17 Laser Treatment of Vascular Lesions
Minimally invasive procedures are in great demand; unfortunately, many nonablative or minimally ablative procedures fail to provide significant results.1–5 The treatment of red and brown lesions with a combination device using 532-nm and 940-nm wavelengths (VariLite vascular laser, Iridex Corp., Mountain View, CA) is truly a lunchtime procedure that produces impressive results on a wide variety of lesions (Figure 17-1).
Dealing with ectatic vessels, birthmarks (such as port-wine stains), hemangiomas, tortuous veins, and related facial lesions was a challenge in the past. They were treated with sclerosing solutions, cryotherapy, radiofrequency needle ablation, surgical excision, and other therapies. It was not until the advent of lasers and the application of theories of selective thermolysis and thermal relaxation time that the treatment of vascular lesions advanced. Selective photothermolysis was introduced by Anderson and Parrish in 1983.6 The theory states that various target chromophores could be selectively destroyed by specific wavelengths and pulse durations, with minimal damage to surrounding tissue.
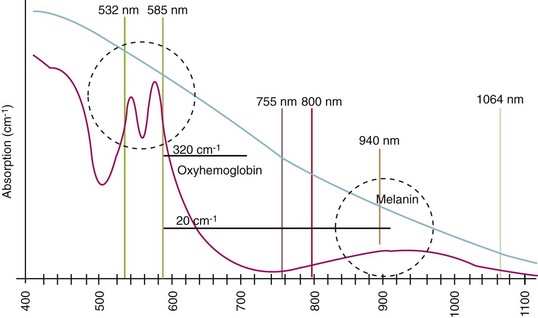
The target for vascular lesions is oxyhemoglobin. Its primary absorption peaks are at approximately 418, 542, and 577 nm in the visible spectrum, and there is a secondary absorption peak at 940 nm in the near-infrared spectrum (Figure 17-2).
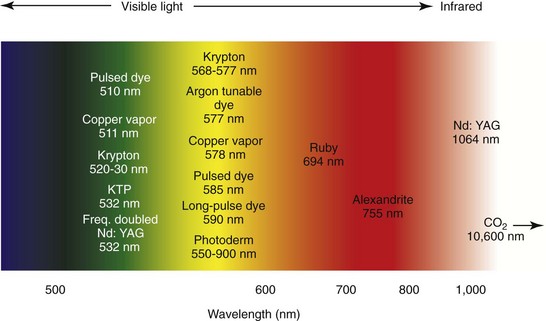
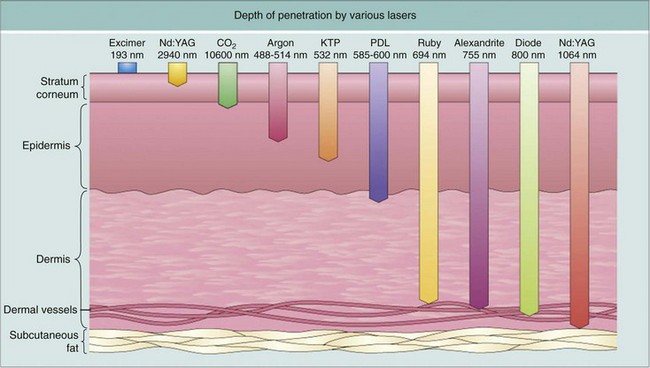
Combining our understanding of selective photothermolysis and TRT led to the development of laser technologies that are safe and effective for treating vascular lesions. Some of the earliest laser treatments for facial telangiectasias were performed using continuous-wave carbon dioxide (10,600 nm) and argon (488 and 514 nm) lasers7 (Figures 17-3 and 17-4). Although successful outcomes were reported, these lasers unselectively destroyed both ectatic vascular tissue and the overlying epidermis. These lasers were in effect sophisticated forms of electrocautery.
The theory of selective photothermolysis spurred the development of flashlamp-pumped, pulsed-dye, and copper-vapor lasers. These lasers emit light at 577- to 585-nm wavelengths that are selectively absorbed by oxyhemoglobin and can destroy the ectatic vessel with minimal damage to the underlying tissue. The pulsed-dye laser differs from older lasers in that it emits light in pulses rather than a continuous beam. The 585-nm flashlamp-pumped, pulsed-dye laser has become the gold standard by which other vascular lasers are judged. It has the significant drawback of posttreatment purpura, which is difficult to conceal and can persist for as much as 14 days (Figure 17-5).
Treatment Wavelengths
There are theories that laser energy creates a small steam bubble that expands along the axis of the vessel, clearing the lumen and pushing a column of hot blood along the vessel. As the vessel cools during its TRT, the vapor bubble condenses and collapses the vessel wall. Thermal coagulation of the blood, now ejected well beyond the actual exposure site, creates an intravascular plug, leaving an empty, thermally damaged lumen at and around the site of the laser exposure7 (Figure 17-6).
When treating larger or deeper vessels containing both oxygenated and reduced hemoglobin, or when absorption by epidermal melanin is a concern, there are significant benefits from treating at 940 nm, which targets the secondary absorption peak of oxyhemoglobin and reduced hemoglobin (see Figure 17-2). The 940-nm wavelength is emitted directly from a customized indium gallium arsenide diode laser and is chosen for larger and deeper vessels primarily because it is exactly at the peak of the secondary absorption band of oxyhemoglobin in the near-infrared region of the spectrum. Since the target is venous blood, it is also important to consider the reduced hemoglobin absorption spectrum. Less strongly absorbed wavelengths penetrate more deeply and can uniformly heat through larger-diameter vessels. Reduced hemoglobin absorption falls rapidly above 950 nm; 940 nm is the longest/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses