CHAPTER 17. Oral cancer
EPIDEMIOLOGY
Oral carcinoma accounts for only about 2% of all malignant tumours in such countries as the UK and the USA. In most countries where reliable data are available, the incidence of cancer of the mouth, though variable, is low. India and Sri Lanka are, however, exceptional, and cancer of the mouth accounts for approximately 40% or more of all cancer there, though the incidence varies widely in different parts of this subcontinent.
Approximately 2000 cases of intraoral and lip carcinoma are registered each year in the UK. For the last 50 years the incidence of oral cancer has declined but, though it is rare, cases are now more frequently seen in those aged 30–50.
Age and gender incidence
Oral cancer is an age-related disease and 98% of patients are over the age of 40. While the overall incidence in the population is only about 1 in 20 000, this rises to 1 in 1100 in males of 75 and over. There is a sharp and virtually linear rise in mouth cancer with age, as with carcinoma in many other sites.
Cancer of the mouth is considerably more common in men than women in most countries, and carcinoma of the lip is at least eight times as common in men as in women in Britain. Intraoral cancer used to be several times more frequent in men than women, but the male to female ratio is overall about 3:2 and, in south-east England, recent figures show little difference in incidence between the genders. The change is the result of the progressive decline in oral cancer in men, but a low, static rate in women.
The incidence of oral cancer rises steeply with age and, with an ageing population, oral cancer will become more common.
AETIOLOGY
It has not been possible to prove conclusively a causative association between specific aetiological factors and oral cancer. This is partly because the quality of cancer statistics is very variable and partly because the aetiology of malignancy is complex and multifactorial. Causative factors operate over a long period and the process of malignant change is so slow that there is a prolonged lag period before it becomes evident. This has been shown strikingly in Japan, where cancers were still developing half a century after the radiation exposure from atomic bombs.
Significant or speculative risk factors for oral squamous cell carcinoma are summarised in Box 17.1.
Box 17.1
Possible aetiological factors for oral cancer
• Possible carcinogens
Tobacco
Alcohol
Betel quid habit
• Sunlight (lip only)
• Infections
Syphilis
Candidosis
Viruses
• Mucosal diseases
Oral epithelial dysplasia
Lichen planus
Oral submucous fibrosis
• Genetic disorders (rare)
Dyskeratosis congenita
Fanconi’s anaemia
Tobacco use
The earliest recorded tobacco-related death was in 1621 when a Thomas Herriot, who introduced clay pipe smoking to England, died (appropriately) of lip cancer. It was not thought at the time that pipe smoking had anything to do with Herriot’s death.
The effects of tobacco on the mouth depend on the way it is used and this varies in different countries. In Westernised countries, cigarette smoking predominates and pipe smoking has declined. In some countries, notably in India, the southern states of the USA and Sweden, tobacco chewing or snuffdipping (unsmoked tobacco held in the mouth for prolonged periods) is a habit. Methods of processing tobacco before use also vary widely, so that its products released into the mouth differ considerably in their effect.
Cigarette smoking
Smoking is considered to be a major aetiological factor, particularly in association with alcohol, and its importance is that it is preventable. However, it is difficult to demonstrate a direct causal link between cigarette smoking and oral cancer. In the UK, data have shown that oral cancer in males steadily declined over a period of more than three-quarters of a century while cigarette consumption grew steadily. Also, there is some evidence that the incidence of oral cancer in males may be rising again despite the fact that males are now smoking less.
Equally difficult to explain is the fact that mouth cancer in women has remained at a steady low level despite their widespread adoption of cigarette smoking. The escalation of their cigarette consumption is shown by the fact that the lung cancer rate in women has risen to nearly equal that of men in the USA.
Unlike pipe smoking or smokeless tobacco use, there is no specific oral lesion related to cigarette smoking, though heavy cigarette smokers develop patchy mucosal pigmentation.
Nevertheless, many studies have closely linked smoking, particularly in association with alcohol, to oral carcinoma. In case-control studies which take account of the amount and duration of tobacco consumption, the specific site and other factors such as alcohol, cigarette smoking has been shown to be closely associated and carry a significant relative risk. The risk of developing a second primary carcinoma is also closely linked to smoking and alcohol. Thus, smoking cigarettes infrequently appears to carry a very low risk, whereas the relative risk rises dramatically in heavy smokers.
Marijuana smoking is widespread and the smoke contains many of the carcinogens and co-carcinogens as tobacco smoke. It is suspected that it may be a more potent carcinogen than tobacco alone but this has not been confirmed in satisfactory studies.
