CHAPTER 18. Neoplastic and non-neoplastic diseases of salivary glands
OBSTRUCTION → Summaries pp. 172, 314
Salivary calculi
A stone can form in a salivary gland or duct. At least 80% of calculi form in the submandibular gland, about 6% in the parotid and about 2% in the sublingual and minor salivary glands.
Clinical features
Adults are mainly affected – males twice as often as females. Calculi are usually unilateral. The classical symptom is pain when the smell or taste of food stimulates salivary secretion. Alternatively, duct obstruction can lead to infection, pain and swelling of the gland.
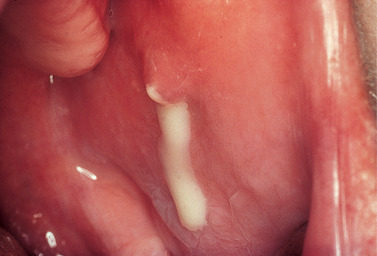
Occasionally there are no symptoms until the stone passes forward and can be palpated in the duct or seen at the duct orifice (Fig. 18.1). Alternatively, the stone may be seen in a radiograph. However, about 40% of parotid and 20% of submandibular stones are not radiopaque and sialography may be needed to locate them.
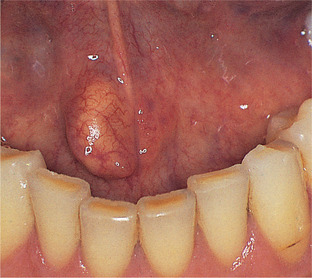 |
| Fig. 18.1
Salivary calculus. This stone has impacted just behind the orifice of the submandibular duct forming a hard nodule. The yellow colour of the stone is visible through the thin mucosa.
|
Calculi are not a cause of dry mouth.
Pathology
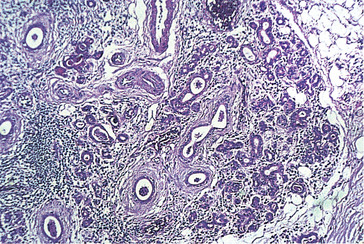
Salivary calculi usually form by deposition of calcium salts around a nidus of organic material and have a layered structure. The roughness of their surface may cause the duct lining to undergo squamous metaplasia (Fig. 18.2). An adherent layer of microbial flora often grows on stones and this, together with obstruction, usually triggers inflammation and fibrosis around the duct.
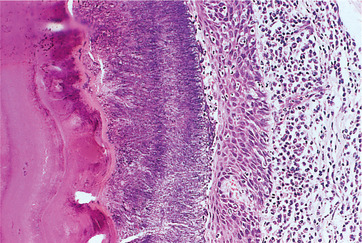 |
| Fig. 18.2
Salivary calculus in a duct. To the left is the salivary calculus which has a lamellar structure and an irregular surface. On the surface is a thick layer of microbial flora filling the space between the stone and the epithelial lining. In the surrounding wall, there is an infiltrate of lymphocytes and plasma cells and neutrophils are migrating through the duct epithelium into the lumen.
|
Management
The stone should be identified by plain radiography and the degree of damage to the gland from ascending infection and sialadenitis assessed by sialography.
If conservative measures fail and the stone is within the duct, the duct has to be opened. An incision, usually under local anaesthesia, is made along the line of the duct just long enough to release the mass. A temporary suture should be put around the duct behind the calculus to prevent it from slipping backwards. The papilla should be left unsutured or the margins of the opening are sutured to the mucosa on either side to prevent subsequent scarring and fibrous obstruction.
When stones are within the gland or a sialogram reveals that the gland is severely damaged by recurrent infection and fibrosis, it will probably have to be excised.
Key features of salivary calculi are summarised in Box 18.1.
Box 18.1
Salivary calculi: key features
• Adult males mainly affected
• Usually (80%) in submandibular gland
• Usually form by accretion of calcium salts round organic nidus
• Typically cause pain by obstructing food-related surge of salivary secretion
• Occasionally asymptomatic until palpable in the mouth or seen in routine radiograph
• Do not cause dry mouth
• Should be removed by manipulation or incision of duct
Parotid papilla and duct strictures → Summary p. 314
The usual cause of strictures at the papilla is chronic trauma (from such causes as projecting clasps, faulty restorations or sharp edges of broken teeth) leading to fibrosis. Fibrosis makes the duct papilla difficult to find and may prevent insertion of a probe.
Strictures of the duct are almost always caused by fibrosis resulting from ulceration and inflammation round a calculus or scarring following inadequate surgery.
Sialography should show the degree of narrowing of the duct or papilla and dilatation behind. Once the cause has been removed, treatment depends on the site of the obstruction. The papilla may have to be excised and the duct lining sutured to the oral mucosa on either side. Alternatively, the duct may be dilated with bougies.
Salivary fistula
Salivary fistula, a communication between the duct system or gland with the skin or mucous membrane, is uncommon. Internal fistulae drain into the oral cavity and cause no symptoms. By contrast, parotid fistula on the skin is troublesome and often persistent. It may be the result of an injury to the cheek or a complication of surgery. Infection often becomes superimposed and persistent leakage of saliva prevents healing. The treatment is primarily by surgical repair but is difficult, especially because of the risk of damage to branches to the facial nerve.
Mucoceles and cysts
The most common type of salivary and soft-tissue cyst is the extravasation mucocele of minor glands. It is not a true cyst as it has no epithelial lining. Retention cysts are far less common. Mucoceles mainly affect the minor salivary glands, particularly of the lip. The cause is usually damage to the duct of a mucous gland. This may be caused by a blow on the lip, as might happen to a football referee holding a whistle in his mouth.
Clinical features
Mucoceles most often form in the lower lip but, occasionally, on the buccal mucosa or floor of the mouth (ranula). They are usually superficial and rarely larger than 1 cm in diameter. In the early stages, they appear as rounded fleshy swellings. Later, they are obviously cystic, hemispherical, fluctuant and bluish due to the thin wall (Fig. 18.3). A mucocele cannot be distinguished from a retention cyst clinically, but this is of little practical importance. A similar mass in the upper lip is much more likely to be a salivary neoplasm.
 |
| Fig. 18.3
Mucous extravasation cyst. The typical presentation at the commonest site: a rounded bluish, translucent cyst in the lower lip.
|
Pathology
Preceding the formation of a mucocele, saliva leaking from a damaged duct into the superficial surrounding tissues excites an inflammatory reaction (Figs 18.4 and 18.5). The pools of saliva gradually coalesce to form a rounded collection of fluid, surrounded by compressed connective tissue without an epithelial lining.
 |
| Fig. 18.4
Extravasation mucocele. To the left is a cavity of spilt mucin with the remnants of the ruptured duct lining epithelium at its edge. To the right is the associated minor mucous salivary gland. A, saliva and macrophages; B, compressed connective tissue wall; C, minor salivary gland.
|
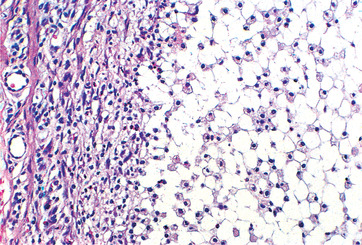 |
| Fig. 18.5
Extravasation mucocele. Higher power showing the lining of the mucin-filled space. Macrophages are migrating into the mucin and in phagocytosing it develop a foamy or vacuolated cytoplasm.
|
Less frequently, the duct may become obstructed but less severely damaged so that saliva does not escape into the surrounding tissues. A retention cyst thus forms with a lining of compressed duct epithelium (Fig. 18.6).
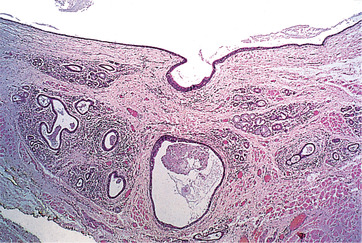 |
| Fig. 18.6
Mucous retention cyst. Remnants of the minor mucous salivary glands are visible, together with their dilated duct, the epithelium of which is continuous with the epithelial lining of the cyst (above).
|
Treatment
A small superficial mucocele should be excised with the underlying gland. The latter is usually found to have been removed with the cyst but if not, recurrence is likely.
Key features are summarised in Box 18.2.
Box 18.2
Mucoceles and cysts: key features
• Most common soft tissue cyst
• Most frequently on lower lip
• Usually caused by damage to duct and extravasation of saliva
• Saliva leaking into surrounding tissues causes mild inflammation
• Saliva eventually pools up to form a mucocele with connective tissue lining
• Rarely due to duct obstruction and dilatation forming a retention cyst with epithelial lining
Ranula
A ranula is an uncommon type of salivary cyst arising from the sublingual or submandibular salivary glands.
The structure is usually the same as other salivary retention cysts. Ranulae are usually unilateral and 2 or 3 cm in diameter (Fig. 18.7). Occasionally, they extend across the whole of the floor of the mouth. They are soft, fluctuant and bluish. They are typically painless but may interfere with speech or mastication. Treatment is preferably by marsupialisation with removal of the related gland. A simple incision leads to recurrence. Enucleation is difficult because of the very thin wall.
 |
| Fig. 18.7
Ranula. A large bluish, translucent swelling in the floor of the mouth caused by a mucous extravasation or retention cyst.
|
SIALADENITIS
Mumps → Summary p. 316
Mumps is due to a paramyxovirus (the mumps virus) and causes painful swelling of the parotids and sometimes other glands. It is highly infectious and is the most common cause of acute parotid swelling.
Clinical features
Children are mainly affected. An incubation period of about 21 days is followed by headache, malaise, fever and tense, painful and tender swelling of the parotids. Permanent nerve deafness or, rarely, meningitis are possible complications. Adults who contract mumps may develop orchitis or oophoritis and may have severe and prolonged malaise. After an attack immunity is long-lasting.
The diagnosis is usually obvious from the history and clinical findings, especially in a child. However, mumps may be mistaken for a dental infection or bacterial sialadenitis, if unilateral. Rarely, when the submaxillary or sublingual glands are affected, mumps may have to be differentiated from lymphadenitis. In cases of doubt, a history of mumps earlier in life usually excludes this diagnosis. If necessary, the diagnosis can be confirmed by a rise in titre of complement-fixing antibodies. Afterwards, antibodies to the S antigen disappear relatively quickly, and their presence indicates recent mumps. The V antibody is persistent and indicates infection at some time previously.
Mumps vaccination is provided as the measles-mumps-rubella (MMR) vaccination, introduced in 1988. Before this there were epidemics every three years. Recent patient concern about the MMR has reduced uptake to below the level required to prevent epidemics and there have been recent outbreaks, notably in 2005 among university students who had not been immunised. Immunisation is not completely effective in preventing the disease, but the acute episode is milder and, particularly in adults, may take atypical forms.
MMR vaccination is given at around 1 and 4 years of age. It is a live virus and a small minority of recipients develop a mild presentation of mumps with salivary gland swelling 3 weeks after the first dose.
Suppurative parotitis
Suppurative parotitis traditionally affected debilitated patients, particularly postoperatively, as a result of xerostomia secondary to dehydration. Currently, suppurative parotitis is more commonly seen in ambulant patients with severe xerostomia, particularly Sjögren’s syndrome, and as an uncommon complication of tricyclic antidepressant treatment. Important bacterial causes include Staphylococcus aureus, streptococci and anaerobes. Typical clinical features are pain in one or both parotids with swelling, redness and tenderness and often increasing malaise and fever. The regional lymph nodes are enlarged and tender, and pus exudes or can be expressed from the parotid duct (Fig. 18.8). The progress of the infection depends largely on the patient’s underlying physical state.
 |
| Fig. 18.8
Suppurative parotitis – pus is leaking from the parotid papilla.
|
Pathology
An intense acute inflammatory infiltrate extends along and dilates the ducts. Inflammation also extends into the periductal tissues and to a varying degree into acini. If neglected, abscesses form and there are varying degrees of acinar destruction.
Treatment
Treatment can be started with flucloxacillin, but only after pus has been obtained for culture and sensitivity testing. The antibiotic can be changed if the bacteriological findings dictate and drainage is rarely necessary.
Tuberculous sialadenitis
Mycobacterial parotitis is frequently a feature of advanced AIDS but, occasionally, also develops in immunocompetent adults. The chronic inflammatory swelling typically resembles a tumour and the diagnosis is only made after histological detection of non-caseating granulomas and identification of M. tuberculosis by PCR.
Chronic sialadenitis → Summary p. 314
Chronic sialadenitis is usually a complication of duct obstruction. It is usually unilateral and asymptomatic or with intermittent painful swelling of the gland. Sialography may show dilatation of ducts behind the obstruction.
