Implant Dentistry: Challenges in the Treatment of the Edentulous Patient
Steven J. Sadowsky1, Howard M. Landesman2, and W. Peter Hansen1
1 University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco, California, USA
2 Encino, California, USA
When considering the impact of innovation, it is noteworthy that only 1 per 1000 articles has studied undesirable consequences from new discoveries, a proportion that has not changed since the 1960s, as reported in a position paper by the Hanken School of Economics in 2009. This is explained by pro‐innovation bias or the fundamental value that innovation is good. However, this widespread attitude may limit decision makers and change agents to anticipate and respond to unforeseen outcomes. Perhaps, as a result of the salvation that dental implants have offered edentulous patients, such an analysis would be sacrosanct. However, enhanced patient‐centered care may hinge on it. As clinicians and academicians, we are in an opportune position to identify and address these trends.
Since the introduction of the osseointegration concept to North America in 1982, there has been a number of unexpected discoveries that have changed the therapeutic model for treatment of the edentulous patient. The advent of affordable and low‐dose radiation three‐dimensional (3‐D) imaging, using cone‐beam computed tomography (CBCT) with attendant software programs, has enabled virtual treatment planning from surgical placement to prosthetic design.1 Further developments have included a digital implant workflow, allowing for fabrication of surgical guides,2,3 interim abutments and provisional prostheses prior to implant surgery,4 intraoral scanning for complete arch impressions,5 and ultimately CAD/CAM production of the definitive restoration.6,7 The developing science of surface topography of dental implants has focused on enhanced formation of osteoblastic proliferation on titanium implants.8–10 Data now have demonstrated an upregulation of genes associated with signaling osteogenic differentiation following early exposure of osteoprogenitor cells to moderately roughened surfaces.11,12 These investigations have influenced original clinical guidelines for the time span necessary between implant placement and loading the prosthetic rehabilitation.13–15 Coupled with the evidence from systematic reviews on the similar fate of tilted and orthogonally placed implants for edentulous arches,16,17 the “All‐on‐4” concept has gained immense traction in the prosthodontic community. Anatomic limitations, including pneumatized maxillary sinus, proximity of the inferior alveolar nerve, and lack of available native bone, usually requiring invasive and costly grafting procedures prior to implant placement, have been circumvented. In line with reducing surgical morbidity, cost, and failure rates, augmentation procedures have been replaced with the use of four zygomatic implants when addressing severe atrophy of the maxilla.18,19 Considering oral health‐related quality‐of‐life indices and patient preferences for minimally invasive procedures, graftless implant rehabilitation of complete edentulism has become more mainstream. It is notable that patient satisfaction averaged 94% with tilted implant placement, 91% with flapless implant placement, 90% with a reduced number of implants, 89% with short implants, 87% with narrow‐diameter implants, and 83% with zygomatic fixtures.20 Another example of this “less is more” direction is the evolution from the original ad modum Branemark prototype with six implants for the rescue of the mandibular denture cripple to a solitary symphyseal implant‐retained overdenture for a selected cohort of patients.21–23
The aforementioned advancements have the potential to improve our diagnostic acumen, render care in an expeditious time period, circumvent extensive and costly preprosthetic surgery, and offer patients more cost‐effective outcomes. With that in mind, one would think that the discipline of implant prosthodontics is moving swiftly down the highway of customized treatment planning with an emphasis on minimally invasive procedures. However, the elephant in the room is the burgeoning reputation that implants are the deus ex machina for all patients requiring minimal surveillance for life. This myth, in conjunction with six prevailing trends, has, on the contrary, resulted in a diminished ability to conservatively treat edentulous patients and an increased likelihood of implant prosthodontic mishaps.
Education
The teaching of complete denture prosthodontics has been marginalized in dental school curricula.
Due to crowded curricula, because of advances in technology24 and implant rehabilitation,25 along with decreasing edentulism,26 there has been a progressive diminution of didactic, laboratory, and clinical training in complete denture prosthodontics.27,28 New graduates are now less well equipped to practice complete denture prosthodontics than in the 1990s.29 Dental schools have low expectations for their undergraduate students to be practically trained in the production and insertion of complete dentures, with lead teachers reporting that course work did not ensure competence on graduation.30,31 Despite that fact 63% of graduates felt complete dentures were an important aspect of dentistry, only 5% expressed confidence in removable prosthodontics.32 A decreased load of core coursework and clinical reinforcement in complete denture principles, incorporating the sphere of troubleshooting denture complications, diagnostic criteria for edentulism, vertical dimension of occlusion (VDO), occlusal harmony, and esthetic arrangement of teeth, has spawned poor management of both conventional and implant prosthodontics.
Troubleshooting denture complications
A typical patient presents with a nonretentive maxillary denture. Instead of assessing the peripheral seal, width of the flange, the allowance for muscle attachments, intimacy of fit of the intaglio surface, and occlusal harmony, a reline is recommended. When this fails, the discussion migrates to implant prosthetic options. For example, if the vibrating line (junction between the movable and immovable soft palate) is up to 8 mm anterior to the distal limit of the denture (Figure 16.1) and there is space in the retrozygomatic vestibular region between the flange and fornix (Figure 16.2), a reline that does not address these deficiencies is destined for failure. When this occurs, the patient considers the “evidence” that a tissue‐borne prosthesis offers little benefit for dependable retention and stability. On the other hand, if the distal limit is adjusted, the flanges are developed by functional border molding, and a thin wash is placed in the relieved intaglio of the denture (Figure 16.3),33 followed by occlusal equilibration, the clinician and patient have the opportunity to assess the prospect of conservative conventional treatment. However, the edentulous mandible has routinely offered more challenges to patients to adapt to a tissue‐borne prosthesis, which especially has been predicated on systemic,34,35 local,36,37 and psychosocial factors.38–40 Ironically, the introduction of implants for the restoration of the edentulous mandible has facilitated a progressive erosion of the education in complete denture prosthodontics.


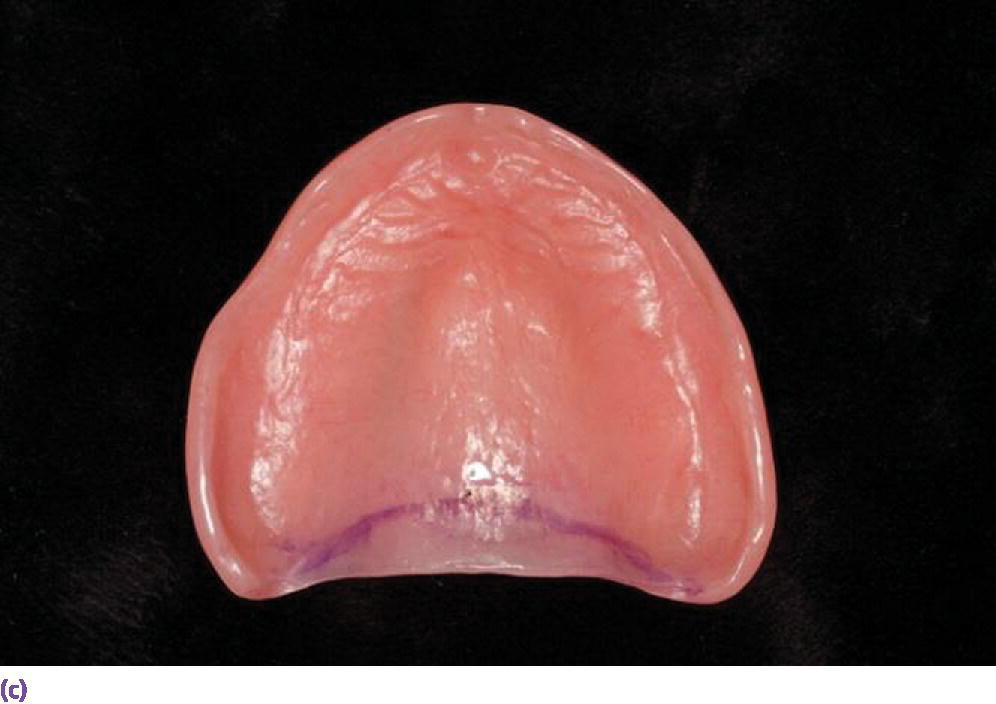
Figure 16.1 (a) Vibrating line established with indelible marker. (b) Denture in place, demonstrating distal limit engaging the movable soft palate beyond the vibrating line. (c) Vibrating line visible on intaglio surface of denture.

