16
3D Image-Aided Diagnosis and Treatment of Impacted and Transposed Teeth
Introduction
Because impacted and transposed teeth often are difficult to diagnose accurately or treat predictably, they remain some of the most challenging cases in orthodontics. Some hurdles or limitations in treating these cases include existing and/or treatment-related root resorption, extended treatment time, failure to retrieve the tooth, and ankylosis. Part of the complexity in treating these cases is related to the inability of the clinician to accurately visualize the location, angulation, spatial position, and relationships of the tooth in three dimensions using conventional two-dimensional (2D) radiographs. Furthermore, even with the availability of three-dimensional (3D) cone beam computed tomography (CBCT), there currently remains a gap in knowledge and abilities of clinicians on how best to extract and utilize all the information available in the 3D dataset for precision diagnosis and how to use this evidence to plan and execute treatment and biomechanics strategies optimally. To achieve these capabilities, it is important for clinicians to acquire the skill set needed to utilize imaging software and to manipulate and interpret 3D images. It is expected that with ongoing improvements in 3D imaging and software, and increasing hands-on experience of clinicians in using this new technology, this hurdle also will be overcome. This chapter provides important insights toward achieving this goal.
Since its introduction into dentistry in 1999, CBCT increasingly has become a valuable aid in diagnosis and treatment planning in orthodontics (Kapila et al., 2011). However, despite substantial research discoveries with CBCT, many of which are highlighted in this book, the profession is still in the early phases of developing approaches and protocols that help us to utilize the information contained in 3D volumes optimally to enhance diagnosis or treatment planning of cases, optimize biomechanics, and ultimately improve the treatment outcomes for our patients. Of the many clinical situations presenting to the orthodontist, the one with the strongest research evidence justifying the use of CBCT is impacted teeth. While there currently is considerable information available on the application of CBCT to impacted teeth, a cohesive and comprehensive approach to applying information derived from CBCT and optimal protocols for its utilization in these cases have not been established.
In this chapter, we provide insights into evidence-based use of CBCT for treating impacted and transposed teeth and how best to utilize the information thus derived for predictable and efficient treatment of these teeth. Specifically, we provide the foundational background on impacted and transposed teeth and extend this to contemporary insights gained by imaging these teeth with CBCT. We then discuss protocols for CBCT imaging, interpretation, and treatment planning for impacted and transposed teeth. Finally, we use cases to demonstrate the potential pitfalls of suboptimal diagnosis and treatments resulting partially from the limitations of 2D radiographs and to demonstrate approaches for individualized 3D image-based biomechanics for efficient and predictable treatment of impacted and transposed teeth while minimizing damage to neighboring roots or periodontium.
Prevalence and Etiology of Impacted and Transposed Teeth
Maxillary canines are the second most commonly impacted teeth after third molar impactions (Bedoya & Park, 2009; Manne et al., 2012, and references therein). Approximately 1–3% of the population has an impacted maxillary canine, which occurs twice as frequently in females than in males. The majority of maxillary impacted canines are unilateral (90–92%), and palatally (85%) rather than buccally (15%) displaced (Peck et al., 1994; Quirynen et al., 2000). Mandibular canine impactions are rare, with an incidence of 0.35% (Dachi & Howell, 1961).
Transposition is defined as the partial or complete positional exchange of adjacent teeth (Shapira & Kuftinec, 2001). Less commonly, a tooth can erupt in the position of a nonadjacent tooth (Peck et al., 1993; Peck & Peck, 1995). Transpositions are more rare than maxillary canine impactions, occurring in less than 1% of the population (Peck et al., 1993; Peck & Peck, 1995). When present, transpositions are most likely to occur in the maxilla and most often involve the canine (Plunkett et al., 1998; Shapira & Kuftinec, 2001; Ely et al., 2006). In the maxilla, the canine is transposed most commonly with the first premolar followed by the lateral incisor (Joshi & Bhatt, 1971; Shapira, 1980; Gholston & Williams, 1984; Peck & Peck, 1995; Wasserstein et al., 1997). Interestingly, all reported cases of mandibular transpositions involve the canine and lateral incisor (Peck et al., 1998). As with impactions, females are more likely to have transposed teeth, and the majority of these will be unilateral and left-sided (Shapira, 1980; Peck & Peck, 1995). Not surprisingly, transpositions also are more common in cleft lip and palate (CL/P) patients than in non-cleft patients (Oberoi et al., 2010).
