Natural Teeth Adjacent to an Implant Site
Joining Implants to Teeth
Carl E. Misch
A common prosthetic axiom is to provide a partially edentulous patient with a fixed prosthesis whenever possible. Implant dentistry may often provide the additional abutments necessary to fulfill this goal regardless of the number of teeth missing. The ability to add abutments in specific locations, rather than being limited to a particular remaining natural abutment that may not always be in optimum health, enables the dentist to expand this prosthetic axiom to most partially edentulous patients.
The dentist most often uses implants as independent support for the restoration. On rare occasion, the implant may be splinted to the natural teeth in the same prosthesis. In either situation, the treatment plan is strongly influenced by the dental evaluation of the remaining natural abutments adjacent to the edentulous site.
Natural teeth may require additional therapy before the final prosthesis can be completed. It is best to communicate with the patient regarding all required treatment involved in the rehabilitation process before the surgical placement of the implants. Otherwise, treatment outcome, sequences, and cost may conflict with the originally projected result and lead to dissatisfaction, the need to modify the original treatment plan, or a poorer prognosis.
Whether considered for abutment support or not, teeth adjacent to a partially edentulous site are evaluated thoroughly and from a different perspective than the rest of the dentition.1,2 In the previous chapter, the conditions that warrant extraction of the tooth are presented. In this chapter, the tooth adjacent to the edentulous site is planned to be maintained. However, on occasion, the adjacent tooth exhibits bone loss next to the edentulous site and presents a less than optimal quality of health. As a consequence, the available bone characteristics immediately adjacent to the tooth are highly influenced by its presence. Often this is a determining factor in the choice between an independent implant prosthesis, a traditional fixed partial denture (FPD), or a removable restoration. When multiple teeth are missing, the treatment becomes even more complex with additional restorative options, such as whether implants and natural teeth may serve as abutments in the same prosthesis.
The dental criteria of the adjacent tooth to an edentulous space addressed in this chapter are (1) abutment options, (2) adjacent bone and soft tissue anatomy, (3) cantilevers, (4) implants connected to teeth, (4a) mobility (of teeth and implants, (4b) splinting natural abutments, (4c) natural and implant pier abutments, and (5) transitional abutments (Box 17-1).
Abutment Options
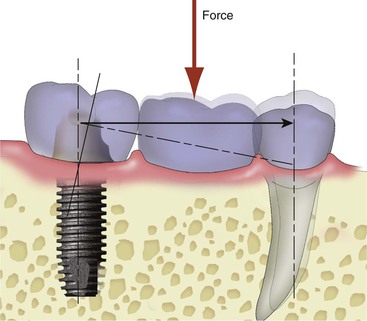
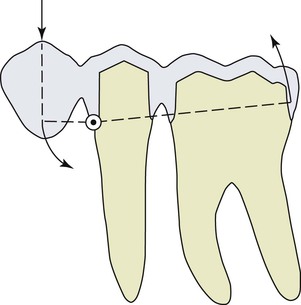
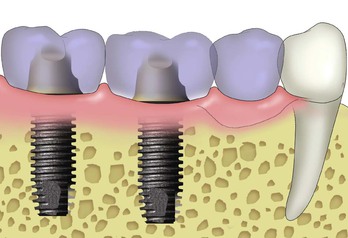
Several options are available for the adequate restoration of an edentulous segment. Before the 1990s, when implants were used in a partially edentulous patient, a three- or four-unit FPD was fabricated with an implant used as one terminal abutment along with a natural tooth separated by one or two pontics3,4(Figure 17-1). When the osseointegrated implant concept for completely edentulous fixed prostheses was introduced in the mid 1980s, the concept was modified for partially edentulous arches to make an implant prosthesis as an independent unit. The primary reason for this approach was to limit the cantilever effect of a “mobile” tooth joined to a “rigid” implant5,6 (Figure 17-2). However, the primary advantage of two separate prosthetic units is more related to reduced biologic complications of the tooth rather than biomechanical implications on the implant.
