Chapter 17 When and how to replace missing teeth
When to replace missing teeth?
Appearance
Tooth loss can have a devastating effect on a patient’s appearance, self-confidence and motivation. The loss of an upper central incisor is an obvious indication for prosthodontic replacement (Figure 17.1), but the technical challenges of designing the restoration must be taken together with the impact of the ‘smile line’. This assessment should be undertaken when the patient is talking and smiling in a relaxed environment and not from under forced conditions! For some patients the replacement of an upper premolar tooth may be unnecessary, but for those with a wide and high smile line tooth replacement may be justified. Whatever the clinical situation, it is advisable that tooth replacement based on appearance should be led by the patient and not the dentist.
Occlusal stability
When a tooth is missing the occlusion can change, with overeruption, tilting or drifting of opposing or adjacent teeth, causing a condition commonly referred to as an unstable occlusion. Consider the 25-year-old patient in Figure 17.2. The loss of the upper first and second premolar and lower first and second molar teeth has led to an unstable occlusion. The failure to replace these missing teeth led to overeruption of the lower second premolar and upper first and second molar teeth into the opposing edentulous spaces. This now complicates prosthodontic replacement as there is inadequate space between the teeth and opposing edentulous ridge.
The overeruption of teeth into edentulous spaces does not always occur and is impossible to predict. Therefore, if restoration of occlusal stability is the only clinical indication for tooth replacement following an extraction, it is advisable to monitor tooth movement over time. This tooth movement or dento-alveolar compensation can occur quickly in some patients and the tooth movement seen in the patient in Figure 17.2 occurred after 6 months. To avoid such a clinical situation, review appointments should be advised and a suggested timing would be after 3 months in the first instance. Baseline study models taken soon after the extraction may also be useful in confirming any tooth movement.
Function
Mastication
Patients frequently complain of difficulty in eating and trauma to the edentulous ridges following tooth loss. The latter problem can only be addressed with a prosthodontic replacement but the former is subjective and individual to each patient. There is little evidence to confirm that loss of molar teeth is accompanied by a significant loss of masticatory function. To the contrary, there is a large body of evidence to support the concept of the shortened dental arch (SDA) (Kanno & Carlsson, 2006). The posterior teeth are mainly involved in mastication and the SDA was proposed as a treatment option if molar teeth had been extracted. The minimum number of occluding pairs of teeth was the four premolar teeth or two pairs of occluding molar teeth. Today, the SDA is generally accepted as a premolar to premolar occlusion, following the loss of the molar teeth.
Does the SDA lead to increased wear of remaining teeth?
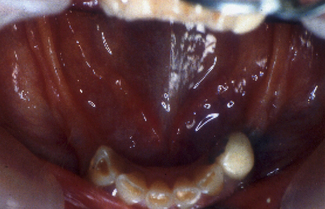
The patient in Figure 17.3 has lost all their posterior teeth and due to the severity of posterior alveolar ridge resorption is unable to wear a successful removable prosthesis. The lower anterior teeth are worn, with cupping of the incisal edges resulting from erosion, though attrition might be a contributing factor to the tooth wear. Whether the tooth wear would have reached the same severity if the posterior teeth were present is unknown.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses