16
Dental Caries, Tooth Fracture and Exposed Dental Pulp: The Role of Endodontics in Orthodontic Treatment Planning and Mechanotherapy
Primum non nocere
Hipoccrates (c.460 to c.377 BC)
Summary
For the past 15–20 years, social scientists and observers of contemporary life have been commenting on the dramatic change in the way business is done in both the public and private sectors. The change that has attracted so much attention and commentary is a significant increase in teamwork and collaborative efforts: people with different views and perspectives are coming together, putting aside their narrow self-interests, and discussing issues openly and supportively in an attempt to solve a larger problem or achieve a broader goal. Teams come together for a number of different reasons, but their goals are the same – to achieve peak performance and experience success. We as dental specialists share the same goal. We want to have happy and satisfied patients with acceptable, even better, facial and dental esthetics with healthy, functional, and stable occlusions. In a beauty-addicted society where a good smile is a powerful weapon, the demand for orthodontic treatment is increasingly rising, and in challenging situations, input from a number of dental disciplines is required to construct detailed treatment plans.
This chapter comprises a comprehensive review of topics requiring interactive cooperation or teamwork between the orthodontist, endodontist, and/or conservative dentistry specialist. Topics such as enamel demineralization around orthodontic attachments, pulpal reactions, root resorption or invasive cervical resorption due to orthodontic treatment, and special considerations about dental trauma will be discussed in detail.
Introduction
An increased desire towards improved facial esthetics and dental appearance is the key motivating factor for orthodontic treatment in every population. These appearance-conscious patients and/or their families request esthetic treatment plans that usually require a comprehensive interactive approach. Coordinated orthodontic, endodontic, and restorative treatments, with careful consideration of patients’ and their families’ expectations and requests are critical for successful outcomes and patient satisfaction (Vitale et al., 2004). Clearly, it is the orthodontist’s responsibility to take a proactive role in forming close cooperation between the disciplines to reach the ultimate goal of achieving healthy esthetics and function, while at the same time limiting undesirable consequences and risks of mechanotherapeutics.
Optimized treatment outcomes necessitate close collaboration between the disciplines to evaluate, diagnose and resolve problems at the following stages of the treatment life cycle:
- Pretreatment evaluation and the early stages of the orthodontic treatment
- Orthodontic treatment
- Emergency orthodontic treatment in trauma cases
- Immediate post-orthodontic period and during orthodontic retention.
This chapter reviews and summarizes the need and benefit of interactions between orthodontists, endodontists, and/or conservative dentistry specialists according to the stages of orthodontic treatment mentioned above.
Pretreatment Evaluation and Early Orthodontic Treatment
Successful orthodontic therapy relies on the accurate assessment of the pretreatment dental and gingival health status with the aid of other dental disciplines. The assessment should include a determination of systemic and/or local factors, and obtaining a detailed history of previous trauma to the oral tissues. The initial clinical examination should precede basic radiographic evaluation, which will help the clinician to decide on precautions to minimize the undesirable effects of orthodontic mechanics. It should not be forgotten that every patient is unique, and demands and merits a unique treatment plan customized for his/her specific needs.
Endodontically Treated Teeth
The decision of whether or not to extract tooth/teeth is an important step in designing concrete orthodontic treatment procedures. If the orthodontist judges a case as one requiring extraction, the next step will be the decision regarding which tooth/teeth to extract (Yagi et al., 2009). There may be multiple options and choosing one of the potential teeth requires consideration of parameters that might require a consultation with specialists from other disciplines. For example, a history of root canal treatment or the presence of periapical lesions, restorations, and carious teeth complicates the decision about the site of extraction. In such cases, the decision should be the one that optimizes the orthodontic treatment prognosis with less invasive operative intervention.
Successful root canal treatment relies on adequate removal of microorganisms and prevention of re-colonization or re-infection through the placement of a root canal filling that obliterates the canal space and a restoration with good coronal seal (Briggs and Scott, 1997). The benefits of root canal treatment are: retention of the natural tooth in the dental arch and facilitation of the restoration to conserve the remaining crown and root structures, preservation of the alveolar bone and accompanying papillae, and maintenance of pressure and tension perception by paradental mechanoreceptors. However, such a retained tooth may be at risk of a future root fracture and development of caries or periodontal disease after orthodontic treatment (Torabinejad et al., 2007). Epidemiological radiographic surveys have revealed a relatively low frequency of high-quality root canal fillings, ranging from 14% to 65% (Eriksen et al., 2002).
Endodontic outcomes are difficult to predict since non-endodontic factors such as the quality of the subsequent restoration and the remaining tooth structure contribute to the true prognosis. Whenever the decision has to be made about whether to perform endodontic treatment or to extract a tooth, orthodontists should consult with endodontists taking into account pre-, intra-, and postoperative factors, such as the patient’s age, socioeconomic class, vital or necrotic pulp, and presence of periapical infections (Travassos et al., 2003). It is important to realize that the presence of periapical lesions, increased age, and the presence of irregular canal anatomies especially in molars may compromise the endodontic outcome. Moreover, procedural errors during canal instrumentation, rinsing with irrigation solutions, and medicaments and fillings may play a crucial role in long-term prognosis. These factors should be evaluated based on good clinical judgment along with input from endodontists, so that the patient is provided with an optimized treatment plan, which is at the same time cost-effective.
Endodontically treated teeth can be moved orthodontically as readily as teeth with vital pulps. If teeth require root canal treatment during orthodontic movement, it is recommended that the root canals be cleaned, shaped, and an interim dressing of calcium hydroxide be placed. Canal obturation is accomplished after orthodontic treatment (Hamilton and Gutmann, 1999). If orthodontic treatment might take too long to finish, a gutta-percha filling should be placed in-treatment, because the calcium hydroxide filling may make the tooth prone to fracture during this period.
Cariogenic Potential and White Spot Lesions
After the decision about the final treatment plan, before the full bond-up appointment, the clinician should take measures against cariogenic challenge. Dental caries in the enamel is unique among other infective diseases in the human body, as enamel is both acellular and avascular; thus enamel cannot heal itself by a cellular repair mechanism (Zero, 1999). In orthodontic patients, caries starts as decalcification areas adjacent to fixed orthodontic appliances. Earlier studies demonstrated increased cariogenic risk associated with a rapid increase in the volume of dental plaque, which has a lower pH and significantly elevated levels of acidogenic bacteria such as Streptococcus mutans around orthodontic attachments than in nonorthodontic patients (Chatterjee and Kleinberg, 1979; Gwinnett and Ceen, 1979). These acidogenic bacteria produce byproducts of organic acids in the presence of fermentable carbohydrates, further lowering the pH of the plaque. As the pH drops below the threshold for remineralization (pH = 4.5), enamel demineralization/decalcification occurs. The first clinical evidence of this demineralization is visualized as a white spot lesion (WSL), which has been defined as ‘subsurface enamel porosity from carious demineralization’ that represents itself as ‘a milky white opacity’ caused by the changes in enamel translucency and light scattering (Bishara and Ostby, 2008).
WSLs are clinically induced in less than 4 weeks (Ogaard et al., 1988), and their prevalence is reported to vary from 4.9% (Gorelick et al., 1982) to 84% (Mizrahi, 1982) of tooth surfaces. More than 50% of subjects may experience an increase in the number of WSLs with fixed orthodontic appliance therapy (Artun and Brobakken, 1986). Boersma et al. (2005) observed that 97% of all their subjects and on average 30% of the buccal surfaces in a person were affected. Again, on average, 40% of the surfaces in males and 22% in females showed white spot lesions. Briefly, any tooth in the mouth can be affected, with the common ones being the maxillary lateral incisors, maxillary canines, and mandibular premolars. Diagnosis, prevention, and treatment of WSLs are all crucial to prevent tooth decay as well as to minimize the tooth discoloration that could compromise the smile esthetics.
The acquired biofilm (the pellicle) in the intact enamel surface participates in dynamic physico-chemical equilibrium with the oral fluids (Zero, 1999; Ten Cate and van Loveren, 1999). When the pH of the oral fluids goes below the physiological norm, calcium and phosphate ions diffuse from the hydroxyapatite mineral in the enamel to the pellicle and into the oral cavity (demineralization). When the pH of the oral fluids rises to the norm, the calcium and phosphate ions in the supersaturated saliva are transmitted through the pellicle into the enamel following the laws of chemical equilibrium (remineralization). Within this cycle, destructive demineralization and restorative remineralization occur either simultaneously or alternately. If this cycle is not prevented and demineralization predominates, WSLs will be the result and once established, it is extremely difficult, or sometimes impossible, to achieve complete remineralization.
The most important prophylactic measure against WSLs is implementation of a good dietary and oral hygiene regimen along with proper tooth brushing with a fluoridated dentifrice. The remineralization process is greatly enhanced by the low levels of fluoride in the saliva and plaque (Ten Cate and van Loveren, 1999). According to Lima et al. (2008), by controlling biofilm accumulation with a fluoride-containing dentifrice, the lesions can not only be arrested but also be partially repaired. Dentifrices typically contain sodium fluoride, monofluorophosphate, stannous fluoride, amine fluoride, or a combination of these compounds, but the maximum concentration allowed in the European community is 0.15%. Ogaard et al. (2004) demonstrated a dose–response effect and a fluoride concentration above 0.1% in dentifrices is recommended for orthodontic patients, because of their increased risk of WSLs.
Stannous fluoride, which interferes with the adsorption of plaque bacteria to the enamel surface, offers beneficial effects not only against caries but also against plaque-induced gingival diseases during orthodontic treatment (Ogaard et al., 1980; Boyd and Chun, 1994). Tin atoms in stannous products block the passage of sucrose into bacterial cells, inhibiting acid production. Ogaard et al. (2006) demonstrated an inhibiting effect of a combined stannous fluoride/amine fluoride toothpaste/mouth rinse against both decalcification and gingival bleeding in a prospective, randomized clinical study. Titanium tetrafluoride solutions through formation of the retentive, titanium-rich, glaze-like surface coating on treated enamel surfaces inhibit caries lesion development in patients wearing fixed appliances. At a low pH, titanium binds with an oxygen atom of a phosphate group to form Ti-O-Ti-O-chains on the tooth surface and this covalently bound titanium covers the tooth surface by formation of a strong complex. This surface coating resists cariogenic challenges even under extreme alkaline and acidic conditions (Büyükyılmaz et al., 1994).
The effect of fluoride is limited when the pH level drops to lower than the solubility product of pure fluoroapatite (pH = 4.5). When this pH is exceeded, the liquid phase of the plaque will be undersaturated with hydroxyapatite and fluoroapatite making remineralization no longer possible (Larsen, 1990). A dose response to fluoride may not be apparent in this stage and more fluoride may not produce a better clinical effect (Ogaard, 2001). Briefly, if the patient is noncompliant with the implemented hygiene and dietary precautions, the use of a fluoridated dentifrice alone may not be effective in preventing the development of WSLs (O’Reilly and Featherstone, 1987). Supplemental professional sources of fluoride and other antimicrobial agents in the forms of varnishes, solutions or gels are often recommended. Fluoridated mouth rinses containing 0.05% sodium fluoride used daily have been shown to significantly reduce lesion formation beneath bands. These mouth rinses may be combined with antimicrobial agents such as chlorhexidine (CHX), octenidine dihydrochloride, benzydamine, triclosan, or zinc to improve their cariostatic effect (Kocak et al., 2009). CHX varnishes for long-term use have been introduced (Ogaard et al., 2001) but are not recommended because of the metallic taste and frequent discoloration it causes to the teeth and tongue.