Pathology
There are varying degrees of destruction of acini, duct dilatation and a scattered chronic inflammatory cellular infiltrate, predominantly lymphoplasmacytic (Fig. 18.9). Extensive interstitial fibrosis and, sometimes, squamous metaplasia in the duct epithelium follow. Calculus formation may be seen in the dilated ducts.
 |
| Fig. 18.9
Chronic sialadenitis resulting from obstruction. The ducts contain casts of mucin and neutrophils and are surrounded by a layer of fibrosis. There is severe acinar atrophy and the space previously occupied by acinar cells now contains infiltrates of lymphocytes and plasma cells.
|
If possible, the obstruction should be removed but, more often, the gland has to be excised and the mass examined histologically to exclude a neoplasm.
DRY MOUTH (XEROSTOMIA)
Many patients with severe xerostomia make no complaint of dry mouth, though they may, for instance, admit that they have difficulty in eating dry food. Some complain of an unpleasant taste in the mouth. Conversely, some who complain of dry mouth have normal salivary flow rates on objective testing and the problem is neurotic in nature. Salivary flow studies are valuable when patients complain of dry mouth. Important causes are summarised in Box 18.3. Patients may suffer xerostomia, calculi and ascending infection and the relationships between these conditions are shown in Fig. 18.10.
Box 18.3
Causes of xerostomia
Organic causes
• Sjögren’s syndrome
• Irradiation
• Mumps (transient)
• HIV infection
• HCV infection
• Sarcoidosis
• Amyloid
• Iron deposition (haemochromatosis, thalassaemia)
Functional causes
• Dehydration
• Fluid deprivation or loss
• Haemorrhage
• Persistent diarrhoea and/or vomiting
• Psychogenic
Anxiety states
Depression
• Drugs
Drugs
• Diuretic overdosage
• Drugs with antimuscarinic effects
Atropine, ipratropium, hyoscine and other analogues
Tricyclic and some other antidepressants
Antihistamines
Antiemetics (including antihistamines and phenothiazines)
Neuroleptics, particularly phenothiazines
• Some older antihypertensives (ganglion blockers and clonidine)
• Drugs with sympathomimetic actions
‘Cold cures’ containing ephedrine, etc.
Decongestants
Bronchodilators
Appetite supressants, particularly amphetamines
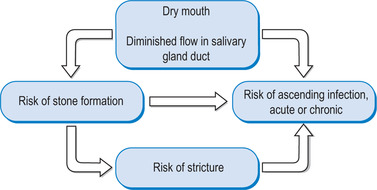 |
| Fig. 18.10
Interrelationships between dry mouth, calculi and their complications. Note: dry mouth may promote stone formation, but stones do not cause dry mouth.
|
SJÖGREN’S SYNDROME → Summary p. 316
In 1933, Sjögren noticed the association of dryness of the mouth and dryness of the eyes. Later, he found that there was a significant association with rheumatoid arthritis. These combinations of complaints are caused by two closely related but distinct diseases.
Primary Sjögren’s syndrome (sicca syndrome) comprises dry mouth and dry eyes not associated with any connective tissue disease. ‘Sicca syndrome’ is also sometimes used for organic causes of dry mouth that lack the immunological anomalies of Sjögren’s syndrome.
Secondary Sjögren’s syndrome comprises dry mouth and dry eyes associated with rheumatoid arthritis or other connective tissue disease.
Clinical features
Females are affected nearly 10 times as frequently as males. Sjögren’s syndrome affects 10–15% of patients with rheumatoid arthritis, possibly 30% of patients with lupus erythematosus and a variable proportion of patients with or without other connective tissue diseases. Sjögren’s syndromes are therefore relatively common. In the absence of drug treatment or radiotherapy, they are the main cause of dry mouth, but their most serious consequence is damage to the eyes and the risk of lymphoma. Primary Sjögren’s syndrome tends to cause more severe oral and ocular changes and has a higher risk of lymphomatous change than secondary.
Major oral effects of Sjögren’s syndrome are summarised in Box 18.4.
Box 18.4
Oral effects of Sjögren’s syndrome
• Discomfort
• Difficulties with eating or swallowing
• Disturbed taste sensation
• Disturbed quality of speech
• Predisposition to infection
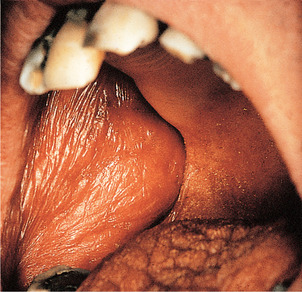
In the early stages, the mucosa may appear moist, but salivary flow measurement shows diminished secretion. In established cases, the oral mucosa is obviously dry, often red, shiny and parchment-like (Fig. 18.11). The tongue is typically red, the papillae characteristically atrophy and the dorsum becomes lobulated with a cobblestone appearance (Fig. 18.12). With diminished salivary secretion, the oral flora changes and candidal infections are common. The latter are the main cause of soreness of the mouth in Sjögren’s syndrome and cause generalised erythema of the mucosa, often with angular stomatitis. Plaque accumulates and there may be rapidly progressive dental caries (Fig. 18.13). The most severe infective complication is suppurative parotitis.
 |
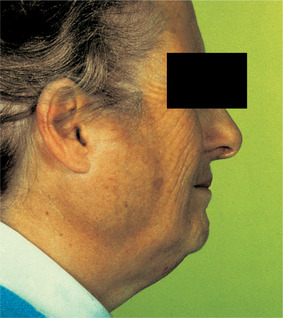
| Fig. 18.11
Sjögren’s syndrome. The mucosa is dry, red, atrophic and wrinkled and sticks to the fingers or mirror during examination. These changes are common to all causes of xerostomia.
|
 |
| Fig. 18.12
Tongue in Sjögren’s syndrome. Longstanding dry mouth and repeated candidal infection produce this depapillated but lobulated tongue.
|
 |
| Fig. 18.13
Sjögren’s syndrome. Extensive cervical caries is a frequent complication of dry mouth. In addition to the lack of saliva, patients may attempt to stimulate salivary flow with sweets or chewing gums.
|
Swelling of the parotids is not common, but a history of swelling at some stage may be obtained in about 30% of patients. Swelling due to the syndrome itself shows no inflammation and is rarely painful (Fig. 18.14). A hot, tender parotid swelling with red, shiny overlying skin indicates suppurative parotitis. Parotid swelling appearing years after the onset strongly suggests lymphomatous change (below).
 |
| Fig. 18.14
Salivary gland swelling in primary Sjögren’s syndrome. The outline of the parotid gland is clearly demarcated.
|
The association of dry mouth, which can destroy appetite, together with the pain of rheumatoid arthritis persisting over many years is a deeply distressing condition. Depression is a common consequence. These patients need support and reassurance as well as efforts to overcome the symptoms.
Sjögren’s syndrome can have serious ocular effects (Box 18.5).
Box 18.5
Ocular effects of Sjögren’s syndrome
• Failure of tear secretion
• Failure of clearance of foreign particles from the cornea and conjunctiva (keratoconjunctivitis sicca)
• Gritty sensation in the eyes and inflammation
• Risk of impairment or loss of sight
Aetiology and pathology
Sjögren’s syndrome is an autoimmune (connective tissue) disease which shows a corresponding variety of immunological abnormalities (Table 18.1). A retrovirus or other virus is as yet unconfirmed as a cause. The disease is systemic and affects all exocrine glands including those of the skin, vagina, lung and pancreas, though these rarely cause significant problems.
| Autoantibodies | Primary SS | Secondary SS |
|---|---|---|
| Salivary duct antibody | 10–36% | 67–70% |
| Rheumatoid factor | 50%± | 90%± |
| SS-A (Ro) antibodies | 5–10% | 50–80% |
| SS-B (La) antibodies | 50–75% | 2–5% |
| Rheumatoid arthritis precipitin | 5%± | 75%± |
Histological changes are shown in Box 18.6. Lymphocytes infiltrate the glands and cluster around ducts, replacing acinar cells (Fig. 18.15). The mechanisms of acinar cell destruction are unclear; they do not appear to be the target of direct lymphocyte killing. Over a period of years, the lymphocytic infiltrates enlarge and replace more of the gland. The ductal cells proliferate, possibly in response to cytokines released by the lymphocytes to form islands and sheets of cells around the ducts. Although myoepithelial cells are not a feature, the islands are often called myoepithelial islands (Fig. 18.16) and the overall appearance is sometimes called myoepithelial sialadenitis.
Box 18.6
Histological changes in salivary glands in Sjögren’s syndrome
• Polyclonal infiltration mainly by CD4 lymphocytes
• Infiltrate initially periductal
• Progressive spread of infiltrate through the glandular tissue
• Progressive destruction of secretory acini
• Proliferation of some duct tissue as epimyoepithelial islands
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