Pipe smoking
Epidemiological evidence has associated oral cancer with pipe smoking, but the habit has steadily declined in most Westernised countries and has never become popular with women. Pipe smokers are also likely to develop stomatitis nicotina of the palate (Ch. 15), a white patch with no malignant potential.
Smokeless tobacco and betel quid
Smokeless tobacco habits are considered in Chapter 16. Betel quid usually contains tobacco and this habit is one of the most carcinogenic known. Areca nut without tobacco is also carcinogenic. For all smokeless tobacco habits, carcinomas tend to arise at the site in the mouth where the tobacco is habitually held and carcinomas are often preceeded by red or white lesions or dysplasia. However, carcinogens are also swallowed and the pharynx and oesophagus are also at risk.
The risk varies with the habit. In the southern USA, the habit of ‘snuff dipping’ causes extensive hyperkeratotic plaques and, after decades of continuous use, may lead to verrucous carcinoma (see below) as well as squamous carcinoma. However, this is a very slow process and cancers develop later in users than in nonusers. Scandinavian moist snuff appears to carry a very low risk.
Most smokeless tobacco users also smoke.
Alcohol
Alcohol consumption has steadily risen in Britain, particularly in the past half-century when oral cancer was declining. However, as noted above, the incidence may now be rising. In some countries, such as Denmark, there is good epidemiological evidence to link alcohol intake with oral carcinoma and, in the Bas Rhin area of France, alcohol is held to be responsible for the highest oral and pharyngeal cancer incidence in Europe. The low incidence of mouth cancer among Mormons and Seventh Day Adventists, who neither drink nor smoke, supports this idea.
It is generally considered that the combination of smoking and drinking is the most important aetiological factor for mouth cancer and, as noted above, many oral cancer patients smoke and drink heavily. The relative risks for alcohol and tobacco consumption are shown in Figure 17.1.
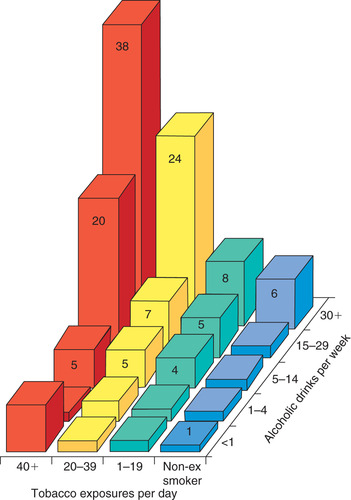 |
| Fig. 17.1
Relative risks of developing oral cancer in consumers (males in a Western population) of tobacco and alcohol. The relative risk for a non-smoker and non-alcohol consumer is taken as one. A smoker consuming 30 cigarettes a day and 20 alcoholic drinks a week is seven times more likely to develop carcinoma.
|
Alcoholic drinks are not usually allowed to reside in the mouth for long periods and there is no specific alcohol-related oral lesion. The mechanism by which alcoholic drinks might cause carcinomas is unclear and may not be their ethanol content. Drinks with the highest content of congeners, such as raw home-brewed spirits, appear to have the closest association with carcinoma. By contrast, evidence from the USA suggests that beer-drinking is associated with a greater risk. It is also possible that alcohol might predispose to carcinoma through its action on the liver and some studies have found a correlation between mouth cancer and cirrhosis. As with smoking, the total consumption is probably a critical factor.
Concern over the possible carcinogenic effects of alcohol has led to a proposal that it should be banned from mouthwashes, some of which contain more than 25% alcohol. There is as yet no conclusive link between mouthwash use and oral carcinoma.
Infections and immunological factors
The oncogenic potential of viruses is well recognised and some evidence has been produced to suggest that the human papillomavirus (particularly HPV 16) genomes can be found to be incorporated into mouth cancer cells. The importance of this finding remains unclear, especially as HPV is equally frequently found in normal mucosa. Screening exfoliated mucosal cells for the presence of HPV DNA has not proved to be useful as a screening test. If HPV played a significant role in oral carcinogenesis, it would be expected that the immunosuppressed, who suffer enhanced HPV infection, would be at greater risk of oral carcinoma. However, though uterine cervical and anal cancer in patients with AIDS is HPV-associated, oral carcinoma is uncommon and usually associated with other risk factors such as heavy tobacco or alcohol use. There is also no evidence of any greater susceptibility to intraoral cancer among patients who are deeply immunosuppressed therapeutically, though many are HPV carriers. Such patients have high rates of lip cancer, but only if exposed to strong sunshine.
There is better evidence that HPV plays a role in tonsil and oropharyngeal carcinoma. At these sites, up to 10% of carcinomas can be shown to contain HPV DNA integrated into the genome, but its precise contribution remains unclear and the focus of considerable research interest.
Syphilis
Syphilitic leukoplakia held pride of place as an infectious precancerous disease, in that the suggested rate of malignant change was between 30 and 100%. However, tertiary syphilis has become so rare that investigation of possible mechanisms has now become impossible and, even in developing countries, syphilitic leukoplakia is no longer a significant risk factor (Ch. 16).
Chronic candidosis
Chronic candidosis can lead to formation of hyperkeratotic plaques or speckled leukoplakias with epithelial dysplasia. There have been isolated reports of malignant change in such lesions but, overall, this accounts for a very small proportion of cases (Ch. 16)
Malnutrition
There is a high incidence of mouth as well as oesophageal cancer in Paterson–Kelly syndrome, in which iron deficiency is a feature. However, this disease is no longer a significant risk factor.
Epidemiologically, a low vitamin A intake has been associated with oral carcinoma, but deficiency of beta-carotene has now been dismissed as contributing to cancer. In India, malnutrition is widespread and may contribute, together with betel quid chewing, to the high incidence. However, there appears to be no comparably high frequency of mouth cancer in other areas, such as many parts of Africa, where malnutrition is at least as severe.
Oral sepsis
Oral sepsis has traditionally been regarded as contributing to mouth cancer. The latter is most common in low socioeconomic groups, which tend to have the most neglected mouths. Oral cancer also progressively declined in frequency in Britain, where a slow but steady improvement in oral health is well documented.
Despite such considerations, the aetiological role of oral sepsis in mouth cancer remains unproven.
Sunlight
Exposure to the ultraviolet component of sunlight is a risk factor, with the result that lip cancer is predominantly a disease of outdoor workers, particularly farmers and fishermen. As with other skin cancers, fair-skinned persons are at most risk. There may be multiple lesions in the most severely affected.
The relationship between exposure to sunlight and lip cancer has been clearly shown in hot countries such as Australia and the USA with large immigrant, fair-skinned populations of European origin. In the USA, for example, the risk of lip cancer approximately doubles for every 250 miles nearer the equator to the site of residence.
Dysplastic lesions caused by sunlight may precede the carcinoma and sun-damaged lip may be identified clinically by its loss of elasticity and atrophic epithelium. Changes due to sunlight are preventable and dentists should encourage the need to wear a high-factor sun-block when exposed to strong sunlight.
Genetic factors
There are a few genetic disorders, notably dyskeratosis congenita (Ch. 16), of which oral cancer is a frequent feature, but such disorders are rare. Mice with a high susceptibility to oral cancer have also been bred. However, the genetics of oral cancer are highly complex and causative genes have not been identified in humans.
Precancerous lesions
Several premalignant lesions are recognised (Ch. 16). In general, the risk of malignant transformation in the more common white lesions is very low, but the risk from speckled leukoplakia and erythroplasia is high. However, it is not known what proportion of carcinomas arise in clinically recognisable premalignant lesion.
Key features of cancer of the mouth are summarised in Box 17.2.
Box 17.2
Cancer of the mouth: key features
• Account for approximately 2% of all cancers in the UK, but one of the most common cancers in the Indian subcontinent
• Males more frequently affected
• Most patients are over 40 and incidence rises rapidly with age
• Lower lip is the most common site and related to actinic damage
• Tongue, posterolaterally, is the most common site within the mouth
• Some arise in pre-existing white or red lesions
• Heavy tobacco smoking and alcohol consumption tend to be associated
• In the Indian subcontinent and South-east Asia, betel (areca nut) habit may be more important
EARLY SQUAMOUS CELL CARCINOMA → Summaries pp. 247, 278, 279
In their earliest stages, carcinomas appear as painless red, speckled or white patches and only a minority are ulcerated (Figs 17.3 and 17.4). As noted in Chapter 16, a high proportion of erythroplasias and speckled leukoplakias are already malignant on first biopsy. The similar appearances of early carcinoma and premalignant lesions result from the processes of keratinisation and epithelial dysplasia and do not necessarily indicate that the carcinoma has arisen in a pre-existing lesion.
 |
| Fig. 17.3
Squamous carcinoma of the soft palate and mucosa posterior to the tuberosity appearing as a speckled leukoplakia.
|
As a carcinoma enlarges, it may develop into a raised nodule or become ulcerated. Induration results from inflammation and fibrosis and infiltration of the tissues. By the time a carcinoma has formed an indurated ulcer with the typical rolled border, it will have been present for some time (Fig. 17.5). As noted below, diagnosis at this late stage is associated with a very poor prognosis and every attempt must be made to identify carcinomas as early as possible.
 |
| Fig. 17.5
Advanced squamous carcinoma. The classical ulcer with a rolled border and central necrosis is a late presentation. Note the surrounding areas of keratosis and erythema which had been present for many years before the carcinoma developed.
|
Ulceration may be associated with soreness, or stinging pain when sharply flavoured food is eaten. Pain is of no value in the diagnosis of carcinoma, but is typically severe in the late stages. Bleeding, either spontaneously or to mild trauma, is also a late feature.
ORAL CANCER SITES
The lower lip is the most frequent site of oral cancer overall, while the tongue is the most frequently affected site within the mouth. In the oral cavity, the majority of cancers are concentrated in the lower part of the mouth, particularly the lateral borders of the tongue, the adjacent floor of the mouth and lingual aspect of the alveolar margin, forming a U-shaped area extending back towards the oropharynx (Fig. 17.2). This accounts for only about 20% of the whole area of the interior of the oral cavity, but 70% of oral cancers are concentrated there. This distribution may be due to the likelihood that carcinogens could pool and concentrate in the lower mouth before swallowing. Possibly for the same reason, the hard palate and central dorsum of tongue are very rarely affected.
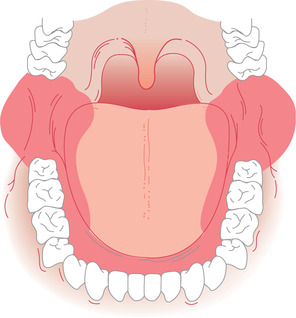 |
| Fig. 17.2
High-risk sites for development of oral carcinoma. The shaded U-shaped area accounts for only about 20% of the whole area of the interior of the mouth, but is the site of over 70% of oral cancers.
|
 |
| Fig. 17.4. |
| Early squamous carcinoma. Despite its inconspicuous appearance, this small white patch on the lateral border of the tongue was found to be a squamous carcinoma on biopsy. |
Carcinoma of the lip
The lip is the most common single site for oral cancer but infrequently seen in dental practice. Being visible, it is often recognised at a very early stage and so has a better prognosis than intraoral cancer. The usual site is the vermilion border of the lower lip to one side of the midline. Men of middle age or over are predominantly affected.
An area of thickening, induration, crusting or shallow ulceration of the lip, less than a centimetre in diameter, is a common early presentation (Fig. 17.6). Advanced, neglected tumours (Fig. 17.7) are unlikely to be seen now. Spread to lymph nodes tends to be slow. The submental nodes are usually the first to be affected.
 |
| Fig. 17.6
Squamous carcinoma of lip. There is an indurated, crusted ulcer with keratosis at one margin in the centre of the lower lip.
|
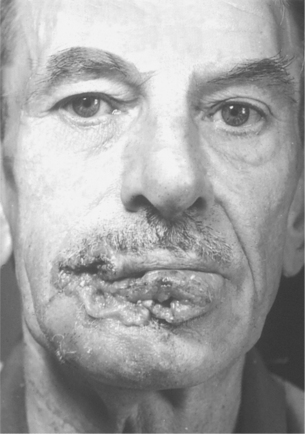 |
| Fig. 17.7
Advanced carcinoma of lip. There is extensive ulceration and necrosis and distortion. Nowadays such extensive lesions are unusual.
(Taken before the advent of colour photography.)
|
Carcinoma of the tongue and floor of mouth
The anterior part of the tongue, particularly the lateral border, and the adjacent ventral tongue and floor of mouth are frequently involved. Presentation is often late with an ulcer 2 cm or more in diameter. Approximately 60% or more patients with localised lesions less than 2 cm in diameter survive for 5 or more years after treatment. In more advanced disease, the usual picture is of a typical malignant ulcer several centimetres in diameter, hard in consistency, with rolled or irregular, raised edges and a rough infected floor which bleeds readily. As growth proceeds, the carcinoma becomes fixed to surrounding tissues and infiltrates the tongue, which becomes progressively stiffer and more painful. Eating, swallowing and talking become d/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