An in-office application of a high concentration of fluoride in the form of a varnish or sealant may be beneficial in noncompliant patients. This exposure to fluoride is limited to office-only application, because of the temporary discoloration of the teeth and the gingival tissues, and, at the same time, increasing expense to the patient and/or chair-time to the clinician (Bishara and Ostby, 2008). With topical fluoride application, a calcium-fluoride like material (CaF2) builds up in plaque, on the tooth surface (enamel/dentin), or in incipient carious lesions, which acts as a reservoir for fluoride release when the pH is lowered (Ogaard, 1990). Vivaldi-Rodrigues et al. (2006) found that the application of the fluoride varnish resulted in a 44.3% reduction in enamel demineralization in orthodontic patients. The Cochrane systematic reviews have not been able to reach a consensus on any topical preparation or schedule that would provide the greatest benefit for preventing enamel demineralization (Benson et al., 2004; Derks et al., 2004; Chadwick et al., 2005). In fact, Benson and co-workers recommended daily fluoride mouth rinsing (0.05% NaF) similar to Zachrisson more than 30 years ago (Benson et al., 2004).
Glass ionomer cements (GICs) and resin-modified glass ionomer (RMGI) cements were introduced as orthodontic bonding adhesives to take advantage of some of their sustained fluoride release capabilities (Swift, 1989; McCourt et al., 1990) but their bond strength was found to be equivocal while the concentration of fluoride released decreased with time (Miguel et al., 1995; Miller et al., 1996; Bishara et al., 2007). Nowadays, bioactive adhesive systems with antibacterial effects or intensive remineralization ability are considered to be beneficial. Recently, a fluoride-releasing antibacterial adhesive system has been developed that combines the physical advantages of dental adhesive technology with antibacterial effects. MDPB (12-methacryloyloxydodecyl-pyridinium bromide) is potentially applicable with various restorative materials since it allows immobilization of the antibacterial component by polymerization, halts the deterioration in the mechanical properties of cured resins, and improves inhibitory effects against bacterial growth on their surfaces (Imazato, 2009). The use of argon laser for curing composite resins used for orthodontic attachments has been tried as it saves time and alters the enamel structure, rendering it less susceptible to demineralization. Combining laser irradiation with fluoride treatment can have a synergistic effect on acid resistance, thus preventing formation of WSLs (Hicks et al., 1995).
Interactive Collaboration During Orthodontic Treatment
Orthodontic treatment will succeed when its advantages outweigh any adverse sequelae. To prevent, minimize, and manage iatrogenic effects of orthodontic mechanics, the clinician should examine both the hard and soft oral tissues that may be affected by the orthodontic treatment (Shaw et al., 1991).
Cariogenic Challenge
WSL development is a very rapid process and may be apparent within 4 weeks after orthodontic bond-up appointment (Ogaard et al., 1988). Excess of bonding material around the attachment base may exacerbate the problem by creating retentive areas where the acidogenic bacteria can adhere and cause demineralization. Complicated appliance designs with loops, auxiliary archwires, springs, coils, and some Class II correctors create non-cleanable areas even in highly motivated patients. In most cases, the lesions are small and restricted to forming narrow white bands around the bracket bases or in the areas between the brackets and the gingival margin (Ogaard, 2008). The demineralized enamel is porous and absorbs stain from daily diet, representing esthetic challenges on the labial surfaces of the affected tooth. In some patients, who are noncompliant with oral hygiene and fluoride regimens, lesion development may be extensive and require premature debonding.
Tooth-conserving and time-saving adhesive methods of retaining orthodontic attachments are replacing traditional methods and procedures. However, despite these advances, caries risk under and in the vicinity of the multibonded appliances is of concern (Ogaard, 1989). Microleakage, an important post-restorative complication, is defined as the seeping and leaking of fluids and bacteria in the tooth–restoration interface (Gladwin and Bagby, 2004). The concept of microleakage has been underestimated by the orthodontists. Formation of WSL at and under the adhesive–enamel interface is often due to microleakage that may be of clinical importance (Arhun et al., 2006b; Arıkan et al., 2006). Expansion and contraction occur when the teeth are subjected to temperature changes by the ingestion of hot or cold foods. The linear thermal coefficients of expansion of enamel and ceramic or metal brackets and the adhesive systems do not match closely. Metal brackets repeatedly contract and expand more than ceramic brackets, enamel, or the adhesive systems, producing microgaps between the bracket and the adhesive system, resulting in leakage of oral fluids and bacteria beneath the brackets. However, if microleakage cannot be prevented, inactivation of bacteria will be a direct strategy to prevent development of WSLs. Antimicrobial adhesive systems may be beneficial in such situations, ensuring antimicrobial effect at the site of therapeutic importance, which is the enamel surface under the bracket in this circumstance (Arhun et al., 2006b).
Pulpal Reactions to Orthodontic Forces
The dental pulp is a specialized type of loose connective tissue, rich in cells such as odontoblasts, fibroblasts, and cells of the immune, nervous, and vascular systems (Leone et al., 2009). While performing complex functions such as having a nervous and vascular supply for vitality, carrying sensory impulses and formation of protective secondary dentin, it is responsive to peripheral impacts, such as orthodontic forces. Morphological and structural changes occur in dental pulps subjected to such forces (Anstendig and Kronman, 1972; Delivanis and Gauer, 1980; Popp et al., 1992; Kayhan et al., 2000). Although reports on these changes present conflicting data, most show degenerative changes that may have harmful effects on tooth vitality.
Circulatory disturbances, vascular compression, and formation of secondary dentin after orthodontic force application have been reported (Stenvik and Mjör, 1970; Anstendig and Kronman, 1972). Radiorespirometric techniques, which measure the tissue respiration rate, indicated depression of the oxygen utilization system within the pulp cells after the application of orthodontic forces (Hamersky et al., 1980; Unsterseher et al., 1987). An average of 27% reduction in pulpal respiration has been seen after 3 days of orthodontic force application (Unsterseher et al., 1987) and this might compromise the long-term vitality of the tooth (Popp et al., 1992). Hypoxia in pulp cells due to reduced blood flow may negatively enhance mitochondrial function and proliferative activity (Amemiya et al., 2003). Significant elevation of aspartate aminotransferase (AST) activity, an enzyme that is released into the extracellular environment following cell death, has been demonstrated after 1 week of intrusive force application (Veberiene et al., 2009). Likewise, Perinetti et al. (2004) observed elevated AST activity in orthodontically treated teeth and found these levels comparable to reversible pulpitis. It has been hypothesized that increased AST levels could be the result of circular disruption, reduction in oxygen levels, and pulp tissue apoptosis. Furthermore, an increased response to electrical pulp testing was seen, which is positively correlated to anatomical features such as pulpal weight and root surface area (Veberiene et al., 2009).
Several authors have detected formation of calcified deposits in the dental pulps of teeth undergoing orthodontic treatment (Stenvik and Mjör, 1970; Delivanis and Gauer, 1980; Popp et al., 1992). However, Stenvik and Mjör (1970) concluded that these changes were not different from those in untreated teeth. Loss of tooth vitality during orthodontic treatment has also been reported, especially in previously traumatized teeth. Histologically, cell death can be seen as either cellular necrosis and/or apoptosis. Even though previous studies named the changes in teeth undergoing orthodontic treatment as necrosis, the term apoptosis is more suitable for nontraumatized teeth. Rana et al. (2001) investigated apoptotic changes with orthodontic mechanics in detail and could observe maximum rate after 3 days of force application.
Several other factors are also involved in pulpal reactions to orthodontic force, the main one being the type of tooth movement. Intrusion, the movement that has the greatest impact on the root apex, is capable of occluding the pulpal blood supply (Vandevska-Radunovic et al., 1994; Sano et al., 2002). Moreover, Kvinnsland et al. (1989) and Nixon et al. (1993) reported a substantial increase in pulpal blood flow and in the number of capillaries after application of extrusive orthodontic forces. Mostafa et al. (1991) observed vacuolization and severe odontoblastic degeneration in dental pulps undergoing orthodontic extrusion for 7 days. McDonald and Pitt Ford (1994) found decreased human blood flow after continuous light tipping forces, using laser Doppler flowmetry. Since orthodontic treatment involves complex three-dimensional tooth movements, it is not always possible to avoid movements that are relatively more detrimental.
Since the first rule of orthodontic mechanics is to avoid poorly controlled and jiggling forces (Krishnan and Davidovitch, 2009), the magnitude of the applied force is another important factor. Controlled intraoral orthodontic mechanics do not require heavy forces for tooth movement, but orthopedic treatment requiring forces over 500 g may have deleterious effects on the dental pulp. In a histological study, Küçükkele and Okar (1994) reported degeneration of vessel walls in teeth undergoing rapid palatal expansion treatment. However, contrary to the results of previous studies, a histomorphometric evaluation by Kayhan et al. (2000) has shown no pulpal differences between control teeth and teeth undergoing RPE.
and Okar (1994) reported degeneration of vessel walls in teeth undergoing rapid palatal expansion treatment. However, contrary to the results of previous studies, a histomorphometric evaluation by Kayhan et al. (2000) has shown no pulpal differences between control teeth and teeth undergoing RPE.
The degree of pulpal reaction to orthodontic forces also depends on individual factors such as the age of the patient and the size of the apical foramen (Butcher and Taylor, 1951; Stenvik and Mjör, 1970). Hamersky et al. (1980) reported positive correlations between age and the rate of tissue respiratory depression. Therefore, the maturity of a tooth is an important aspect in preserving tooth vitality during orthodontic treatment and clinicians should be cautious while moving teeth with closed apices.
As pulpal tissue is susceptible to thermal stress, temperature generating orthodontic procedures such as stripping, thermal debonding, and residual adhesive removal after debonding requires extra attention. The heat generated during rotary instrumentation may result in irreversible trauma to the pulp. Among the different modalities used for instrumentation, such as handheld stripper, rotary disks and air-rotor stripping that utilizes diamond burs, the handheld stripper, which does not need any rotary instrument, has been found to be the safest method (Baysal et al., 2007). Thermal debonding using carbon dioxide laser (Ma et al., 1997) is considered safest for debonding orthodontic brackets. Clean-up of residual resin using high-speed handpieces may cause vascular injuries and pulp necrosis. Zach and Cohen (1965) stated that a temperature rise of more than 5.5°C will result in pulpal inflammation and an increase of 11°C resulted in necrosis. Uysal et al. (2005) reported that clean-up of residual resin should be performed with adequate water-cooling to avoid temperature changes exceeding the critical value. Eminkahyagil et al. (2006) concluded that tungsten carbide burs used at low speed may be the method of choice for adhesive clean-up.
Technological advancements in laser dentistry may be useful in the future for avoiding severe pulpal reactions. In a recent study performed on rats, it has been shown that the use of low level laser therapy (LLLT) during tooth movement results in increase in vascularization and faster repair of pulpal tissue. The therapeutic effects of LLLT, such as pain relief, acceleration of tissue healing, repair and neovascularization, increased fibroblast and collagen fiber proliferation, and decrease in the immune response, may provide an insight for optimization of orthodontic treatment (Abi-Ramia et al., 2010).
Despite all these efforts to minimize adverse pulp reactions, it seems almost impossible to avoid hyperemia or reversible pulpitis during the early stages of orthodontic tooth movement. As shown by Popp et al. (1992), the signs of hyperemia diminish as blood flow returns to normal in 72 hours. These mild pulpitis reactions can be detected 2 hours after bonding/banding. Moderate pain caused by pulp hyperemia can last up to at least 7 days (Polat and Karaman, 2005). Mild pain can be noted after each appointment due to the change in archwires, but pulp vitality is unaffected in most of these cases.
Differential diagnosis between symptoms of tooth movement and an inflamed tooth is very difficult, especially if there is a history of a trauma. A patient with severe pain or pain that lasts for more than 10 days or who has darkening of the crown should consult a restorative specialist, preferably an endodontist. Radiographic evidence of an apical radiolucency may necessitate endodontic therapy (Hamilton and Gutmann, 1999), although orthodontic movement can be continued afterward.