Figure 16.2 Peripheral seal lacking with short flange in the retrozygomatic region.

Figure 16.3 Tissue conditioner used first to develop the periphery with a higher viscosity powder/liquid ratio and then a very thin wash for the intaglio surface.
Diagnostic criteria for complete edentulism
In 2002, the McGill Consensus concluded that the minimum standard of care for the edentulous mandible was a two‐implant overdenture.41 This statement did not differentiate among different classes of edentulism, patients’ prognosis for success with complete dentures, or their limitations in embracing an implant therapy. To address the question posed by the edentulous patient, “Do I need implants?”, the focus is generally directed to the mandibular arch. In an attempt to organize the diagnostic criteria for complete edentulism, McGarry et al.42 introduced a classification system for pretreatment evaluation of patients considered for complete dentures (Table 16.1). The Prosthodontic Diagnostic Index identified two classifications (class III and IV) which were in need of implant/surgical intervention. These included patients with residual ridge deficiencies, muscle attachments challenging retention (Figure 16.4a), history of parethesia/dysesthesia, incoordination, retracted tongue position (Figure 16.4b), hyperactive gag reflex, and, most importantly, a high maladaptive quotient. Since 10–15% of patients receiving new and technically well‐made dentures, and 25–35% with older dentures, are generally not satisfied with the treatment because of maladaptive tendencies,43 Friedman et al.44 offered a classification system to assist the clinician in identifying a spectrum of physical and psychological maladaptive responses of patients who are made edentulous. Therefore, despite the advent of implants, for a class of patients that physically, anatomically, and psychosocially present with favorable conditions, a tissue‐borne prosthesis is a viable option, especially for the patient with financial limitations. On the other hand, there has been a presumption that implants not only can overcome anatomic deficiencies but also maladaptation. In this regard, it is notable to consider that implant patients have higher expectations than those treated with conventional prostheses.45 Over 60 years ago, M.M. House delineated four different personality profiles influencing the prognosis of complete denture therapy (philosophical, exacting, hysterical and indifferent). His classification still has relevance in the decision to rehabilitate the patient conventionally, with implants or not at all. In the final resolve, adding implants to the arsenal of therapeutic options for patients should not minimize the effective application of tissue‐supported prostheses for selected patients or underestimate the role that psychosocial issues have in accommodating to implant prostheses.
Table 16.1 Checklist for prognostic classification of complete edentulism.
Source: reproduced with permission from the American College of Prosthodontists.
| Class I | Class II | Class III | Class IV | ||
| Bone height – mandibular | |||||
| 21 mm or greater | |||||
| 16–20 mm | |||||
| 11–15 mm | |||||
| 10 mm or less | |||||
| Ridge morphology – maxilla | |||||
| Type A – resists vertical and horizontal movement, hamular notch, no tori | |||||
| Type B – no buccal vestibule, poor hamular notch, no tori | |||||
| Type C – no anterior vestibule, min support, mobile anterior ridge | |||||
| Type D – no anterior/posterior vestibules, tori, redundant tissue | |||||
| Muscle attachments – mandibular | |||||
| Type A – adequate attached mucosa | |||||
| Type B – no buccal attached mucosa (22–27), + mentalis m | |||||
| Type C – no anterior buccal and lingual vestibule (22–27), + genioglossus & mentalis m | |||||
| Type D – attached mucosa in posterior only | |||||
| Type E – no attached mucosa, cheek/lip moves tongue | |||||
| Maxillomandibular relationships | |||||
| Class I | |||||
| Class II | |||||
| Class III | |||||
| Conditions requiring preprosthetic surgery | |||||
| Minor soft tissue procedures | |||||
| Minor hard tissue procedures | |||||
| Implants – simple | |||||
| Implants with bone graft – complex | |||||
| Correction of dentofacial deformities | |||||
| Hard tissue augmentation | |||||
| Major soft tissue revisions | |||||
| Limited interarch space | |||||
| 18–20 mm | |||||
| Surgical correction needed | |||||
| Tongue anatomy | |||||
| Large (occludes interdental space) | |||||
| Hyperactive – with retracted position | |||||
| Modifiers | |||||
| Oral manifestation of systemic disease | |||||
| Mild | |||||
| Moderate | |||||
| Severe | |||||
| Psychosocial | |||||
| Moderate | |||||
| Severe | |||||
| Temporomandibular joint disorder symptoms | |||||
| History of paresthesia or dysesthesia | |||||
| Maxillofacial defects | |||||
| Ataxia | |||||
| Refractory patient | |||||
| ICD‐9‐CM diagnostic codes | 525.41 | 525.42 | 525.43 | 525.44 | |
| Guidelines for use of the worksheet | |||||
|
|||||


Figure 16.4 (a) High muscle attachment which negatively affects the prognosis of a complete denture. (b) Retruded tongue compromising prognosis of complete denture leading to appropriate implant treatment.
Vertical dimension of occlusion
The ability to assess the appropriate vertical dimension of occlusion (VDO) is paramount in predictable prosthodontics for the edentate as well as for the dentulous patient who has lost adequate vertical stops. Historically, predoctoral training in complete denture fabrication offered students multiple opportunities to practice calibrating this measurement. Errors in establishing the correct VDO could be seen as causing contact of teeth when speaking or a collapsed edentulous appearance. As complete denture education waned, more sophisticated implant rehabilitations requiring this skill were at risk of being mismanaged, often with irreversible consequences. Various prosthetic modalities, such as implant overdentures (with diverse anchorage systems and dimensional requirements), implant‐fixed complete dentures, and metal–ceramic designs, all require different interarch spatial allowance.46,47 Specific guidelines are discussed in Chapters 17 and 18. Errors in this calculation not only may handcuff accurate surgical planning for alveoplasty, but once the implants are placed, the intended design may not be able to be executed. Insufficient space afforded for the prosthetic components often leads to material fatigue and/or fracture.48
There are several techniques for determining the correct VDO. These methods include the use of physiologic rest position, swallowing, phonetic, esthetic, and facial measurements. Today these techniques seem difficult for students to grasp without focused training. There is consensus that the use of multiple determinants is helpful in establishing VDO.49–51 One measurement used is the vertical dimension of rest (VDR),52,53 which is the mandibular position assumed when the head is in an upright position54 and the involved muscles, particularly the elevator and depressor groups, are in equilibrium in tonic contraction and the condyles are in a neutral and unstrained position. The interocclusal distance (IOD) is the space between VDR and VDO (Figure 16.5). A weak correlation has been documented between speaking /s/ space and IOD.55 For class I patients there is approximately 3 mm of IOD, class II patients more than 3 mm and class III patients less than 3 mm.56 A 15‐year longitudinal study using lateral cephalometric radiographs to record the VDO of patients after assessment of VDR, the “m”57 and swallowing58 technique, confirmed a small range of stability in all subjects throughout the follow‐up.59 Esthetic and facial analyses have also been recommended to verify VDO.60–62
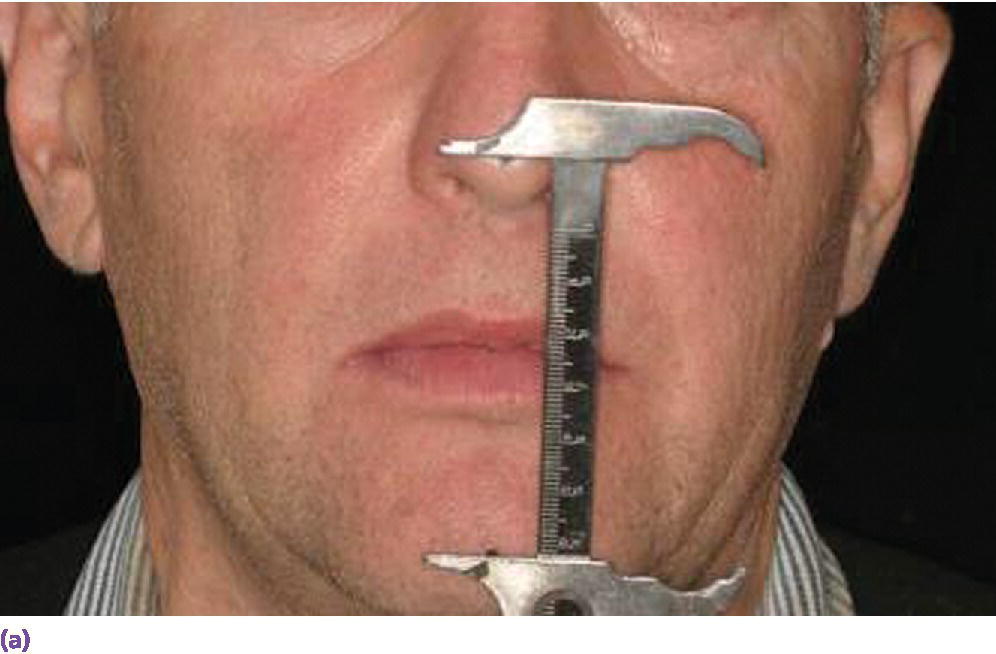
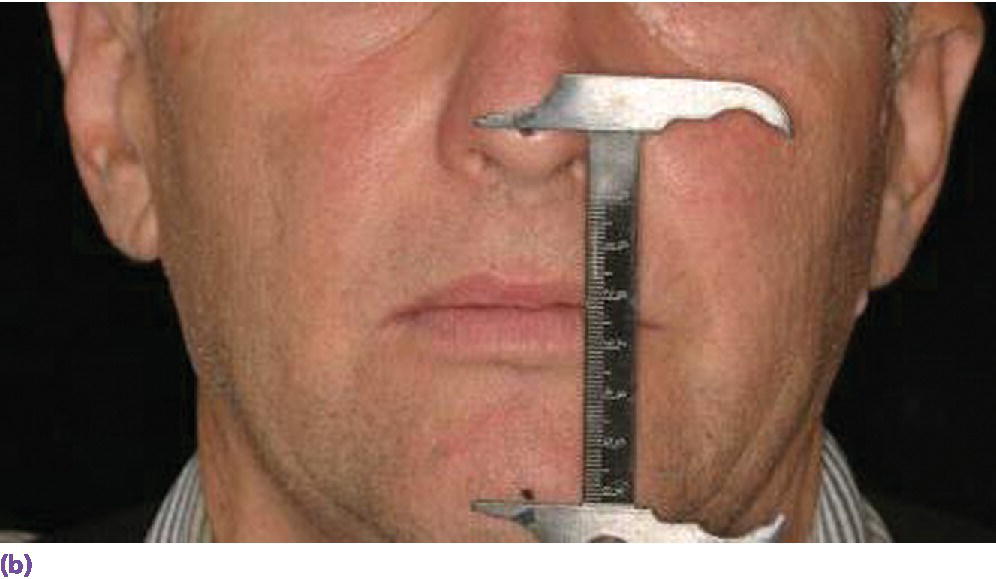
Figure 16.5 (a) Vertical dimension of rest (VDR) recorded with a boley gauge. (b) Vertical dimension of occlusion (VDO) registered with less than 1 mm difference between VDR and VDO. This demonstrates insufficient interocclusal distance for a class I patient.
Occlusal harmony
It has been said that there is no better discipline to learn occlusal concepts and equilibration than complete denture prosthodontics (Figure 16.6). Identifying the interrelationship of the occlusal plane, curve of Spee, curve of Wilson, condylar inclination, and incisal guidance is facilitated when balanced set‐ups are generated. There is little debate that a harmonious occlusion in various forms improves the stability and comfort of a tissue‐borne prosthesis.63,64 The clinical remount allows for a recording of guided ligamentous centric relation position, a verifiable occlusal record, and the opportunity to identify disruptive occlusal interferences (Figure 16.7). However, the teaching of complete denture occlusion has been marginalized in the dental school curriculum.56
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


