3.6 mm should be present when using a 1.6 mm diameter implant resulting in a desired minimum safety distance of 1.0 mm.
If the interradicular distance is insufficient according to the CBCT-generated measurement, clinicians are advised to establish proper root divergence prior to inserting the miniscrew. This can be achieved through bracket repositioning or adding a root divergence bend to the archwire. Alternatively, a different site can be selected. One site that nearly always offers sufficient interradicular distance for palatal insertion is located between the maxillary second premolar and first molar (Poggio et al., 2006). This is because the maxillary first molar has only a single palatal root offering adequate interradicular distance for TAD insertions (Figure 18.2).
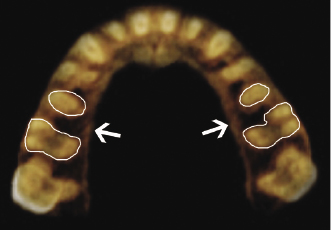
Even an ideal interradicular insertion site such as the one mentioned above leaves, at best, only about 2 mm on either side of the miniscrew. The room for error and imprecision in terms of identifying the precise spot to insert the pin and the most ideal angulation, therefore, is limited. A purchase point located only 1 mm too far distal combined with a few degrees of additional distal angulation surely will lead the implant to be placed too close to the distal limits, namely the mesial edge of the palatal first molar root or mesio-buccal root of first molar, depending on the implant length, of the insertion site. A proper protocol should be in place, therefore, to transfer the information obtained from the CBCT scan to the patient. Two approaches stand out and have been proven effective clinically.
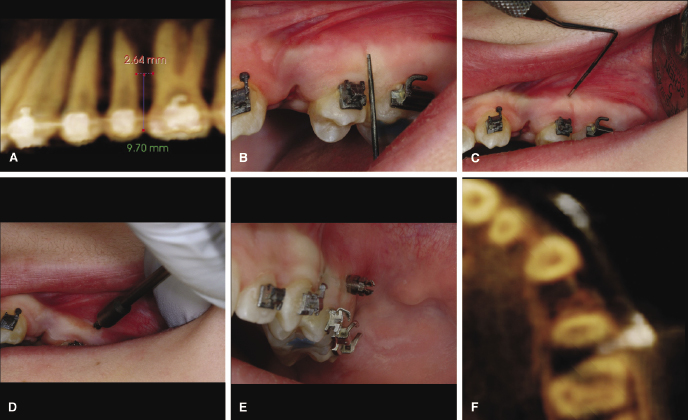
The first, which due to its simplicity, is this author’s preferred approach is based on the use of fixed intraoral landmarks that are identified easily on a CBCT scan. The most useful landmark seems to be the interproximal contact of two adjacent teeth and a bracket or the wire. Once the location of the greatest interradicular distance is identified, the perpendicular distance from there to the chosen landmark is measured (Figure 18.3A). This measurement then is transferred easily to the patient using a periodontal probe (Figure 18.3B). The insertion spot is marked with the probe (Figure 18.3C) and the implant is inserted at that site (Figure 18.3D). The dominant shortcoming of this method is the variability in insertion angle, which can be controlled only with proper insertion technique and a steady hand. Novices will have greater difficulty with this technique than experienced clinicians and may choose to diverge roots more aggressively with orthodontic means prior to insertion. For the experienced practitioner, however, this method predictably can lead to successful insertions (Figure 18.3E,F).
The second approach borrows from techniques applied in the dental implant field: the use of laboratory-fabricated surgical stents like the method above allows proper identification of the insertion location and also safeguards the direction of insertion, essentially guiding the implant in 3D. Various techniques for this approach have been described in the literature (Suzuki & Suzuki, 2008; Miyazawa et al., 2010). Most recently, Morea and coworkers (2011) detailed the use and outcome of a stereolithographic surgical guide fabricated from a CBCT scan (Figure 18.4). Using this group’s technique, the placement of the TADs averaged less than 1 mm displacement and less than 2° variation from its planned position. While this ap/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