Orthodontically Induced Root Resorption
Both external and internal root resorption are challenging for the clinician since the exact nature of irreversible loss of tooth substance is not known and treatment of aggressive forms is difficult. Several predisposing factors have been suggested and the application of faulty mechanics has been proposed as the main cause of iatrogenic external root resorption. This section provides an overview of two types of external root resorption: external apical root resorption and invasive cervical root resorption.
Alveolar bone resorption is the basis of orthodontic tooth movement. Bone resorption occurs in a usual healthy periodontal environment, while the highly mineralized cementum is more resistant to the resorption process, because of its fluoride content and vascular nature. Moreover, the cemental surface is covered by a pre-cemental layer that is resistant to resorption (Reitan, 1974). The inflammatory process, incident and essential for tooth movement, is also a reason for orthodontically induced root resorption. Orthodontically induced inflammatory root resorption (OIRR) frequently determines the success of orthodontic treatment (Mohandesan et al., 2007). If the duration of orthodontic treatment or the magnitude of the force is increased, the risk of root resorption increases and results in exposure of the dentin layer under the resorbing cementum, which heightens the osteoclastic attack and leads to progressive root resorption until all orthodontic forces are stopped. When the forces are relieved, repair commences from the periphery with fibroblast and cementoblast-like cells synthesizing collagenous fibrillar material and a new periodontal ligament (PDL). Most of the resorbed lacunae are frequently repaired with secondary cementum (Reitan, 1985). According to Owman-Moll and Kurol (1998), 6–7 weeks after the termination of force, the amount of repair rises to 82%.
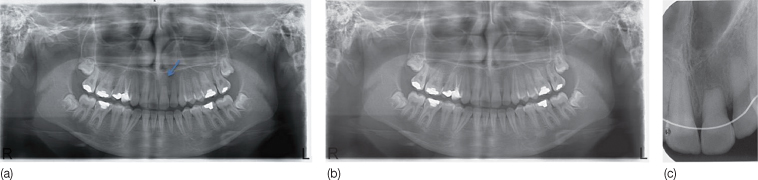
Root resorption caused by orthodontic therapy occurs in two locations: superficial surface resorption or in the apical third of the root (Figure 16.1). The increased incidence can be explained in two ways (Huang et al., 2005).
- First, the fulcrum of the tooth is more coronal to the apical third of the root and due to the differences in the direction of the PDL fibers, forces are more traumatic to the apical region than to the coronal.
- Second, the middle and gingival thirds of the root are covered with acellular cementum, whereas the apical third is covered with cellular cementum, containing cells and blood vessels that have been damaged by heavy forces (Rygh, 1977).
Figure 16.1 Orthodontically induced apical root resorption in the apical third of the root. (a) At the end of fixed appliance treatment. (b) At 1-year follow up. (c) Periapical radiograph at 14-month follow-up. Resorption has not progressed: however the tooth has been splinted with a flexible wire retainer due to slight mobility.
Predisposing factors for root resorption can be divided into biological factors and factors related to orthodontic mechanics. Among the biological factors, chronological age, dental age, gender, tooth structure, root morphology, presence of previous resorption, trauma and endodontic therapy, autotransplantation, alveolar bone density, malocclusion type, periodontal disease, occlusal forces, habits, absence of teeth, impacted canines, and systemic conditions, have been listed. Treatment and appliance type, amount of tooth displacement, type of tooth movement, duration, degree and amount of orthodontic force, intermaxillary elastic usage and application of orthopedic forces are among the mechanical factors related to root resorption. However, a major factor for the occurrence of root resorption is individual susceptibility (Rygh, 1977). The susceptibility to root resorption differs among individuals, as well as within the same individual at different periods of time. Hormones, body type and the metabolic rate trigger signals that initiate fluctuations in osteoclastic and osteoblastic activities. In certain systemic diseases such as allergy and asthma there is increased susceptibility to resorption (Davidovitch, 1996; McNab et al., 1999; Davidovitch et al., 2000). The maxillary and mandibular incisors, maxillary first molars, maxillary first and second premolars, and the maxillary canines are the teeth that are more prone to root resorption. One reason for the high prevalence of root resorption among incisors may be their thin root morphology, but it is more likely due to the excessive movement during orthodontic treatment, that is, round tripping, and contact with the cortical plates of alveolar bone, particularly during the use of intra-slot torque, which generates very heavy forces (De Angelis and Davidovitch, 2009).
The presence of root resorption can be established using conventional radiographic methods such as periapical radiography, orthopantomograms, or lateral cephalograms. However, these routinely used methods are not helpful in the detection of lateral and early lesions, since resorption cannot be radiographically seen before some amount of apical root shortening occurs (Brezniak and Wasserstein, 2002). The periapical method seems to be the best conventional method, with minimal distortion and superimposition of anatomic structures. Computed tomography (CT), either computed medical or dental cone beam, is far superior to conventional dental radiography for locating early resorptive areas (Ericson and Kurol, 2000). However, the routine clinical use of CT is limited by its high radiation dose and expense (Sameshima and Asgarifar, 2001). Cone-beam dental CT offers lower radiation dose, fewer artifacts, and faster image projection than a conventional CT (Dudic et al., 2009).