Because both impactions and transpositions represent ectopic eruption, it commonly is accepted that their etiologies are multifactorial, involving local, systemic, and genetic factors (Peck et al., 1993, 1998, 2002; Frazier-Bowers et al., 2010). Supporting this concept are the growing number of studies showing the concomitant presence of dental anomalies, especially peg lateral incisors and/or dental agenesis, especially second premolars, with canine impactions (Peck et al., 1996a, 1996b; Peck & Peck, 1997; Peck, 1998; Shalish et al., 2002; Leonardi et al., 2003; Garib et al., 2009). Genome-wide association studies have yet to be performed specifically on patients with impactions or transpositions, but it is likely that this approach will yield significant information on the genes responsible for normal or abnormal developmental positioning of teeth. This could help clinicians diagnose and treat impactions early, which is important for improving outcomes for these patients (Manne et al., 2012).
While current research on tooth eruption relies heavily on understanding the molecular regulation of eruption, conventional 2D radiographs, especially periapical and panoramic radiographs, have allowed us to identify several local factors that may contribute to ectopic or impacted canines. These factors include enlarged crown, retained primary canines, ankylosis, cysts, neoplasms, root dilacerations, and missing or peg lateral incisor (Manne et al., 2012). Identifying the presence of these local factors is important for accurate diagnosis and treatment planning for impactions and transpositions. As noted below, 3D radiography has broadened our understanding of normal and ectopic tooth development and eruption that likely will contribute to further refinements in diagnostics and treatment approaches. Furthermore, the knowledge gained through these studies will be critical for focusing future research efforts on the pathophysiological mediators of impactions and transpositions.
2D and 3D Radiographic Findings on Normal Canine Development and Eruption
Since the maxillary canine is the most commonly impacted tooth, it has received the majority of attention from researchers interested in the process of dental impactions. For this reason, the following section focuses on studies, particularly those using 2D and 3D radiographs, that have broadened our understanding of normal canine development and eruption.
While conventional 2D radiographs have given us important data on normal tooth development, their accuracy for assessing tooth position falls significantly below the accuracy of 3D radiographs (see also Chapter 15). Knowing this, a critical reader of the scientific literature on radiographic mapping of maxillary canine development and eruption rightly would be wary of existing literature because it is based overwhelmingly on conventional 2D radiographs. Moreover, as Broadbent (1941) advised early on, researchers and clinicians must recognize the technical limitations of 2D radiographs to describe a 3D process. He suggested that useful information on canine development and eruption can be gleaned only from both a lateral and posterior-anterior cephalograph of the subject, which then was the best available approach to “representing” a structure in 3D. Investigations using this approach to assess 3D canine position have shown that, on average, the maxillary canines move incisally 18.6 mm in children between ages 5 and 13, distally 11.5 mm from ages 7 to 13 years, and palatally until about 2 years prior to eruption, at which point the canines reverse direction, eventually moving 2.7 mm buccal to their starting position (Coulter & Richardson, 1997). The question regarding this study is how accurate the data are given that the measurements were taken from conventional 2D radiographs, which inherently are inaccurate. It is clear that CBCT offers a much clearer and far more accurate picture than 2D radiographs of how canines develop and erupt.
To date, the only published 3D study focused on canine eruption was conducted on CL/P patients (Oberoi et al., 2010). Unlike the Coulter and Richardson study (1997), which tracked canine eruption annually between the ages of 5 and 15, the CBCT scans in this study were taken only twice, once at age 10 years 6 months and then again at age 11 years 9 months. Therefore, we do not have a complete 3D picture of maxillary canine development in these children. Nonetheless, this study traces canine movement prior to eruption on both the cleft and non-cleft sides. Both the cleft- and non-cleft-side canines move incisally, mesially, and buccally, albeit at different rates. The cleft-side canine moves incisally 0.8 mm more than the non-cleft-side canine (6.8 mm and 5.9 mm, respectively), mesially 1.6 mm more than the non-cleft-side canine (3.2 mm and 1.6 mm, respectively) and the same distance buccally as the non-cleft-side canine (2.5 mm). By comparison, strikingly smaller maxillary canine movements of 0.2 mm incisally, 0.6 mm buccally, and none in the mesio-distal axis were reported in children ages 10–11 and 11–12 using 2D lateral and posterior-anterior cephalographs (Coulter & Richardson, 1997). Thus, not only are the measurements made from 2D radiographs far smaller than those derived from CBCT, but they essentially show that the canines do not move in 10- to 12-year-old children, which, besides contradicting the 3D observations, is highly unlikely.
With the introduction of CBCT and its 3D rendering capacity, it now is becoming common practice for orthodontists to prescribe CBCT for patients with an impacted canine diagnosed clinically and/or on conventional 2D radiographs, providing a database of 2D and 3D radiographs taken on the same patient. This allows direct comparison of the diagnostic quality of each image and, more importantly, enables the assessment of how CBCT images effect a clinician’s treatment planning decisions; this will be discussed later. These 3D data also have enabled researchers to determine if impacted canines have a unique 3D positional signature relative to that of a normally erupting canine. Thus, analyses of CBCT scans from 29 consecutively treated orthodontics patients (mean age = 16.6 years) who presented with at least one impacted canine showed that the average distance of the unerupted canine cusp was 10.1 mm mesial, 1.8 mm palatal, and 10 mm vertical from the position it would occupy if positioned ideally in the arch (Oberoi & Knueppel, 2012). Whether this pattern is detectable earlier in development is not known yet, but if it is, it would be helpful for early diagnosis of impacted canines and implementation of case-specific interceptive strategies or treatment approaches.
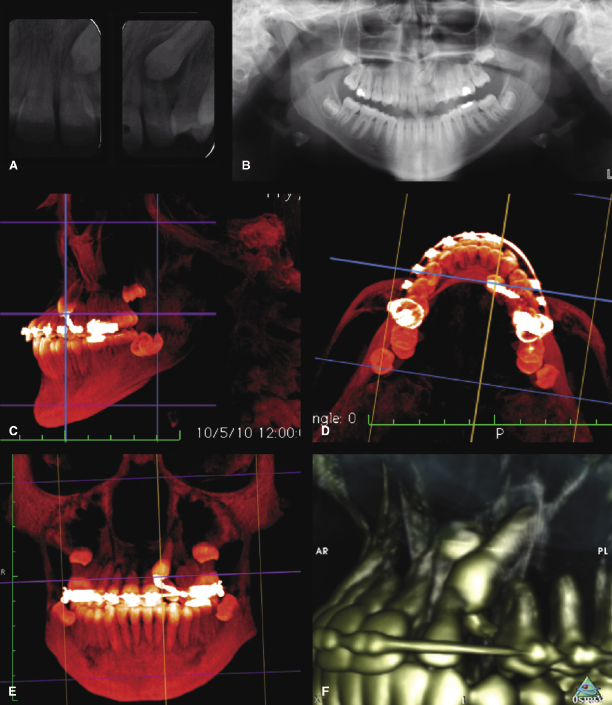
Another distinction between 2D and 3D radiography is in their capacity to detect resorption of roots of teeth that are in close proximity to impacted teeth (Alqerban et al., 2009a, 2011). Diagnosing root resorption with conventional 2D radiographs can be challenging due to superimposition of structures and the other pitfalls of 2D images (Figure 16.1). Thus, while periapical and panoramic radiographs enable the detection of root resorption in about 33–50% of the incisors associated with impacted canines, CBCT facilitates the detection of root resorption on an additional 65% of these roots than are detectable with 2D imaging (Alqerban et al., 2011; see also Chapter 15). These findings and their clinical implications are discussed below in greater depth.
Efficacy of CBCT in Diagnosis and Treatment Planning of Impacted Teeth and Associated Root Resorption
As pointed out in Chapters 1 and 6, the use of CBCT imaging ideally should be determined by evidence showing its efficacy in enhancing diagnosis and treatment decisions, and ultimately in improving treatment efficiency and outcomes. In the absence of such research-based support for using CBCT, a secondary justification for imaging is when, on the basis of clinical or other diagnostic aids, the clinician determines that the benefits of CBCT outweigh its risks. In this context, there now is substantial research evidence to support the use of CBCT imaging for diagnosing and treatment planning impacted teeth. Indeed, it is one of the few clinical situations in orthodontics that has this level of research evidence to support the use of CBCT (Haney et al., 2010; Katheria et al., 2010; Botticelli et al., 2011). The most supportive research evidence for the use of CBCT radiographs for diagnosing and treatment planning impacted canines arises from comparison studies that demonstrate differences between 2D and 3D imaging in the accuracy of localizing impacted canines, identification of canine-induced root resorption on adjacent teeth, and pinpointing the site for surgical access to the impacted canine. Importantly, some of these studies also demonstrate that CBCT images increase the clinician’s confidence in treatment planning. In the following sections, we will review the lines of research that support the use of CBCT imaging on patients with impacted teeth.
