New Treatment Modalities for Class III Malocclusion
Nazan Küçükkeleş, Hanife Nuray Yılmaz, Şirin Nevzatoğlu
Patients with Class III malocclusion comprise a relatively small percentage of the average orthodontic practice but these cases are among the most difficult to treat effectively and efficiently.1 Until the 1970s, skeletal Class III malocclusions were thought to be caused solely by a large and/or protrusive mandible. Now we know that they can be a result of various factors: (1) prognathic mandible with a normally positioned maxilla, (2) retrognathic maxilla with a normal mandible, (3) combination maxillary retrognathism and mandibular prognathism, and (4) normal skeletal relationship of maxilla and mandible with reverse overjet in the presence of centric relation–centric occlusion (CR-CO) discrepancy, also known as a “pseudo” Class III relationship.
According to studies by Ellis and McNamara2 and Guyer et al.,3 40% to 60% of skeletal Class III patients have maxillary deficiency or retrusion, suggesting that maxillary deficiency does play a role in most skeletal Class III malocclusions. Therefore the appropriate treatment option for growing patients with Class III malocclusions should include maxillary protraction. For more than 40 years, protraction facemask therapy has been the most popular method of protracting the maxilla and the effects are well documented. This chapter discusses the effects of protraction facemask therapy as well as the timing of its application for maximum efficiency.
Timing of Treatment for Class III Malocclusion
The timing of treatment for Class III malocclusion has always been a matter of debate among orthodontists. Should treatment start early in the patient’s childhood or should clinicians wait until growth is completed and then proceed with orthognathic surgery? Some authors support the benefits of early treatment and point to the disadvantages of a long treatment time while waiting for the skeletal maturation of a child before sending him or her for orthognathic surgery. Others choose early orthognathic surgery because of concerns about dental compensation and/or mistiming of the cessation of mandibular growth during orthopedic treatment.
Proffit4 contended that treatment should start as soon as possible after Class III malocclusion is diagnosed. He pointed to an ideal age of 8 years. Baccetti et al.5 studied a sample of 46 subjects in mixed dentition and compared them with a control sample of 32 subjects with untreated Class III malocclusion. Treated and untreated samples were divided into early and late mixed dentition groups for identification of the optimum treatment timing. The younger group showed significantly greater advancement of maxillary structures and significantly more upward and forward direction of condylar growth after treatment.
Kapust et al.6 examined patients divided into three different age groups and suggested that earlier treatment produces a more favorable result; however, the older children did have significant treatment outcomes, indicating that orthopedic changes can be obtained in the 10- to 14-year-old age group as well.
In 2000 Saadia and Torres7 examined the sagittal response of Class III patients in the primary, mixed, and late mixed dentition phases who were treated with expansion followed by facemask therapy. They found that greater significant changes were seen in patients treated in the primary and mixed dentition phases, even with fewer hours of appliance wear per day.
In 2004 Ochoa and Nanda8 examined the growth pattern of maxilla and mandible with ages ranging from 6 to 20 years and reported that maximum maxillary growth was observed between the ages of 6 and 8 years. The maxillary complex was still growing after the age of 8 years but at a decreasing pace until the age of 14 years. Moreover, in girls there was a significant decrease in maxillary growth after the age of 12 years while in some male patients even little maxillary growth was seen until the age of 20 years.
In the same year, Franchi et al.9 treated 50 patients who were in late deciduous/early mixed or late mixed dentition with an initial phase of rapid palatal expansion (RPE) and facemask therapy followed by a second phase of preadjusted edgewise therapy. They reported that orthopedic treatment of Class III malocclusion was more effective when it was initiated at an early developmental phase rather than at later stages with respect to untreated Class III control groups. However, patients treated with RPE and facemask therapy in the late mixed dentition did exhibit improvement with the treatment but to a lesser degree.
Baik10 examined 47 Korean children who were divided into three groups according to their ages and found no statistically significant difference among the groups.
Sung and Baik11 subsequently evaluated the effect of maxillary protraction in patients who were divided into six age groups from ages 7 to 12 years and found that the amount of skeletal change among the groups was not statistically significant.
Merwin et al.12 examined 30 patients who were divided into two age groups of 5 to 8 years and 9 to 12 years and reported that cephalometric changes were similar between the two groups, suggesting that a similar skeletal response can be expected in patients in either the early or the late mixed dentition.