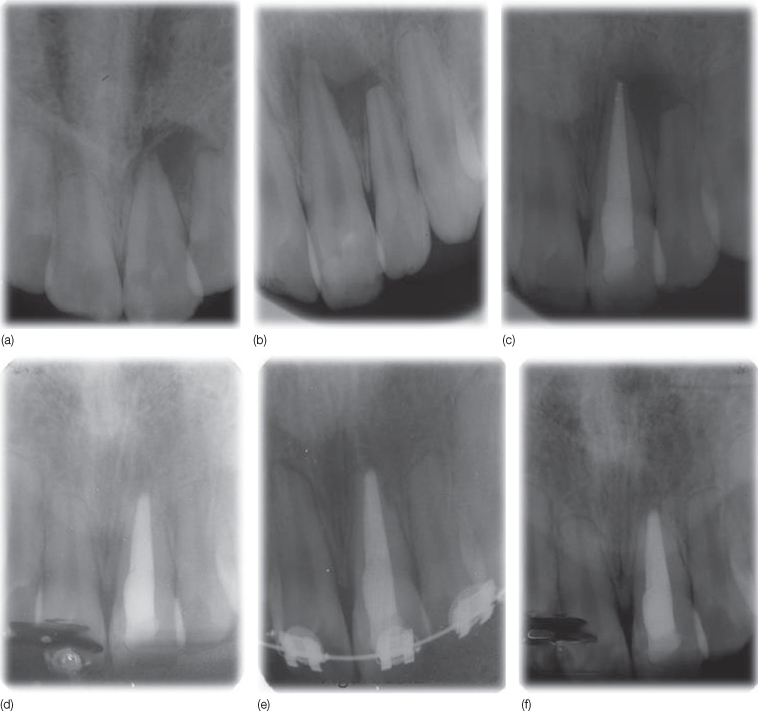
Resorption is observed in teeth subjected to faulty mechanics in the early stages of treatment, such as in uncontrolled tipping of maxillary incisors in order to reduce excessive overjet (De Angelis and Davidovitch, 2009). Root resorption can be diagnosed with the help of dentinal proteins such as dentin matrix protein 1 and dentin phosphophoryn, which are released into the gingival crevicular fluid during active root resorption (Mah and Prasad, 2004). If there was pretreatment root resorption, the rate might increase from 4% to 77% during treatment (Goldson and Henrikson, 1975). Previously traumatized teeth present an important risk for OIRR (Linge and Linge, 1991), but Malmgren et al. (1982) concluded that resorption rates do not increase in the presence of trauma if a normal PDL environment is maintained (as a result of applying appropriate mechanics). Although Wickwire et al. (1974) found a greater incidence of resorption during orthodontic treatment in 53 endodontically treated teeth, Spurrier et al. (1990) and Remington et al. (1989) found lower resorption rates in such teeth due to their increased dentin hardness and density after the orthodontic treatment (Figure 16.2).
Figure 16.2 Root resorption due to orthodontic treatment. (a,b) The talon cusp of the left central incisor was ground down during orthodontic treatment. Note that only this tooth did not demonstrate apical resorption, as it was nonvital due to pulp/dentin exposure, which was not diagnosed during the grinding procedure. (c,d) Treatment of chronic apical periodontitis with root canal treatment and apical resection. (e) Patient was re-treated orthodontically. (f) After the second orthodontic treatment, the left central incisor showed no resorption and was also asymptomatic without any mobility.
Treatment plans for patients with predisposing factors should ensure that teeth will not be moved unnecessarily and into contact with cortical plates of alveolar bone, in order to avoid any additional resorption. During treatment, evaluation should be done 6 months after the onset of treatment (Levander and Malmgren, 1988). If any sign of resorption is seen in the radiographs (which implies that faulty mechanics had been used), the application of orthodontic force can be interrupted for 2–4 months to allow for repair (Reitan, 1964; Levander and Malmgren, 1988), but more importantly, the appliances should be adjusted to deliver the appropriate mechanical forces. Severe resorption should never occur when biomechanical principles are followed correctly, with close attention to the unique anatomical features of each patient. Iatrogenic root resorption usually does not progress once orthodontic force is discontinued.
A tooth with severe resorption and increased mobility can be splinted to the neighboring teeth. The patient should be informed about the situation and advised to be careful during the use of these teeth. Root canal treatment is usually not needed but can be performed if excessive loss of root length has occurred (Malmgren and Levander, 2004). In rare cases, resorption continues despite termination of orthodontic treatment and does not stop until splinting and endodontic therapy is performed (Gholston and Mattison, 1983). For severe, active lesions, endodontic treatment should be performed with a calcium hydroxide paste, but if the resorption has ceased, the canal can be filled with gutta-percha. During the retention period, the clinician should prevent occlusal trauma to the resorbed teeth through modification in the retainers (Dougherty, 1968). A crown/root ratio of 1:1 is sufficient for maintaining the tooth. If the root length is shorter than this, the tooth is likely to be unable to bear the functional loads of mastication. Although vitality is rarely affected, endodontic treatment should be performed if the crown/root ratio is less than 1:1. A search for pharmacological agents capable of repairing root resorption revealed that bisphosphonates (Liu et al., 2004), echistatin (Talic et al., 2006) and low doses of corticosteroids (Ashcraft et al., 1992) (1 mg/kg) have positive effects, whereas high doses (15 mg/kg) have a reverse effect.
Invasive cervical resorption is an aggressive type of external root resorption that leads to progressive destruction of tooth structure. It usually affects single teeth, but in rare cases multiple teeth are affected (Coyle et al., 2006). Cervical location is the characteristic feature, and resorption of coronal dentin and enamel creates a pinkish color as the vascular tissues become visible (Heithersay, 2004) (Figure 16.3). The lesions are characterized by highly vascular fibrous tissue with osteoclasts arising from the PDL (Smidt et al., 2007). Since microorganisms are rarely found, microbial involvement in these lesions is doubtful (Heithersay, 1999; Trope, 2002). A study of 222 patients who displayed invasive cervical resorption showed that orthodontic treatment, trauma, intracoronal bleaching, and surgery involving the cementoenamel junction were the major predisposing factors. In that study, 21.2% of patients were reported to have a history of orthodontic treatment. Again, this type of root resorption implies that inappropriate mechanics had been applied in these patients.
Figure 16.3 (a,b) Invasive cervical resorption after orthodontic treatment, demonstrating a pinkish color. (c) Patient was referred to an experienced endodontic specialist for treatment of invasive cervical resorption by elimination of the actively resorbing tissue and restoration of the defect with a suitable filling material (mineral trioxide aggregate [MTA]). However, conventional root canal treatment was carried out by a general practitioner and the prognosis remained poor.
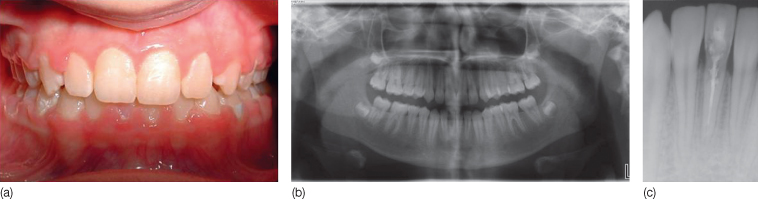
Invasive cervical resorption is painless and rarely symptomatic. The resorption process starts below the gingival margin and extends apically and coronally along the root dentin (Smidt et al., 2007). The lesion is often separated from the pulp by the predentin layer, which is the last to resorb (Heithersay, 2004). A clinical feature is a pink coronal discoloration close to the gingival margin. It can go unnoticed for months to years and only become evident on routine radiography. Conventional radiographs taken from different angles can identify the involved surfaces but a three-dimensional visualization of the exact size and location of the lesion requires a CT scan (Kim et al., 2003; Gulsahi et al., 2007). Two important features of invasive cervical resorption differentiate it from internal root resorption. One is the absence of pulpal signs and the other is the radiographic appearance of the pulp canal size (Gulabivala and Searson, 1995; Smidt et al., 2007). In invasive cervical resorption the canal space is unchanged and the radiolucency extends coronally and apically in the dentin.
Invasive cervical resorption is quite aggressive, therefore the orthodontist should refer the patient as soon as the lesion is diagnosed. The treatment should be performed by experienced specialists to prevent tooth loss. The rationale for treatment of invasive cervical resorption is the elimination of the actively resorbing tissue and restoration of the defect with a suitable filling material (Figure 16.4). Both nonsurgical and surgical treatment approaches can be used. Nonsurgical regimens involve topical application of a 90% aqueous solution of trichloroacetic acid for the induction of coagulation necrosis to the lesion area, curettage, endodontic treatment if pulpal perforation is present, and glass ionomer cement restoration. The use of calcium hydroxide for neutralization of the lesion, elimination of microorganisms and inactivation of toxic products is also recommended (Frank, 1981). If the margin of the lesion is below the cervical line, orthodontic extrusion can be performed. Extrusive orthodontic forces can be applied for 4–6 weeks and during the extrusion, crown shortening can be performed if premature contact occurs. Fiberotomy can be performed for the maintenance of the extruded tooth (Smidt et al., 2007). However, the clinician should keep in mind the possibility of ankylosis, which is not seen in cases of cervical resorption (Figure 16.5).
Figure 16.4 Diagnosis and treatment of invasive cervical resorption. (a) Note the extensive irregular radiolucency in the left mandibular second premolar in the panoramic radiograph. (b) The periapical radiograph of the left mandibular second premolar tooth shows an irregular radiolucent area in the tooth crown (arrow). (c) Axial computed tomography (CT) scans taken from coronal to apical and obtained with a bone window setting showing extensive resorption in the mesial cervical area of the left mandibular second premolar. (d) Intraoral appearance of the resorption area. (e) Intraoral appearance after the root canal treatment and restoration of the resorbed area. (f) Periapical radiograph at 6-month follow-up.
(From Gulsahi A, Gulsahi K, Ungor M (2007) Invasive cervical resorption: clinical and radiological diagnosis and treatment of 3 cases. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics 103(3): e65–72.)
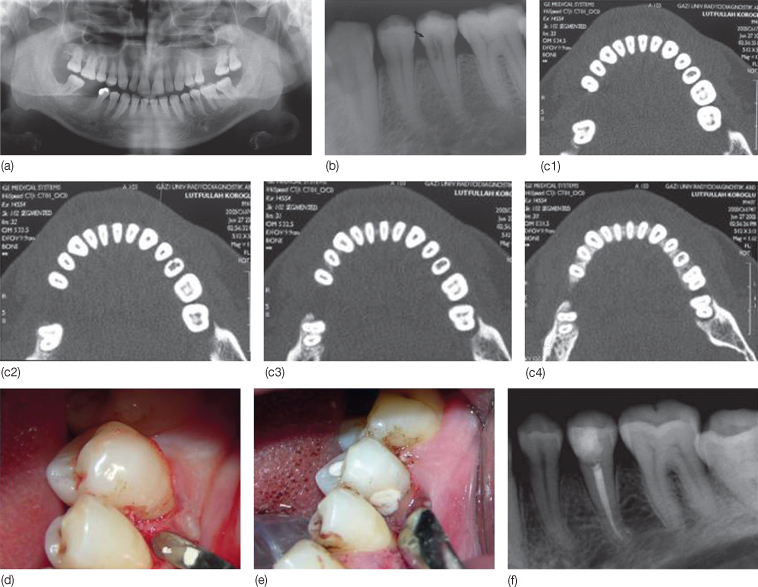
Figure 16.5 Ankylosis can occur in cases of invasive cervical resorption. (a,b) Patient referred to the orthodontic clinic for treatment of cervical resorption via orthodontic extrusion after periodontal curettage. (c) Orthodontic force was applied after occlusal grinding. (d) No movement occurred following 3 months of force application as the tooth was ankylosed, it was then extracted.

Surgical treatment involves periodontal flap surgery, curettage, and restoration of the defect. Restorative materials that have been used previously include amalgam, composite resin, and glass ionomer cement (Lustmann and Ehrlich, 1974; Frank, 1981; Frank and Blakland, 1987). Currently, mineral trioxide aggregate (MTA) is recommended to restore the resorptive cementum in cervical resorption cases (Frank and Torabinejad, 1998; White and Bryant, 2002; Yilmaz et al., 2010). Baek et al. (2005) have shown that the type of cementum coverage achieved using MTA had not been achieved with any other material. White and Bryant (2002) reported an increase in radiodense crestal bone when MTA was used with guided tissue regeneration to fill an external root resorption site with a bone defect. A platelet-enriched fibrin sealant (Tisseel) has been in use for a long time for sinus floor augmentation, treatment of peri-implantitis, intrabony periodontal defects, and alveolar ridge reconstruction. Ren et al. (2000) have demonstrated that Tisseel enhances the healing of exposed pulp tissue in dogs. Though dentinal bridge formation was not present in a majority of cases, the authors concluded that fibrin sealant was a promising material as a bioactive pulp capping agent.
Emergency Orthodontic Treatment in Trauma Cases
There are instances where other dental disciplines may require orthodontic collaboration such as in trauma patients referred from emergency clinics. Trauma to the orofacial region occurs frequently and comprises 5% of all injuries that require treatment (Glendor et al., 2007). Dental injuries, which are the most common among all facial injuries, are experienced by more than 20% of children, mostly between the ages of 8 and 12 (Glendor et al., 2007; Moule and Moule, 2009). Boys sustain dental injuries about twice as often as girls do. Most dental injuries involving the maxillary incisors occur in cases of Class II Division 1 malocclusion with increased overjet and inadequate lip closure (Forsberg and Tedestam, 1993; Burden, 1995). Emergency management of traumatized teeth is usually performed by a pediatric dentist, or an endodontic/conservative dentistry specialist, but an interactive approach involving the orthodontist in the trauma management team is advised. Orthodontic treatment planning for patients with previously traumatized teeth often requires decisions regarding the long-term viability of the traumatized teeth and effects of trauma on the developing dentoalveolar complex.
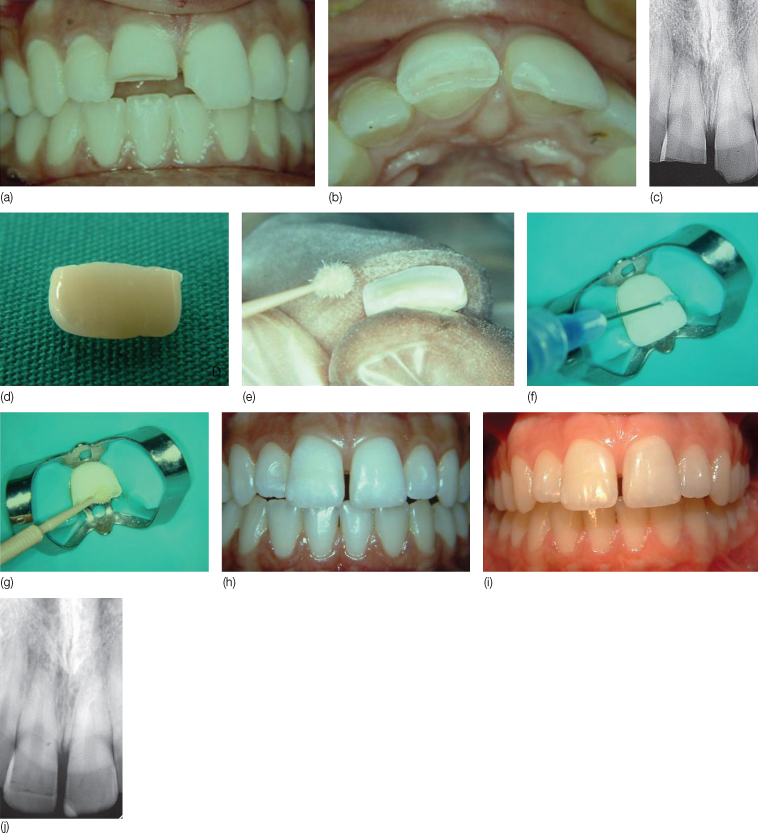
Treatment of an uncomplicated crown fracture can be accomplished quite successfully by either a build-up with acid-etch composite resin, or by reattaching the fractured segment, if available, using an adhesive bonding system (Figure 16.6). The expected outcome for either approach is excellent with nearly 100% pulp survival regardless of root developmental status (Robertson et al., 2000). The appropriate time for evaluating the vitality of the tooth is 8 weeks after the trauma.
Figure 16.6 Step-by-step progression of reattachment of the fractured segment of a central incisor using an adhesive bonding system. (a–c) Intraoral and radiographic views before treatment. (d) Broken fragment of tooth. (e–g) Re-attachment procedure. (h) After re-attachment and polishing. (i,j) 1-year follow-up. The tooth was vital.
(From Arhun N, Ungor M [2007] Re-attachment of a fractured tooth: a case report. Dental Traumatology 23(5): 322–6. Courtesy of John Wiley and Sons.)
A fracture involving dentin exposes dentinal tubules in direct communication with the pulp. Therefore, timely protection of the exposed dentin is advisable to prevent the pulp from undergoing infection-related necrosis. Complicated fractures of the primary teeth require decisions based on life expectancy of the primary tooth and vitality of the pulpal tissue (Flores, 2002). If the fracture occurs in an adult with fully formed roots it will be more practical to perform root canal treatment prior to the prosthetic restoration and/or orthodontic treatment. On the other hand, it is very important to make every effort to preserve pulp vitality in young patients with developing permanent teeth as continued pulp vitality facilitates root development (Fuks et al., 1987). The exposed pulp will develop granulation tissue to protect the exposed wound and bacteria will invade the pulp tissue gradually. However, it may take many days for bacteria to penetrate even a few millimeters so the pulp can be preserved even if it has been exposed for more than 24–48 hours (Heide, 1991). Therefore, complicated fractures should not be viewed as hopeless situations for pulp survival in young patients. Miomir Cvek (1978) introduced a procedure known as the Cvek pulpotomy technique, which employs calcium hydroxide for pulp capping. This vital pulpotomy technique should be performed as soon as possible after the trauma. As long as the pulp is alive and is properly protected, continued root development can be expected.
If pulpal necrosis accompanies the fracture, the general treatment protocol involves root canal treatment followed by protective permanent restorations. The open and sometimes divergent apical morphology and weak root dentinal walls make e/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