2D versus 3D Radiography for Diagnosing Impacted Teeth
Prior to the introduction of CBCT imaging, localizing and diagnosis for impacted canines were performed primarily from 2D radiographs (Power & Short, 1993; Stivaros & Mandall, 2000; Warford et al., 2003). Occlusal and periapical radiographs traditionally have been utilized to localize the position of the canine using the “same lingual, opposite buccal” (SLOB) rule, which generally focuses on localizing the impacted tooth crown’s 2D bucco-lingual position rather than detailing the entire tooth’s 3D spatial position and relationship to surrounding structures. With the growing body of research on CBCT imaging to localize impacted canines, the limitations of making treatment decisions using the SLOB rule and conventional 2D radiographs is becoming increasingly evident, as will be discussed later.
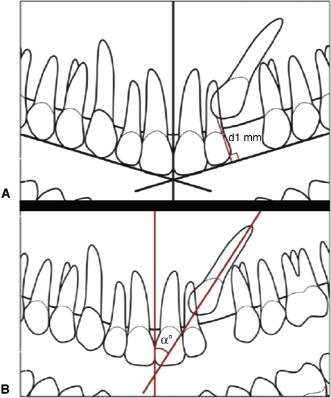
While using conventional 2D panoramic radiographs for localizing an impacted canine is not advised (Nagpal et al., 2009), it has been proposed that panoramic radiographs can be used for early diagnosis of canine impaction in patients as young as 5–9 years old (Novak et al., 2012; Sajnani & King, 2012). Thus, a retrospective study (Sajnani & King, 2012) of 2D panoramic radiographs of 442 patients between 3 years of age to adulthood with at least one impacted maxillary canine demonstrated that the perpendicular distance of the canine cusp tip to the occlusal plane is significantly larger for the impacted than normally erupting canines from age 5 years and up (Figure 16.2A). Also, whereas the normal canine cusp tip did not appear to overlap any part of the lateral incisor, that of the impacted canine overlapped the distal of the lateral incisor root at age 9 years and, on average, eventually overlapped the mesial of the lateral incisor root. Finally, the canine angle relative to the midline was significantly larger for the impacted canine (28.4°) compared with the normal canine (11.3°) beginning at 9 years of age (Figure 16.2B). Moreover, this angulation of the impacted canine increases with age, while the non-impacted canine angle decreases with age. These findings indicate that the canine cusp location relative to the occlusal plane and the lateral incisor and its angulation relative to the midline may be used to predict whether the canine is at risk for impaction.
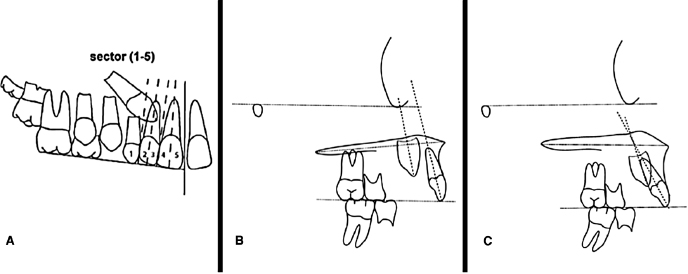
Early diagnosis of potential canine impaction from conventional 2D lateral cephalographs in combination with panoramic radiographs also has been reported in a prospective controlled study of 35 orthodontics patients with at least one palatally displaced canine and 50 patients with normal canine eruption in subjects with a mean age of slightly over 10 years (Novak et al., 2012). The panoramic radiographs were utilized to assess the canine mesial angulation relative to the midline and canine cusp tip distance from the occlusal plane using the same approach as shown in Figure 16.2. In addition, the position of the canine cusp tip relative to the lateral and central incisors was assigned a sector value (Figure 16.3A). The mesial angle of the palatally displaced canine to the midline was significantly larger (27.5°) than the normal canine (7.6°). As opposed to nearly all (92%) of the normal canine cusps being positioned in sector 1, only 23% of the palatally displaced canines were located in this sector. These palatally displaced canines more often were distributed in sectors 2 (43%), 3 (23%), and 4 (11%). There was no significant difference in the distance from the occlusal plane between the palatally displaced and normal canines on the panoramic radiographs. The lateral cephalographs (Figure 16.3B,C) were used to evaluate the vertical angle of the canine to the Frankfort and palatal planes and to the central incisor. The canine cusp tip distance from the central incisor vertical axis parallel to Frankfort Horizontal, anterior alveolar ridge parallel to Frankfort Horizontal, and the functional occlusal plane also were measured from the lateral cephalographs. Each of the angular measurements was smaller, while the linear measurements all were larger for the palatally displaced canines compared with the normally developing canines. These findings provide a guide to assessing the potential for canine impactions using panoramic and cephalometric radiographs.
Assessing impacted canine position on 2D radiographs has been the gold standard for decades largely because 3D radiographs were not available. Also, although previous studies indicate a 92% accuracy of localizing impacted canines from 2D radiographs (Ericson & Kurol, 1986a, 1986b, 1987), recent findings demonstrate a substantial discrepancy between 2D and 3D images in localizing canines and in the detection of root resorption (Alqerban et al., 2009a, 2011; Haney et al., 2010; Katheria et al., 2010; Botticelli et al., 2011). More important, a key question regarding CBCT imaging of impacted teeth is whether the information obtained from these images improves diagnosis, aids in refining treatment plan(s), and, in the long term, improves treatment outcomes. The answer to the first two questions is provided by several recent studies that have demonstrated significant differences in diagnosis and treatment planning and improved confidence in these decisions for impacted teeth when comparing 3D with 2D radiography (Haney et al., 2010; Katheria et al., 2010; Botticelli et al., 2011; Alqerban et al., 2013).
In a study by Haney and colleagues (2010), the investigators sought responses from a group of orthodontists and oral and maxillofacial surgeons on the location and site of surgical access for impacted canines in routine 2D radiographs (panoramic, occlusal, and two periapicals) versus printouts of 3D CBCT images. There was an approximate 20% lack of agreement among clinicians on the palatal versus labial location of the tooth tip between the two imaging modalities. The same lack of agreement was found when determining on which side to start the surgical access, implying that an accurate identification of tooth tip location has a direct effect on site of surgical access. When the treatment plan included forced recovery of the tooth, then the initial force vector selected was influenced significantly by the radiographic modality. Specifically, when these teeth were evaluated with 3D images, the vector was changed for 11 of 12 teeth judged to have an initial distal recovery vector on 2D images. Interestingly, clinicians generated the same orthodontic treatment plan using CBCT and 2D radiographs for only 36% of the impacted teeth, demonstrating large differences in treatment approaches when the two imaging methods were compared. Furthermore, CBCT contributed to significantly higher confidence in diagnosis and treatment planning relative to the combination of panoramic, periapical, and occlusal radiographs. Similar, and in some instances larger, differences in determination of canine or supernumerary positions and treatment decisions between CBCT and conventional imaging have been reported by others (Katheria et al., 2010; Botticelli et al., 2011). Observers in the Katheria study scored a significantly higher proportion of CBCT examinations as “very useful” in treatment planning than conventional radiographic examinations (Katheria et al., 2010). The treatment decisions made differed between the two imaging modalities for 27–30% of the subjects (Haney et al., 2010; Botticelli et al., 2011). While these studies provide sound support for the efficacy of CBCT in diagnosing and treatment planning impacted teeth, it is plausible that the findings would have been strengthened further if virtual images on a computer monitor were used, rather than printouts of the 3D images.
2D and 3D Findings on Root Resorption Associated with Impacted Canines
An ectopic or impacted tooth presents a risk for resorbing roots of nearby teeth, which in the case of impacted canines typically affects the lateral incisor and less frequently the central incisor (Alqerban et al., 2009b; Bjerklin & Guitirokh, 2011; Bertl et al., 2013; Strbac et al., 2013). Because of this, any improved efficacy in detecting root resorption using CBCT rather than 2D radiography that contributes to better and informed treatment decisions could prove to be valuable to the patient and clinician, providing further justification for the use of CBCT for treatment of impacted teeth. Indeed, research findings show not only a 22–36% lack of agreement in the perception of root resorption of teeth adjacent to impacted teeth between 2D versus 3D imaging (Haney et al., 2010; Botticelli et al., 2011), but that the incidence and magnitude of root resorption detected in association with impacted teeth is greater in 3D versus conventional radiographs. Specifically, CBCT is more sensitive than 2D radiographs in detecting root resorption associated with impacted canines (Alqerban et al., 2009a). Furthermore, whereas 2D radiographs reveal root resorption in 30–50% of lateral incisors in individuals with impacted canines, the detection of lateral incisor root resorption increases by at least another 65% when using CBCT (Alqerban et al., 2011). Thus, it is not surprising that 71% of clinicians consider CBCT to be “very useful” for diagnosing root resorption, while only 9% of clinicians say the same about conventional 2D radiographs (Katheria et al., 2010).
Treatment Outcomes as the Gold Standard Evidence for Utilizing CBCT
Despite the current evidence on the value of CBCT in enhancing diagnosis and treatment planning of impacted teeth, additional supporting evidence that CBCT translates into overall better treatment outcomes and efficiency than those resulting from conventional 2D radiographs still is lacking. For this purpose, it is important to specifically determine if information obtained from CBCT imaging improves the success rate in retrieving teeth, contributes to more efficient treatment with shorter treatment times, and decreases morbidity including root resorption and poor soft and hard tissue support better than treatments based on conventional 2D radiography. Derivation of such evidence requires longer-term follow-up studies. While we await treatment outcome–based justification for the use CBCT in treating impacted teeth, the findings that CBCT contributes to changes in treatment decisions in approximately 30% of these cases (Haney et al., 2010; Botticelli et al., 2011) may provide adequate rationale for utilizing CBCT in diagnosis and treatment planning of impacted teeth.
Although data on the efficacy of CBCT in enhancing treatment outcomes and efficiency for impacted teeth are pending, it is reasonable to assume that if the orthodontist or surgeon fails to utilize the information available from CBCT images optimally and instead implements the same or similar treatment approaches and mechanics as done with conventional 2D radiographs, no improvements in treatment outcomes should be expected. Indeed, for improved treatment outcomes and efficiencies, it is imperative that the data from CBCT be utilized fully to refine or modify treatment plans and to implement optimal retrieval mechanics. It is likely that if CBCT-derived information truly is used to comprehend the precise spatial location of the entire tooth and its relationship to neighboring structures and to define optimal surgical access, bond position, and mechanics, enhanced outcomes that include decreased treatment time, improved success rate, and decreased damage to neighboring teeth should result. The sections below outline the recommended imaging, diagnostic, treatment, and biomechanical protocols that can help in achieving the goals of improved treatment outcomes and efficiencies for impacted and transposed teeth.
Protocols for CBCT Imaging of Impacted and Transposed Teeth
Determining Imaging Needs and Field of View (FOV)
As discussed in Chapter 1, before obtaining a CBCT, it is important first to perform a thorough clinical examination to extract and synthesize all pertinent diagnostic information needed for determining whether to take a CBCT and, if needed, which region and FOV will facilitate treatment planning best. The appropriately selected optimal FOV in turn will determine if additional conventional 2D radiographs are needed (see Figure 1.5 in Chapter 1). In general, if the clinical exam reveals that the only reason to prescribe a CBCT image is an impacted tooth, then a small FOV CBCT, which captures the canine, adjacent teeth, and surrounding bony structures, would suffice. On the other hand, if the clinical examination reveals impacted teeth in different quadrants or other significant findings requiring further 3D radiographic information, then the prescribed FOV should be modified accordingly. For example, if the patient is a candidate for orthognathic surgery, then an extended FOV may be preferred. Since a panoramic radiograph can be reconstructed from medium and extended FOV CBCTs and a cephalogram can be derived from an extended FOV, the need for these two types of conventional 2D radiographs will be determined by the preferred CBCT FOV prescribed for the patient. When uncertain about the optimal FOV for a particular patient, consulting an oral and maxillofacial radiologist is recommended. Overall, as with other clinical scenarios, an individualized rather than a routine radiographic protocol should be followed for imaging impacted or transposed teeth (see also Chapters 1 and 6).
Protocols for CBCT Image Interpretation
Given the high percentage of missed lesions and false-positive errors in reading and interpreting CBCT images by orthodontists (Ahmed et al., 2012), it is advisable that the services of an oral and maxillofacial radiologist be utilized to provide a report on the region of interest (ROI) and on any significant incidental findings (see Figure 1.14 in Chapter 1). If clinically significant incidental findings are noted, it is important to refer the patient to the appropriate healthcare provider(s) for follow-up and treatment.
A careful review by the orthodontist of the oral and maxillofacial radiologist’s report and images may aid in making decisions on how to proceed with treating the impacted or transposed tooth. Given that the radiologist may not be aware of the precise information required for surgical and biomechanical decisions and the high level of diagnostically valuable data contained in the CBCT, however, it is important that the orthodontist review and manipulate CBCT images directly on the computer to derive all the pertinent information. This process is perfor/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