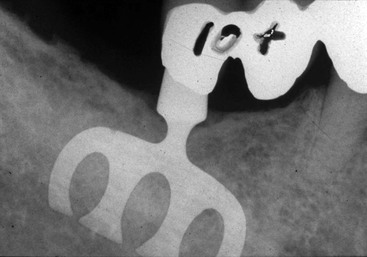
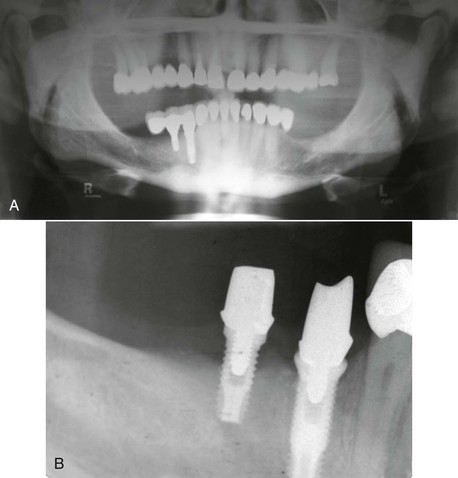
Under ideal conditions, placing implant abutments in sufficient number to fabricate a completely separate implant-supported prosthesis has several biologic advantages. The most common cause of failure of tooth-supported fixed prostheses is caries of the abutment teeth.7 Unrestored natural teeth do not decay as often as restored teeth, and implant abutments do not decay. In addition, the pontic between splinted abutments (whether natural teeth or a tooth and an implant) acts as a plaque trap. As a result, whereas a crown on a natural tooth has a decay rate of 1% at 10 to 15 years, an abutment for a FPD has a caries rate of more than 20% (Figure 17-3). The second most common cause of fixed prosthesis failure is endodontic failure or complications of a natural tooth abutment. Implant abutments do not need endodontic therapy. Unrestored natural teeth are less likely to require endodontics. Therefore, the natural tooth should not be splinted to an implant under ideal conditions. The 10-year survival rates indicate a greater than 25% improved survival rate for implant prosthesis compared with FPDs supported by natural teeth (or natural teeth splinted to implants) because the natural tooth is more prone to biologic complications.8,9
Compared with unrestored natural teeth, natural teeth abutments are more difficult to clean; collect and retain more plaque; are often more temperature or contact sensitive; and are more subject to future prosthetic, periodontal, or endodontic treatment. Caries, endodontic problems, or both may cause not only a loss of the fixed prosthesis but also almost as often lead to the failure and extraction of at least one of the natural tooth abutments. As a result, an independent implant restoration is the treatment of choice for almost every multiple-tooth edentulous site in a partially edentulous patient. In addition to the biologic advantage of independent implant prostheses, there is also a biomechanical advantage. Natural teeth respond to occlusal forces differently than implants. Whereas a light force produces most of the recorded movement of a tooth, the amplitude of implant movement is related directly to the force applied.6–8,10–11 In arches with implant and natural abutments, it is easier to adjust the occlusion when these entities are two independent units.
When planning an independent implant prosthesis, instead of using a natural tooth as one of the terminal abutments, the dentist usually requires the addition of at least one more implant. An increase in implant abutment number enhances the implant–bone interface and therefore reduces the stress to the support system and improves the ability of the fixed restoration to withstand additional forces when necessary. In addition, because of the additional retentive units, uncemented or unretained restorations occur with less frequency. Unretained restorations are the third most common complication reported in fixed prosthodontics.7,8
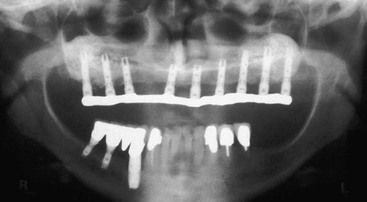
Abutment screw loosening is a complication reported for implant prostheses, especially during the first year.9,11,12 The increase in implant number also decreases the amount of forces on the abutment screws and thus reduces the risk of abutment screw loosening. As a result, many reasons justify the use of a sufficient number of implants for an independent prosthesis. So many advantages exist for an independent implant-supported fixed prosthesis with multiple units that such a treatment is always the first choice when possible (Figure 17-4).
Unfortunately, completely implant-supported fixed prostheses in partially edentulous patients are not always feasible and on occasion carry a higher surgical risk. Thus, the natural tooth occasionally may be considered a potential abutment. However, the dentist should consider splinting of implants and natural teeth within the same prosthesis only when the surface area of the implant support does not permit replacement of the total number of missing teeth and additional implant placement is not indicated.
Adjacent Bone Anatomy
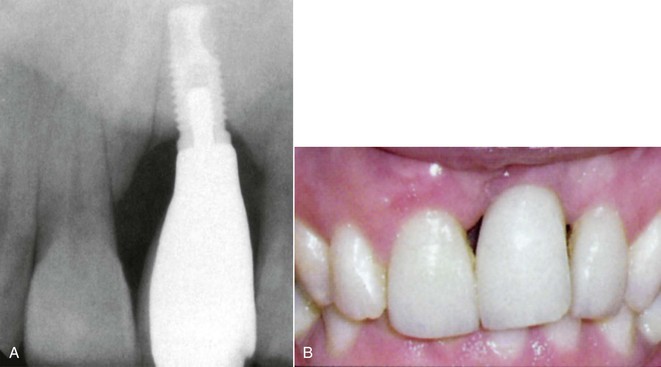
When one or more missing teeth are between existing teeth, the bone position on the adjacent roots is thoroughly evaluated, especially when the missing tooth is in the esthetic zone. Ideally, the bone on each adjacent anterior tooth next to the edentulous site should be 2.0 mm or less from the interproximal cementoenamel junction (CEJ) (which is 3 mm above the facial CEJ). When this anatomy is present, the interdental papilla adjacent to the edentulous site will be ideal because it is supported by the interproximal bone on the tooth.
The edentulous bony structure adjacent to a natural tooth varies in height, width, length, and angulation and is a reflection of the history of the former tooth, its extraction, and the period of time the site has been edentulous. If the ridge topography is not ideal for endosteal implant placement in the site immediately adjacent to the natural abutment, the dentist should consider a bone graft or a pontic. An osteoplasty needed to obtain adequate bone width in the area adjacent to a natural tooth often compromises the adjacent natural root support; increases the crown height of the final implant restoration; and affects the esthetic outcome, especially in the interdental papilla region (Figure 17-5). Therefore, osteoplasty to gain additional width is usually not indicated adjacent to a natural tooth.
If an ideal prosthodontic abutment position is adjacent to a natural tooth and inadequate bone width is available, augmentation of the edentulous site before implant insertion may improve the bone anatomy without compromising the natural abutment. In case of inadequate bone width volume adjacent to a tooth with adequate bone on the root next to the site, the dentist considers treatment options to graft the site in width to permit division A or B implant placement.
Inadequate bone height adjacent to a tooth offers a poorer prognosis for augmentation than in other situations. In general, to grow bone in height is more difficult than to grow it in width. In addition, when the inadequate bone height of the edentulous site includes the region adjacent to a natural root (and results in horizontal bone loss on the tooth root), the ability to grow additional bone height becomes even more unpredictable and is usually unsuccessful.
Bone height augmentation is not predictable on a natural tooth root with a horizontal defect. If the natural tooth root has lost bone adjacent to the site, the bone augmentation in height usually will not occur above the existing position of bone on the root. There are four alternatives for inadequate bone height adjacent to a natural tooth. The first option is orthodontic extrusion of the tooth before the bone graft. When one of the teeth has a poor adjacent bone anatomy, orthodontic extrusion to elevate the interproximal bone of the tooth is considered. The orthodontic movement will increase bone height next to the tooth and improve the bone graft prognosis. After this is accomplished, a bone graft in the implant site is more predictable (Figure 17-6). However, the tooth or teeth usually require endodontics and restoration after the orthodontic extrusion process.
A second option is extraction of the adjacent tooth and augmentation of the adjacent edentulous site and the extraction socket. This is more often indicated when only one toothadjacent to the implant site is compromised and the orthodontic extrusion is not indicated on this tooth because the amount of root in the bone is inadequate. In such cases, after the orthodontic extrusion, endodontics, and restoration, the end result is still a compromised tooth as a consequence (Figure 17-7).
The third treatment option is the fabrication of the three-unit FPD. This is often the most predictable and less expensive treatment option. In a study by Tarnow et al., if the interproximal bone to interproximal contact region of the crown is more than 5 mm, the interdental papilla will often be depressed.13 However, when this distance is 6 mm, 40% of the papilla regions will appear within normal limits, and when 7 mm, 25% of the adjacent papilla will appear normal. When the interproximal bone between the two teeth adjacent to an edentulous site is not ideal on both of the adjacent teeth but the interdental papilla is within ideal limits, consideration is given to leaving the soft tissue as it is and fabricating a three-unit FPD (Figure 17-8). If an implant is attempted and the interproximal bone is not ideal, the soft tissue often shrinks after the surgery, and the soft tissue drape is compromised around the implant and, as important, exposes the root of the adjacent teeth.
The fourth option is to place a pontic next to the natural tooth (Figure 17-9). An implant apically positioned more than 3 to 4 mm below the CEJ and interproximal bone level of the adjacent natural tooth root presents potential soft tissue contour problems (Figure 17-10). When the most distal natural tooth has inadequate bone height on the root, the soft tissue between the tooth and adjacent implant creates a more shallow slope, unlike the steep drop of the level of the bony crest between the elements. Under these conditions, a soft tissue pocket greater than 6 mm may result around the implant crown adjacent to the natural tooth (see Figure 17-5). Therefore, when a bone graft for height around a multitooth edentulous site is required to place an implant adequately adjacent to a natural root, the dentist should consider a pontic to replace the missing element next to the natural tooth. The pontic may be supported by a cantilever from implants or teeth or using dual support from teeth and implants.
In summary, if the bone is inadequate in height on the tooth root and implant site, the following should be done: (1) orthodontic extrusion and graft, (2) extract and graft two sites, (3) fabricate a three-unit FPD, or (4a) cantilever a pontic from two or more natural teeth or two or more division A implants or (4b) fabricate a fixed prosthesis with one pontic connecting an implant with one or two adjacent teeth, depending on the adjacent tooth status.
Cantilevers in Partial Edentulism
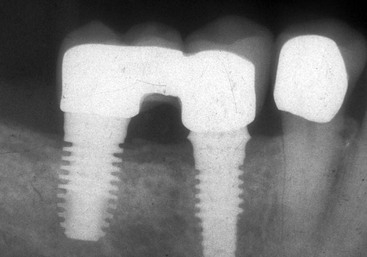
Cantilevers in fixed prostheses result in moment loads or torque on the abutments.14 They are used more frequently for implant-supported prostheses than natural teeth abutments.15,16 Several widely diverging guidelines have been recommended for the use of cantilevers in partially edentulous patients, ranging from almost no extension at all to the cantilever of several teeth.16,17 The cantilevered prosthesis is often problematic. The most common complication for a cantilevered restoration from natural teeth is uncementation of the abutment farthest from the cantilever.8,18 When a pontic is cantilevered, the abutment next to the pontics is a fulcrum, and an occlusal force on the pontic places a tensile and shear force on the more distal abutment (Figure 17-11). Cement is almost 20 times weaker in tension compared with compression forces. For example, the compressive strength of zinc phosphate cement is 12,000 psi, but its tensile strength before fracture is only 500 psi. As a result, the most common complication is an unretained crown on the more distal abutment; then the fulcrum abutment becomes mobile and loses bone, fractures, or both.
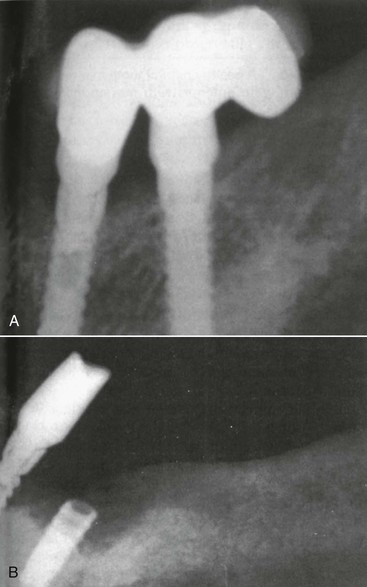
It is interesting to note that cantilevers with natural teeth abutments are rarely used in conventional prosthetics. The failure rate of a traditional three-unit FPD at 5 years is often less than 5%. However, the 5-year failure rate of cantilevered three-unit FPD is 25%, and 60% have complications.8,19 The failure is usually related to an uncemented abutment (farthest abutment from the cantilever), and the failure is biomechanical in nature. The traditional three-unit FPD fails more often from biologic conditions (e.g., decay, endodontics), which takes longer to occur. Implants are more rigid than teeth. As a consequence, the force to the cement seal is greater with implant abutments than teeth! The adjacent implant to the pontic acts even more as a fulcrum. In other words, it is worse to cantilever on implants than natural teeth (Figure 17-12).
The force on the cantilever may be compared with a class I lever. The distance between the most anterior and most distal abutments is divided by the length of the cantilever to determine the mechanical advantage to the farthest abutment from the cantilever. Takayama has suggested that the cantilever should not extend beyond the distance between the implants to keep the mechanical advantage less than one times this distance.20 The most common distance between two implant centers is 7 to 8 mm so that the outer dimensions of the implants may be 3 mm apart and the crowns on the implants are similar in size to a premolar. Thus, the size of the cantilever (when considered) should not be greater than a premolar of similar size when two implants support the three-unit prosthesis.
The most important factor in determining the safe length of the cantilever is the amount of force the patient places on the cantilever. For example, a cantilever may have a mechanical advantage (force multiplier) of two times. Hence, if a 25-lb load is applied to the pontic, a 50-lb force (tensile) is applied to the distal abutment, and 75 lb is applied to the fulcrum (class I lever mechanics). Hence the force is magnified two to three times. However, if the load on the pontic is 100 lb, it is magnified to 200-lb force on the distal abutment and a 300-lb force on the fulcrum or four times more than the first example. In other words, the amount of the force applied to the cantilever is even more important than the length of the cantilever or the distance between the implants.
Cantilevers on implants are more problematic than on teeth for several reasons. The magnification of forces are to the entire implant system. The cement or screw that retains the prosthesis may fail (Figure 17-13). The implant may fracture (Figure 17-14). The implant may become mobile and lost. These complications are often more significant than a cantilevered restoration supported by natural teeth.
Ideally, if a cantilever is necessary, it should extend mesially, rather than distally, to reduce the amount of occlusal force on the lever.6 (Figure 17-15). A cantilever of a lateral incisor from two or more adjacent implants is the least at risk because the canine tooth (implant) can protect lateral forces on the cantilever and the anterior region has less bite forces and the lateral incisor is the smallest tooth in the arch.
The crown height also influences the amount of the force on the cantilever to the cement and bone interface. The force is magni/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses