Chapter 17
Corrective Soft Tissue Surgery
Introduction
The aim of the protocols that have been outlined in this book is to establish clear outcomes and to base them on predictable procedures. Human variation in terms of host response might lead to unplanned outcomes requiring corrective surgery. Corrective soft tissue surgery is designed to improve the functional and aesthetic outcome in situations where compromise has taken place.
This chapter will deal with some of the surgical procedures available for the manipulation of soft tissues and provide examples of situations where they may be used.
It is essential that a clinician understands the principles underlying successful soft tissue surgery so that the techniques can be applied to a greater range of situations than those outlined here. Flowchart 17-1 provides the reader with guidance during the decision-making process with regard to the most suitable procedure. However, for the sake of convenience specific procedures will be outlined, with possible applications listed.
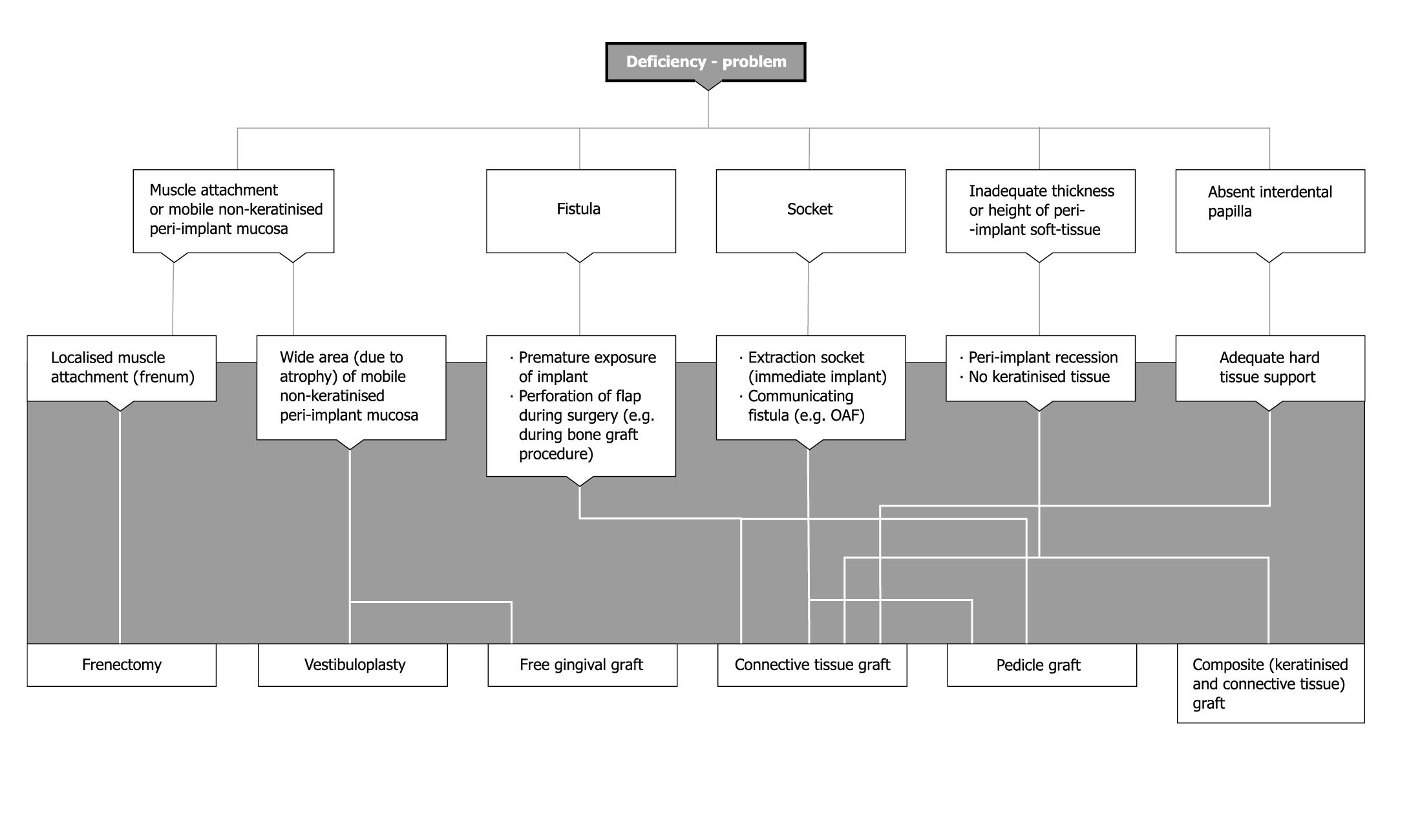
Flowchart 17-1 Corrective soft tissue surgery. OAF, oro-antral fistula.
The periodontal literature is replete with procedures designed to correct soft tissue deficiencies associated with the teeth. It is not the intention to cover these here. However, the reader should become familiar with these as they outline certain principles. Some of the procedures described in the periodontal and preprosthetic surgical literature will also be covered here because of their relevance to implant dentistry.
Vestibuloplasty
A large area of mobile non-keratinised peri-implant mucosa may result in a number of problems for the patient. These may be of an aesthetic nature where poor-quality tissue is inconsistent with the adjacent areas. A broad band of mobile tissue may also result in functional problems that relate to considerable difficulties in hygiene; these, in turn, may cause inflammation. It goes without saying that inflammation with its associated pain and swelling will result in poorer oral hygiene, which, in turn, will compound the situation.
Mobile, non-keratinised peri-implant mucosa can often be found where there is advanced atrophy and the keratinised tissue is essentially non-existent and muscle attachments are present at the level of the ridge crest. Following implant exposure, the inability of the patient to maintain normal hygiene procedures for these areas may require intervention.
The situation may also be found after bone grafting of atrophic ridges with atrophic mucosa. The situation is often made worse by advancing tissues to effect closure over the graft, which may be quite substantial in size.
Surgical Principles
A vestibuloplasty is designed to recreate a vestibule and does so by reattaching muscle insertions apically and producing non-mobile peri-implant soft tissues. The reattachment of the muscles may be enhanced by the creation of attached keratinised mucosa, using a free gingival graft. This will improve the stability of the soft tissues around implant abutments and superstructures.261–264
The surgical technique involves a partial-thickness incision around the implant abutment, which does not incise the periosteum. Care should be taken to ensure that the muscle attachments are dissected, leaving the periosteum attached to the bone. Scissors or a scalpel may be used for this procedure. The muscles are elevated with the flap and sutured to the periosteum more apically. The clinician must bear in mind that reattachment of the muscles in a more apical position may affect the facial features.
The raw exposed periosteum may be allowed to epithelialise. A dressing may be used to protect the periosteum. Alternatively, a free gingival graft can be sutured onto the periosteum, which is still attached and, therefore, ensures stability of the graft for predictable revascularisation. A free gingival graft will provide a greater thickness of attached mucosa, which is keratinised and will, therefore, enhance aesthetics and hygiene due to its greater robustness (Figs 17-1 and 17-2; see Case 1 below).
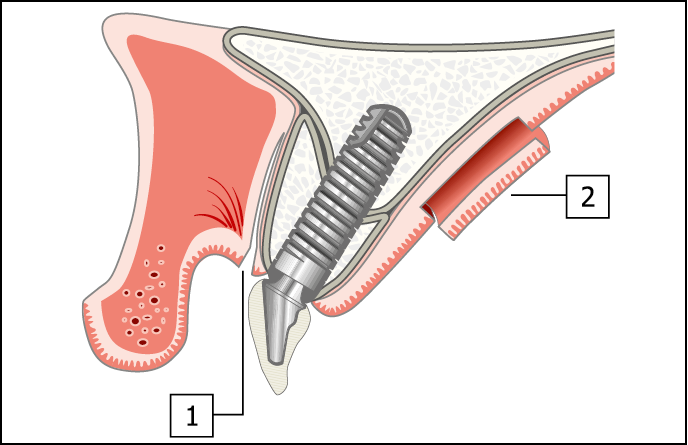
Fig 17-1 Incisions at the recipient and donor sites for vestibuloplasty and free gingival graft. (1) A split-thickness labial incision is made to reposition the muscle attachments apically. The periosteum is not elevated to ensure that the blood supply to the bone graft is maintained. (2) An incision is made for harvesting palatal keratinised tissue graft of 2-mm thickness. The superficial layer is harvested without interrupting the subepithelial mucosa, the nerve or the blood supply to the marginal tissues. This enables relatively large areas to be harvested.
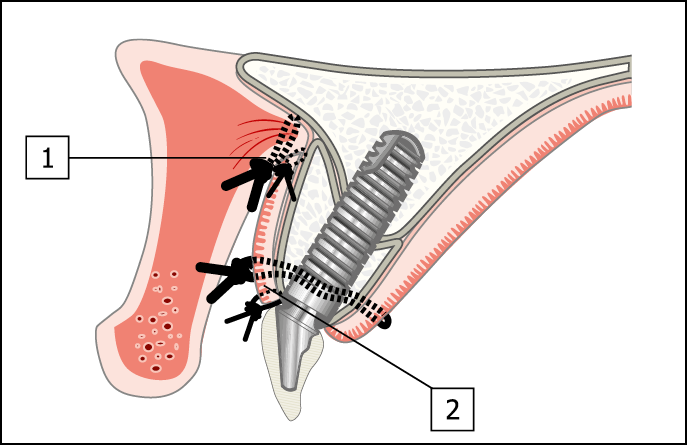
Fig 17-2 Diagram of the completed procedure. (1) The vestibuloplasty has been completed, with the muscle attachments repositioned and sutured in a more apical position using resorbable sutures (3-0 Vicryl Rapide). (2) The free gingival graft is located in place with 3-0 Vicryl sutures. The edges are secured with 6-0 Vicryl sutures to stabilise and accurately position all the margins.
Frenectomy
Localised muscle attachments that may result in a compromised outcome, such as gingival recession or marginal inflammation around an implant, should be addressed in the same manner as that outlined in the periodontal literature. Sectioning of the muscle attachment and its reattachment to an apical position is an effective way of eliminating a potential or actual problem.
Free Gingival Graft
Tissue for a free gingival graft is harvested from the palate and can be used to cover the exposed periosteum. Since the graft is non-vascularised, its blood supply is obtained from the underlying periosteum; the graft must, therefore, be completely stable and free from any movement in order to enable vascularisation to take place. It should be borne in mind that the surface texture and colour of the graft is determined by the donor site and may differ from that of the recipient site. This has some consequences for small grafts that are limited to one or two teeth.
Surgical Technique
Preparation of the Recipient Site
The preparation of the recipient site has already been outlined above for vestibuloplasty. The size of the required graft may either be measured directly or a template can be cut to fit over the area to be grafted. This will enable the graft outline to be marked at the donor site to ensure that the correct size of tissue is harvested.
Preparation of the Donor Site
Keratinised tissue is most commonly found in the palate. The amount required should be marked prior to the incision. This will ensure that the correct size is obtained. The graft is obtained using a scalpel to section an approximately 1 to 2 mm thickness of epithelial tissue. This will regenerate and re-establish the sensory innervation at both the donor and recipient sites. The donor site may be left to epithelialise or may be protected by a periodontal dressing or an acrylic resin splint.
Securing the Graft
The graft is best secured by means of sutures that will immobilise it. Vicryl 3-0 sutures may be used as locating sutures, and 6-0 sutures are most suitable for securing the graft to the periosteum. Additional stabilisation of the graft can be achieved with acrylic resin templates secured by means of a periodontal dressing.
Subepithelial Connective Tissue Grafts
Connective tissue grafts are non-vascularised and have no epithelium. They are designed to obtain their blood supply via one or both of their non-epithelialised surfaces. They are obtained from the palate and are very versatile. They have numerous applications for the closure of fistulas and the increase in soft tissue thickness.265–273
Applications
Two examples of the application of connective tissue grafts are given.
Closure of Fistulas
Connective tissue grafts lend themselves extremely well to the closure of fistulas and perforations before, during or after surgical procedures. A connective tissue graft may be used as an underlay to close a perforation in a flap made during surgery, such as a bone graft procedure. Small oro-antral fistulas can also be repaired. The principles behind these procedures are the creation of a barrier beneath the fistula or defect with a connective tissue graft, which will predictably become vascularised by the surrounding tissues through both the surfaces. The size of the area in contact with a potential blood supply increases the potential for successful revascularisation of the graft. Larger defects, such as immediate implants requiring delayed loading, will be viable only if a large connective tissue graft underlies the surrounding tissues. They may also be used to eliminate tattoos caused by amalgam used in conventional or endodontic restorations.
Increasing soft tissue bulk
Connective tissue grafts may be used in situations where compromised healing has led to a deficiency in the soft tissue. Gingival recession around the neck of an implant or the loss of an interdental papilla can be repaired with the minimum of disruption, but with only a limited degree of predictability. A connective tissue graft can be added to increase the tissue bulk by creating a pocket into which the graft can be secured. A graft of this type can also be used to create keratinised tissue, with the advantage that the connective tissue graft will attain the colour and texture of the surrounding epithelium as it epithelialises.
Surgical Techniques
Preparation of the Recipient Site
The recipient site is prepared by first creating a pocket within the tissues between the periosteum and the epithelium into which the connective tissue graft will be inserted. The size of the required graft is measured and the data transferred to the palate by way of an outline, so that a graft of the correct size and shape can be harvested. If gingival augmentation is required, the pocket is created on the labial aspect. For the correction of fistulas and defects, the pocket is prepared in such a way that the graft will block the fistula and will span beyond the margins of the fistula. In both cases, one or more sutures are used to draw the connective tissue graft into the correct position. Additional sutures are used to keep it secure.
Preparation of the Donor Site
A single incision made parallel to the ridge crest, or two incisions at right angles to each other creating an ‘L’ shape, may be used to gain access to the subepithelial connective tissue. The sequence of incisions is depicted below in Fig 17-57.
Composite Graft
Composite grafts are essentially connective tissue grafts that have had a proportion of the keratinised epithelium harvested with the subepithelial connective tissue. Establishing the vascularity of the graft will depend on the size of the surface area of the non-epithelialised connective tissue, as it is through this area that revascularisation will be achieved.
Applications
Creating Keratinised Tissue
A band of keratinised tissue can be created around the cervical margin of an implant. The graft is obtained from the palate and inserted into a pocket on the labial aspect of the implant requiring soft tissue augmentation. The graft is inserted into the pocket with the help of a suture and secured with finer sutures to precisely position the keratinised band. The graft obtains its blood supply from the interface between the connective tissue and the surrounding vascularised tissues.
Pedicle Flap
The pedicle flap described here is a subepithelial vascularised flap, which is obtained from the palate and mobilised to the area where it is required in two different ways (lateral or inverted). The choice of technique will depend on the availability of tissue. However, the blood supply to the pedicle will play a significant part in the design.
Pedicle flaps can be used for the closure of fistulas (e.g. oro-antral fistula), for the creation of soft tissue bulk and for the creation of attached keratinised tissue.
Applications for the Closure of Epithelial Continuity Defects
Oro-antral Fistulas
Pedicle flaps provide an excellent and predictable way of closing oro-antral fistulas without the loss of attached tissue, which would occur if a buccal advancement flap is used. The viability of the flap, coupled with its insertion into a subepithelial pocket surrounding the defect, offers predictable closure of the defect without anatomical compromise. Subsequent procedures to repair any bony defects can easily be carried out.
Socket Closure after Immediate Implant Placement
Immediate placement of implants at the time of extraction may well be coupled with immediate loading or transgingival healing. However, where adequate stability of the implant has not been achieved, delayed loading becomes necessary. The pedicle flap can very effectively provide soft tissue coverage over the resultant socket without the loss of attached tissue. In addition, the bulk of the labial soft tissues can effectively be increased.
This procedure may be indicated where immediate placement of the implants is desired but the soft tissue contours need to be improved. A pedicle flap will improve the soft tissue contours and enable the loading to be commenced six weeks after implantation.
Closure over Bone Grafts
Where there are palatal bone deficiencies and a crestal incision has been used to gain access to the bony crest, closure of the wound may be difficult to achieve. In these cases, a pedicle flap may be used.
Closure over Implants
Closure over implants may become necessary where additional hard or soft tissue augmentation procedures need to be carried out after implant exposure. This may occur after the completion of the prosthetic phase. Closure over the implant can be predictably achieved without palatal repositioning of any labial keratinised mucosa.
Applications for Increasing Soft Tissue Bulk
Creating Interdental Papillae
Interdental papillae can be created with a pedicle flap provided that there is adequate bone support. The vascularity of the flap results in a sustainable increase in papillary height.
Creating Labial Soft Tissue Bulk
Increasing the bulk of the soft tissue on the labial aspect of the implant can be achieved using this technique prior to implant exposure. However, if this procedure is carried out after exposure of the implant, the treatment will involve removal of the abutment and closure over the implant. The use of an interim provisional restoration will then be necessary while the graft heals, and the implant will be exposed at a later stage. It may be necessary to use a different abutment if the recurrence of recession is to be avoided.
Surgical Technique
The design of the flap should comply with two basic principles:
- • maintenance of an adequate blood supply
- • mobilisation of sufficient tissue to successfully meet the objective.
Access to the subepithelial connective tissue is gained by elevating the palatal epithelium using a split-thickness flap. The incision design will depend on the location of the recipient site and the type of flap that is to be used. The shape of the connective tissue required for the flap is incised, often to include the periosteum. This is elevated and transferred to the recipient site, maintaining an intact blood supply. The insertion of the connective tissue flap must be subepithelial and must not overlie any region of epithelium. Attachment of the connective tissue to the recipient site can then be assured.
A suture (3-0 Vicryl) may be used to draw the edge of the flap into the subepithelial pocket that has been created. Additional fine sutures (6-0 Vicryl) may be used to approximate the margins more precisely. The split-thickness epithelial flap is then repositioned and sutured over the donor site and a proportion of the flap.
Lateral Pedicle Flap
The lateral pedicle flap is most commonly used in the second premolar and molar regions for either of the purposes described above. This type of flap is extremely reliable as it can be designed to receive an abundant blood supply from the greater palatine vessels. There is usually sufficient tissue present in the anterior part of the maxilla to allow it to be displaced laterally over the recipient site.
The incision is made within the socket or fistula that requires coverage. The split-thickness incision is extended anteriorly along the crest of the ridge adjacent to any remaining teeth. The anterior extent of the incision will be limited by the thickness of the tissue under the rugae and by the anterior teeth.
Planning for surgery will, therefore, require the thickness of the tissues to be measured preoperatively. Local anaesthetic needles provide an atraumatic and effective way of doing this. At the anterior extent of this incision, a perpendicular split-thickness incision provides access to the subepithelial connective tissue. The incision is then extended distally as required. The split-thickness flap is elevated carefully, ensuring that no perforation of the connective tissue through to the bone takes place.
The outline of the pedicle flap is incised using two parallel incisions running mesiodistally. A perpendicular incision is then made at the anterior to limit the length of the flap. The parallel incisions may need to be extended distal to the defect to provide sufficient mobility of the flap.
The flap can be elevated as required and rotated laterally to cover the defect or bulk the labial tissue. The flap must not cross the epithelium and must be inserted into a pocket created within the subepithelial tissue on the labial aspect of the defect. The graft is drawn into the pocket and secured with 3-0 Vicryl sutures, while 6-0 Vicryl sutures can be used to fix the graft precisely and to reposition the split-thickness epithelial flap.
Inverted Pedicle Flap
The inverted pedicle flap is most commonly used in the incisor or canine regions. This is often because there is limited tissue available for lateral transposition in these areas. Although there are occasions when tissue can be transferred across the midline, this is generally not possible because of the thin tissue in the midline and the compromised blood and sensory nerve supply.
The incision for the split-thickness epithelial flap is made within the margins of the socket or fistula that requires covering. The distal extension of the incision is made alongside the alveolar crest so that the maximum benefit is derived from the palatal blood supply. Access may be extended as far back as the distal aspect of the second molar, provided that the incision is not in close proximity to the midline. If a broader graft is required, the distal extension should not go beyond the distal aspect of the first molar to ensure that there is no interruption of the neurovascular supply from the greater palatine foramen.
The pedicle is incised using two parallel incisions running along mesiodistally. The distal incision perpendicular to the parallel incisions will interrupt the blood supply from the greater palatine vessels. The success of the pedicle graft will, therefore, depend on the collateral blood supply and will require a large area of attachment to the underlying bone on the anterior aspect of the pedicle flap. Typically, for one unit of the pedicle flap that will remain attached to the underlying bone, two units of pedicle will be required. It should be borne in mind that, of the two units of the inverted flap, one will overlay the attached portion and only one unit will be available for the required purpose.
Corrective Soft Tissue Surgery:
Clinical Cases
Case 1: Vestibuloplasty and Free Gingival Graft
This case study demonstrates the use of vestibuloplasty and a free gingival graft to recreate a sulcus following bone graft surgery.
A 60-year-old woman presented with extensive hard and soft tissue deficiencies. These were corrected using bone grafts harvested from the iliac crest. A remote palatal incision was used. Soft tissue coverage of the grafts resulted in the loss of the vestibular sulcus (Figs 17-3–17-16).
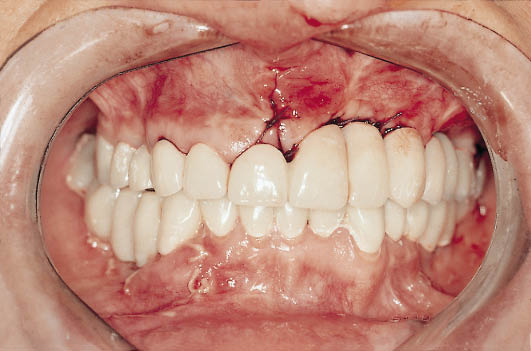
Fig 17-3 Labial view of the patient at the start of treatment, showing the provisional metal-acrylic bridge in situ. The extent of deficiencies on the patient’s left-hand side is apparent from the increased length of the teeth.

Fig 17-4 Labial view of the provisional maxillary restoration following bone graft surgery. The ridge has been overcontoured to compensate for the remodelling process. The reduced size of the teeth on the provisional restoration as well as the loss of sulcular height is evident. No keratinised attached tissue can be seen.

Fig 17-5 Labial view of the definitive maxillary metal-ceramic restoration showing good tooth form.

Fig 17-6 Close-up of the maxillary teeth emerging through non-keratinised mobile soft tissues.

Fig 17-7 The laboratory cast showing a clear vacuum-formed splint for the protection of the palate following the harvesting of the keratinised soft tissue graft.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