Looking at all of these results, it seems favorable to apply maxillary protraction before the age of 12 years. Nevertheless, the treatment results are more effective when maxillary protraction is initiated at an early developmental phase of the dentition rather than at later stages.
Treatment Approaches in Class III Malocclusion
There are three main approaches for the treatment of a skeletal Class III malocclusion:
Because this chapter is concerned with the new orthopedic treatment modalities, the first and third treatment options will not be discussed and we will focus on the treatment option of growth modification.
Effects of Facemask Therapy
Since most skeletal Class III patients have maxillary deficiency or retrusion, the appropriate treatment option for growing patients is protraction of the maxilla. The literature reports a series of approaches regarding orthopedic treatment of Class III malocclusions.13 Facemask treatment is the most frequently used treatment protocol for this anomaly. The treatment effects of facemask therapy are a combination of skeletal and dental changes of the maxilla and the mandible.9 The maxilla moves downward and forward with a slight upward movement in the anterior and downward movement in the posterior palatal plane as a result of protraction force together with the extrusion of posterior teeth. Consequently, downward and backward rotation of the mandible improves the maxillomandibular skeletal relationship in the sagittal dimension. This rotation is a major contributing factor in establishing positive overjet. Currently there seems to be general agreement on applying a downward and forward force with 30 degrees to occlusal plane in order to achieve anterior displacement of maxilla with minimal downward and forward rotation.14–16 There are also some dentoalveolar changes, such as increase in upper incisor inclinations due to mesial movement of upper dental arch and decrease in lower incisor inclinations due to the pressure applied by the chin cup of the facemask.
In clinical studies the duration of facemask use ranges from 12 to 24 hours per day with a force amount of 300 to 600 g per side, with most studies showing an average of 2 mm maxillary advancement.5,9,17–21
In a prospective clinical trial,22 after facemask treatment in 20 patients, overjet correction was found to be the result of forward maxillary movement (31%), backward movement of the mandible (21%), labial movement of the maxillary incisors (28%), and lingual movement of the mandibular incisors (20%).
In 2003 Cha23 evaluated skeletal and dentoalveolar changes produced by RPE and facemask therapy in 85 subjects who were divided into three groups: prepubertal growth group (Group 1; n = 34), pubertal growth group (Group 2; n = 32), and postpubertal growth group (Group 3; n = 19). The Delaire type facemask was used for 12 hours with 500 g of force. Negative overjet was corrected by 80.1% skeletal and 19.9% dentoalveolar changes in Group 1, 84.0% skeletal and 16.0% dentoalveolar changes in Group 2, and 63.6% skeletal and 36.4% dentoalveolar changes in Group 3. The maxillary anterior movement in Groups 1, 2, and 3 was 2.69, 2.69, and 0.97 mm, respectively.
Challenges of Using Facemask Therapy
Although the main target of the treatment is forward movement of the maxilla, the values for maxillary advancement reported in the literature5,9,17–19 are not more than 2-mm with 6 to 12 months of treatment. Also, there are some limitations of this method, such as insufficient skeletal correction in severe Class III malocclusions and undesired dentoalveolar effects due to application of high forces to the teeth.
In 2003 Hägg et al.24 reported that 7 of 21 patients who were treated by facemask had negative overjet after an average of 8 years recall. Of these patients, 29% were considered for orthognathic surgery. Baccetti et al.25 reported that 12 of 41 patients (28%), all of whom had comprehensive orthodontics after facemask therapy, had negative overjet and Class III molar relationships after an average of 6.5 years recall at a mean age of 15 years. In 2006 Wells et al.26 examined 41 Class III patients 10 years after the treatment of facemask therapy and reported 30% relapse into reverse overjet, mainly because of increased horizontally directed and often late mandibular growth. Due to the unpredictable long-term relapse potential, it was recommended by the authors to overcorrect the overjet in anticipation of some relapse. Furthermore, using various types of retention appliances was also proposed to improve stability.26 Since dentoalveolar changes are the most prone to relapse, it would be advantageous to eliminate or at least minimize dentoalveolar effects and maximize orthopedic effects of the treatment.24–26
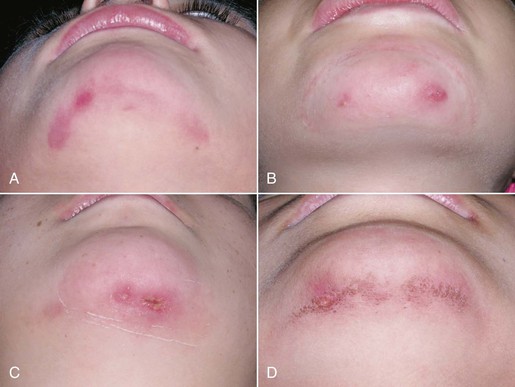
Another problem encountered with extraoral appliances is the need for patient compliance and parental support.27 These appliances are bulky yet need to be worn for at least 12 to 16 hours per day for a total duration of 9 to 12 months. Also, high forces usually cause irritation of the skin in the chin area (Fig. 17-1). All of these factors lead to compliance problems and impair the treatment results. In 2006 Brandao et al.28 examined the duration of extraoral appliance use using an electronic recording device. Interestingly, they found that the electronic recording device reported 6 to 7 hours of use whereas the patient reported 13 to 14 hours of use of the extraoral device.
Perceptions of Facial Esthetics and Psychological Development
The perception of facial esthetics influences one’s psychological development from early childhood to adulthood. In the literature it has been reported that laypersons evaluate prognathic profiles more negatively than retrognathic profiles.29–31 Therefore early intervention in cases of orthodontic malocclusion is important from the standpoint of the patient’s psychological development. Some clinicians prefer orthognathic surgery for the correction of Class III malocclusion and wait until age 20 years because of the potential relapse seen with late mandibular growth. However, delaying the treatment time results in patients coping with all of the problems mentioned above during adolescence. At the end of this challenging stage patients will then have orthognatic surgery under general anesthesia in addition to an extensive period of orthodontic treatment.
Problems Related to Surgery
Sometimes surgery requires blood transfusion and bone grafts at the time of operation, which make the surgery even more difficult. It was reported that 51% of maxillary advancement and extrusion surgery requires bone grafts. Sixty-five percent of bone grafts are taken from the iliac bone whereas 8.5% are taken from the rib area.32 During or after maxillary osteotomy the complication rate is reported to be approximately 4.2%. In addition, damage to the roots of teeth due to the internal rigid fixation screws, hemorrhage, morbidity, and hearing and vision loss are reported as other complications of orthognathic surgery.
Regarding the stability of the maxillary advancement surgery, relapse of less than 2-mm is found in 80% of cases and relapse of 2- to 4-mm is reported in the remaining 20% of cases. However, the relapse rate increases when maxillary advancement and extrusion are both performed. Although the maxillary advancement is found to be stable, 40% to 50% of extrusion is prone to relapse, indicating the instability of this intervention. Stable results are obtained when the rigid internal fixation is used in maxillary advancement plus mandibular setback surgery. However, 40% to 50% of relapse is also seen when the mandibular setback surgery is performed alone.33–36
Improved Treatment Modalities for Class III Malocclusions
Based on the information discussed above, new treatment protocols that are effective, efficient, and applicable at any age are needed for the treatment of Class III malocclusions. A new focus is the use of skeletal anchorage devices to achieve protraction of the maxillary complex, with some using these devices in conjunction with corticotomies. In 1999 Rachmiel et al.37 presented 14 cleft lip and palate patients (8 to 10 years old) treated by an incomplete Le Fort I osteotomy followed by protraction of the maxilla with facemask. The results showed a mean maxillary forward movement of 7.2-mm after 3 weeks of protraction, which was followed by a retention period of 9 weeks for callus maturation. In 2001 Molina38 also applied a facemask in conjunction with incomplete Le Fort I osteotomy in 43 patients who were divided into two groups according to the severity of the maxillary retrusion. He reported a mean maxillary forward movement of 9-mm in the severe group and of 5-mm in the moderately retrusive group. Unfortunately, neither study reported long-term results of the corticotomy-assisted maxillary protraction protocol. In the similar time period, Singer et al.39 achieved 4-mm of advancement with the facemask applied from Brånemark implants on the zygomatic buttress region. It was the first report in which temporary anchorage devices (TADs) were used for the orthopedic protraction of maxilla in growing patients. Currently, in the field of orthodontics, a dramatic increase in the use of TADs, such as palatal implants, onplants, mini-screws, and mini-plates, has been observed. Currently, mini-plates are commonly used in maxillofacial surgery for rigid fixation of the bony segments. Most of the literature reports that the mini-plates are quite stable, even with the high forces.40 In 2008 Kircelli and Pektas41 applied the Delaire type facemask from mini-plates, which were placed on the lateral nasal walls of the maxilla. The elastic force was 300 g per side and they reported 4.8-mm maxillary advancement together with 3.3-mm forward movement of the infraorbital region in six patients. In 2010 Heymann et al.42 applied Class III elastics between mini-plates on the zygomatic region in the maxilla and the canine region in the mandible. They reported that forward movement of the maxilla ranged from 0.4- to 4.7-mm in 12 months for six patients with a mean age of 11.8 years. In the same year, De Clerck et al.43 reported on a group of 21 patients (mean age of 11.10 years) consecutively treated with the same protocol. The results were compared with a matched control group of 18 untreated Class III patients and revealed that A point showed an average of 4-mm forward movement in the treated subjects compared to the control subjects. Orbital and pterygomaxillary points advanced almost 3-mm and 2-mm, respectively, with more advancement in the treated group. A significant restraining effect on mandibular growth (–2-mm) was also recorded in the treated group.
Orthopedic Effects of Rapid Palatal Expansion versus Corticotomy-Assisted Maxillary Protraction (Study I)
In 2007 our team44 designed a study to compare corticotomy-assisted maxillary protraction with conventional rapid palatal expansion (RPE)–assisted facemask therapy. Subjects with comparatively mild maxillary retrognathism were treated by conventional RPE plus facemask. This group included 18 patients with a mean age of 12.9 ± 1.1 years. Another 16 patients with a mean age of 13.1 ± 2.1 years who had moderate to severe maxillary retrognathism were treated by surgery plus facemask. In the latter group, Le Fort I osteotomy was performed for each patient under general anesthesia by the same surgeon and facemask was applied on the fifth to seventh day postsurgery with a total force value ranging from 1700 to 2000 g (Figs. 17-2 to 17-4). The elastics were oriented with a 30-degree angle to the occlusal plane as in the other study group. Facemasks were worn 24 hours per day (except during meals) until the achievement of Class II dental relationships, after which patients were told to switch to nighttime wear for another 3 months for retention purposes. In both groups maxillary splints were debonded following retention periods.
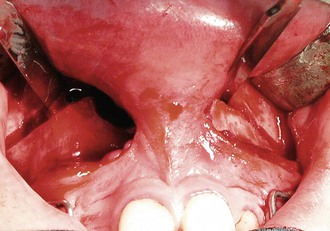
Figure 17-3 Study I. Corticotomy line.
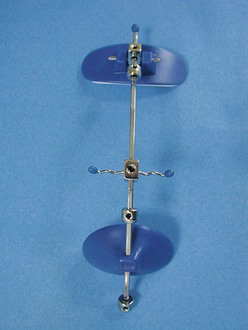
Figure 17-4 Petit type facemask appliance.
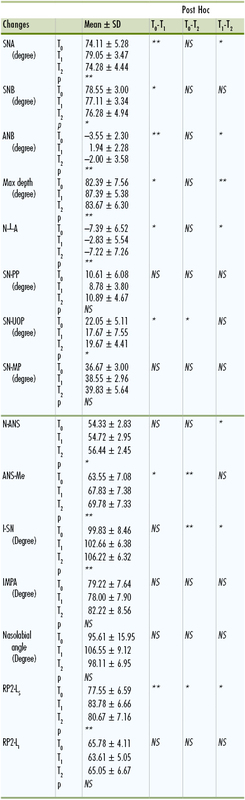
After the protraction phase, sella-nasion A point (SNA) and A point nasion B point (ANB) angles increased and sella-nasion B point (SNB) angle decreased significantly in both groups and sagittal maxillomandibular relationships were normalized (Table 17-1). The cephalometric findings demonstrated significant maxillary advancement in both groups together with mandibular backward rotation. However, there was a significant difference between treatment groups from the point of maxillary advancement reflected on hard and soft tissues (4-mm advancement in the surgery group versus 1.3-mm in the RPE group). Soft tissue results revealed that the upper lip and upper lip sulcus moved significantly forward in both groups during treatment but the values were significantly higher in the surgery group. Treatment duration was also found to be significantly different between groups. Total treatment time was 5 months for the corticotomy group and 9 months for the RPE plus facemask group. Therefore the surgically assisted facemask treatment was found to be more efficient and effective for the correction of Class III malocclusion when compared to the RPE-assisted facemask treatment. A patient treated with corticotomy-assisted facemask therapy is presented in Case Report 1.
TABLE 17-1
Means and SD Values Before and After Treatment in Study I
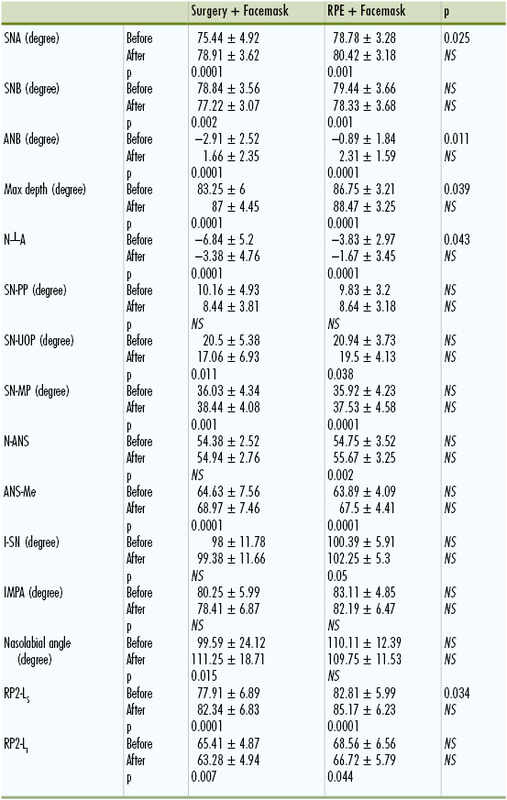
Student t test (statistical analysis used in this study).
ANB, A point nasion B point; ANS, anterior nasal spine; ANS-Me, Distance of ANS to Menton; I-SN, upper incisors sella-nasion; IMPA, incisor mandibular plane angle; MP, mandibular plane; N, nasion; N┴A, distance of A point to a line drawn from nasion perpendicular to Frankfort horizontal plane; NS, not significant; RP2-Li, distance of vertical reference plane to labrale inferior; RP2-Ls, distance of vertical reference plane to labrale superior; RPE, rapid palatal expansion; SN, sella-nasion; SN-PP, sella-nasion palatal plane; SN-UOP, sella-nasion upper occlusal plane; SNA, sella-nasion A point; SNB, sella-nasion B point.
Long-Term Evaluation of Corticotomy-Assisted Facemask Therapy (Study II)
We decided to evaluate the long-term stability of the surgery-assisted protraction group in 2012. Sixteen patients were recalled 5 years following the surgically assisted protraction. Only nine patients presented for the follow-up study and records were renewed. The study was carried out using lateral cephalometric films taken before treatment (T0), immediately after maxillary protraction (T1), and after 5 years (T2). Although the cases maintained normal overjet and overbite and the Class I relationship, significant relapse of maxillary advancement was noted in the follow-up period (Table 17-2). On the other hand, the statistically significant decrease of the SNB angle obtained during treatment remained unchanged after treatment. During maxillary protraction upper incisors moved bodily without proclination whereas in the follow-up period significant increase in the upper incisor inclination was observed, probably to compensate for the relapse of maxillary position. During treatment the upper molars moved forward and they maintained their position throughout the follow-up period. There were no significant changes in the lower incisor inclination at all stages. Skeletal and dental extrusion achieved during protraction was preserved. It was interesting that even though some soft tissue improvements were lost, forward movement of the maxilla and the upper lip was partially maintained. This led to a well-maintained facial appearance in the follow-up period. Clinical examination of the recall period showed well-preserved dental relationships. There were no discrepancies between the final and recall occlusions and the residual changes were still significant compared to the pre-treatment values.45
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses