Chapter 18 Minimal preparation (resin retained) bridges
What are minimal preparation (resin retained) bridges and when are they used?
Minimal preparation (resin retained) bridges are therefore used when the potential abutment teeth are unrestored or minimally restored and there is a need to reduce unnecessary tooth preparation. Consider the 22-year-old patient in Figure 18.1: preparation of the vital upper right central incisor tooth for a metal–ceramic retainer has been destructive of tooth tissue as this tooth only had a small fractured incisal edge. A cantilevered minimal preparation (resin retained) bridge using the central incisor as an abutment tooth would have been much more conservative. However, in this patient both lateral incisors are missing. Conventional bridge retainer preparation of the non-vital upper left central incisor tooth has been necessary not only to retain a pontic but also to disguise the appearance of the discoloured tooth. Furthermore, this patient had orthodontic treatment to close a midline diastema and since this treatment tends to be unstable, the conventional retainers were linked to also act as an orthodontic retainer.
History of resin-bonded bridges
Macromechanical retention
Natural tooth pontic
This technique can be used for a tooth that needs to be extracted. Once extracted, the root is resected and then the crown is cemented to the adjacent tooth/teeth using composite resin cement. At the resected root end the root canal should be opened and restored with either a glass ionomer or composite resin to prevent food and plaque stagnating within the tooth. To bond the extracted tooth the corresponding approximal surfaces are acid etched, bond applied and then composite used to cement the crown in place. Figure 18.2 illustrates diagrammatically how this procedure is carried out and Figure 18.3 shows an example where this has been done. In the author’s opinion this technique has been remarkably successful for the patient in Figure 18.3 as this ‘temporary’ measure had been carried out many years previously.
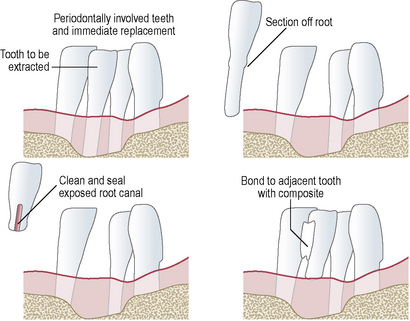
Figure 18.2 Diagrammatic representation of the patient seen in Figure 18.3. The teeth are periodontally involved and the lower right central incisor requires extraction. Following extraction the root is resected (top right), the root canal is cleaned from the resected end and the canal restored with composite resin or glass ionomer (bottom left). The tooth is then bonded to the adjacent tooth with composite resin cement (bottom right).
Laboratory-made bridges using macromechanical retention
Rochette bridges
A Rochette bridge consists of a pontic connected to a metal wing retainer which covers the lingual surface of the abutment tooth. Within the wing, countersunk holes are cut which allow retentive composite plugs or rivets to form when the bridge is cemented in situ (Figure 18.4). When Rochette bridges were originally described, they were designed to act as permanent fixed prosthodontic restorations (Figure 18.5). However, to achieve composite plugs of adequate strength they had to be of a significant diameter and depth, the latter necessitating a thick wing which caused problems in relation to the occlusion, especially when placed in the upper anterior region. In addition, occlusal stresses were concentrated on a limited number of composite plugs, predisposing to them to fracture and, as such, retention rates were often poor in the long term.
Micromechanical retention and solid wing retainers
Rochette bridges suffered from a number of problems, namely potential degradation of the exposed composite (wear) and areas of stress concentration within the countersunk holes and composite rivets. In an attempt to retain a solid wing with reduced thickness and provide an improved retention for minimal preparation (resin retained) bridges Thompson and Livaditis in 1982 described a method of electrolytically etching the fit surface of non-precious alloys. The acid, its concentration and etching time were different for different alloys. In each case, however, an etch pattern was produced that allowed micromechanical retention of the bridge when a chemically cured non-adhesive resin was used for cementation. This bridge became known as the ‘Maryland bridge’. The Maryland bridge technique required acid baths in the laboratory, and was a technique-sensitive procedure. Attempts were made to use chairside acid etch gels for the metal frame; however, the introduction of adhesive resin cements in the late 1980s superseded their further development.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses