The restorative–endo interface
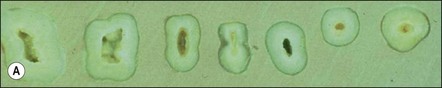
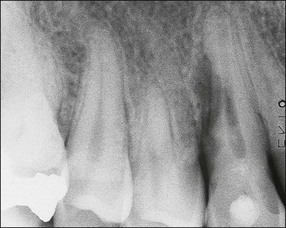
Much has been written about restoration of the root-treated tooth, in part because such teeth are often lacking in sufficient coronal tooth structure and what is remaining may be compromised by cracks or altered physical properties. They therefore, require novel and ingenious methods of restoration that account for their inherent weakness. The spectrum encompassed by the pattern of distribution of remaining tooth structure is broad; attempts have been made to devise an index to characterize it (Fig. 14.1). The distribution of the remaining tooth structure may enable it to be sculpted into a preparation with adequate retention and resistance form for a restoration or it may not (Fig. 14.2). In the latter situation, various dowel systems have been used to supplement retention and resistance form by utilizing the root structure. A wide range of dowel or retention systems is available to aid restoration but significant research to support all the claims of manufacturers is lacking. That root-treated teeth are more susceptible to fracture is a widely held clinical impression and they may, therefore, require different considerations when restoring them compared to vital teeth. The high fracture rate of endodontically-treated teeth, especially immature anterior teeth (Fig. 14.3) and those restored with mesio-occlusal-distal (MOD) plastic restorations (Fig. 14.4) has been documented. Unrestored teeth, particularly mandibular molars, may develop mesiodistal cracks across the marginal ridges in patients with heavy occlusal loading (Fig. 14.5); but maxillary molars are not immune to such damage either (Fig. 14.6). The three main reasons advanced to explain the possible high fracture rate are:
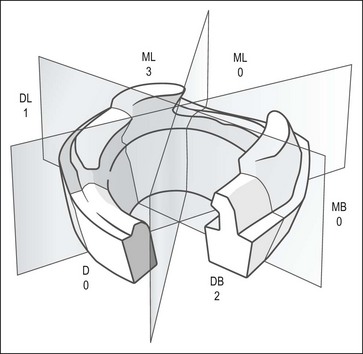
Fig. 14.1 Restorability index (from McDonald A, Setchell D (2005). Developing a tooth restorability index. Dent Update 32(6), 343–4, 346–8)

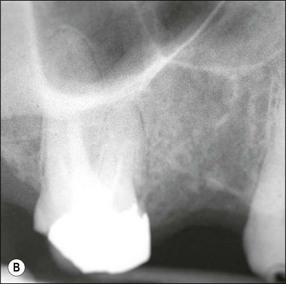

Fig. 14.2 (a–c) Distribution of remaining tooth structure with inadequate retention and resistance form

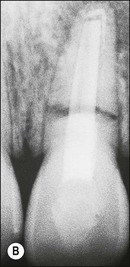
Fig. 14.3 (a) Root-filled maxillary central incisor; (b) middle third root fracture of the same tooth

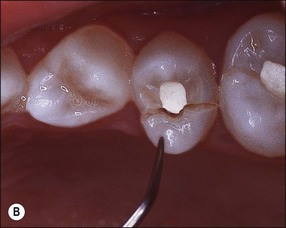
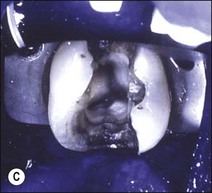
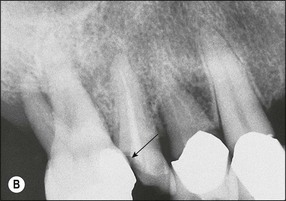
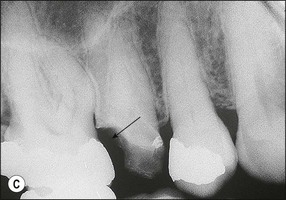
Fig. 14.4 (a) Radiograph of fractured root-treated maxillary premolar; (b) clinical view of a fractured premolar; (c) fracture through floor of the pulp chamber of molar


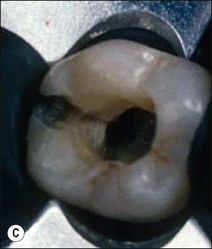



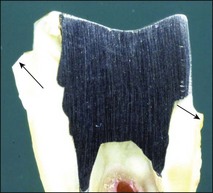
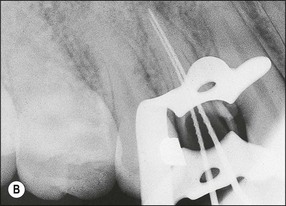
Fig. 14.5 (a–f) Mesiodistal crack (arrowed) developed in the mandibular second molar in a patient with heavy occlusal loading; Pulp extirpation and crack exploration (c); root canal treatment of the orthodontic band-protected tooth (d); MOD onlay preparation (e); and cemented gold casting (f)
1. Altered physical properties of tooth tissue The idea that root-treated teeth are brittle has long been propagated as an explanation for the apparently higher fracture rate of such teeth but no convincing evidence has been found to support the theory. Dehydrated dentine is brittle and hydrated or rehydrated dentine is viscoelastic. The water in the dentinal tubules that confers on the tooth its resilience. Measures to dehydrate teeth may be counterproductive. Given that cementum is permeable to moisture, it is difficult to envisage permanently dehydrated dentine in the moisture-saturated mouth
2. Weakening due to loss of tooth tissue Many studies have evaluated the effect of pattern of tooth-tissue loss as a cause of tooth weakening. The loss of marginal ridge integrity is probably one of the most important factors. The width of occlusal isthmus and depth of cavities compound the situation. Loss of roof of the pulp chamber has been considered to be an important contributory factor in the weakening effect; its importance probably lies in its contribution to the increased depth of the cavity, making the cusps “longer” and more susceptible to flexure (Fig. 14.7a,b). Loading of such cusps may lead to unfavourable stress concentration at the cervical region making the cusps prone to fracture (Fig. 14.7c,d)
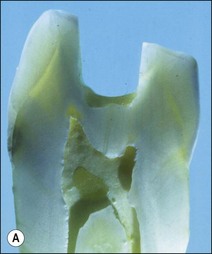
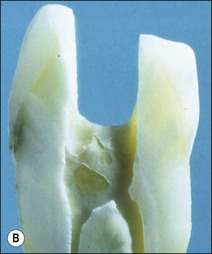
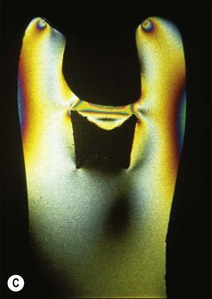
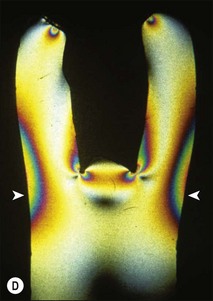
Fig. 14.7 (a,b) Deeper proximal boxes and lack of roof of pulp chamber render cusps more prone to flexure; (c,d) photoelastic model (courtesy of Mr P O’Neilly) showing concentration of stress increases at the base of the cusps (arrowed) when the roof of the pulp chamber is removed
3. Loss of proprioception Loss of the dental pulp may deprive the tooth of some of its mechanoreceptive properties. Teeth without pulps have a higher “load perception” threshold and may take up to twice the load of a tooth with a vital pulp before registering discomfort. Although proprioceptors have not been identified in the dental pulp, there is evidence for Aβ nerve fibres which are reputed to serve a proprioceptive function. Despite lack of clear evidence, this concept is plausible and, together with tooth weakening, offers an attractive explanation for the apparently higher rate of mechanical failure of root-treated teeth.
Restorability of the tooth
The restorability of the tooth should always be determined before endodontic treatment as part of a general restorative and oral treatment plan. Space available should be sufficient to place an aesthetic, functional restoration with cleansable contours, which will optimize the health of the periodontal tissues and adjacent teeth. Often the tooth requiring endodontic treatment is severely broken down and movement of neighbouring teeth may result in occlusal (Fig. 14.8a) and proximal (Fig. 14.8b,c) loss of space, which may occasionally be corrected by orthodontic movement but this is not always a practical solution. Even when the tooth is not to be restored but used as an overdenture abutment, an assessment of the space for a denture is important (Fig. 14.9a,b). A denture with thin metal framework may fracture (Fig. 14.9c).

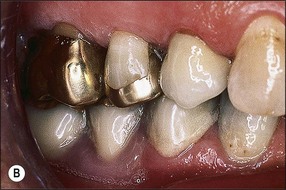

Fig. 14.9 (a,b) Occlusal space considerations for overdenture situation; (c) fracture of denture due to thinness of framework
An adequate amount of remaining tooth tissue is necessary in addition to space. Although it is difficult to describe strict limits, a cast restoration encompassing at least 2 mm of sound dentine around the circumference would make the longevity of the restoration more predictable (Fig. 14.10).
In the absence of sufficient coronal tooth tissue, it may be possible to gain retention from the root. Under such circumstances, it is critical to evaluate the length, width, shape and curvature of the root, to assess the potential use of a dowel. In the absence of sufficient coronal dentine, under exceptional circumstances, it may be possible to extrude the tooth orthodontically. In some procedures, the supporting alveolar and periodontal tissues are extruded with it, which must then be recontoured surgically prior to restoration (Fig. 14.11). Rapid extrusion may allow the tooth to be extruded without the periodontal supporting tissues, circumventing the need for surgery. The long-term predictability of such teeth is not high and such a plan must be agreed with informed consent about the cost–benefit ratio.
How to restore teeth after endodontic treatment
The biomechanics of anterior and posterior teeth are fundamentally different (Fig. 14.12). The anterior teeth serve an incising and tearing function and, in parafunction, serve as the guiding surfaces for mandibular excursions; they are generally not loaded axially except in class 3 malocclusions. The teeth are broader in the labiolingual plane to provide greater bulk and strength in this direction of loading (Fig. 14.13) and, therefore, have long roots that are bulky labiolingually. Posterior teeth, in contrast, serve a crushing, grinding function and have a broad rectangular base with multiple roots, which are likely to be broad buccolingually. They are loaded axially, except in mandibular excursive movements when lateral forces may jar teeth in interference. Such interfering contacts, therefore incur the worst damage on posterior teeth, resulting in cracks and fractures. Anterior and posterior teeth therefore, merit separate consideration in restorative options, not least because of their fundamentally different structures and loading considerations.
Restoration of anterior teeth
Relatively intact teeth
Unrestored anterior teeth may require endodontic treatment because of pulp necrosis caused by traumatic injury (Fig. 14.14), severance of blood supply during surgery (Fig. 14.15), periodontal involvement (Fig. 14.16) or tooth transplantation (Fig. 14.17). Restoration of such teeth would normally be confined to the access cavities (Fig. 14.18) and may be achieved satisfactorily with composite restorative material. In such cases, “reinforcement” of the tooth by placement of a post or dowel remains controversial (Fig. 14.19). The rationale for post placement is based on the belief that the root-treated tooth is inherently weak and that the post would provide a degree of reinforcement by distributing some of the stresses to the root. The scientific support for this is equivocal. It appears that whether a tooth is made more resistant to fracture by placement of a dowel is dependent on the type of loading. It is widely accepted that where a post is not required to aid retention then it should not be placed. If one is placed then it should be at the expense of the minimal amount of tooth tissue. The need for a post is a subjective clinical assessment based on the amount and distribution of remaining dentine after preparation of the tooth for the selected restoration. In Figure 14.20, sufficient dentine cores remained after crown preparation to render post/cores unnecessary whereas, in Figure 14.21, loss of tooth tissue in the three teeth was variable. The gold posts and cores supplemented residual dentine cores. The idea of “reinforcement” has recently been resurrected with the possibility of using adhesive luting cements to bond posts made of materials similar in physical properties to dentine (carbon-fibre or glass-fibre posts). There is, as yet, no long-term clinical evidence to support this concept.

Fig. 14.16 Bone loss around a non-vital mandibular premolar, which has not responded to endodontic treatment – lesion of primary periodontal origin


Fig. 14.20 (a) Adequate dentine cores remaining after crown preparation of root-filled canines render posts or cores unnecessary; (b) buccal view of prepared left canine

Fig. 14.21 As much tooth tissue should be retained as possible, supplemented with a metal core as necessary
Previously unrestored, root-treated teeth sometimes require more extensive restoration than simple access filling, for example, if the crown requires realignment or if its discoloration cannot be dealt with by bleaching alone. The most conservative restoration likely to satisfy aesthetic and functional requirements should be selected so as not to weaken the tooth further. Such restorations may include composite or porcelain veneers (Fig. 14.22), with or without tooth preparation, according to the prevailing preoperative condition. The least conservative preparation is for a ceramometal or pure ceramic crown but, even using this design, the tooth should be prepared to review the need for supplementation of retention by a dowel.
Teeth with proximal cavities
A common clinical situation is one in which an anterior tooth has mesial and distal cavities or restorations (Fig. 14.23). The addition of an access cavity leaves such a tooth with a “band” of missing tooth tissue across the middle of its crown (Fig. 14.24). Provided that the labial enamel plate is intact, relatively strong and unblemished by discoloration or surface deformities, such as pitting, the tooth may be satisfactorily restored with composite restorative materials. A crown may give a better aesthetic result, particularly if adjacent teeth also need to be crowned, but will not necessarily confer greater strength or durability on the tooth. The presence of additional cavities/restorations or tooth-tissue loss would strengthen the case for full coverage cast restorations.
Teeth with inadequate tissue for retention without auxiliary aids
A full coverage cast restoration may be desirable if extensive tooth surface has been lost due to caries, erosion, abrasion, attrition or previous restorations. Poor aesthetics due to large restorations and severe discoloration may also make a full crown more desirable. In such circumstances, the “rooftop” preparations (Fig. 14.25), once recommended, are now considered too destructive. It is considered better to prepare the tooth for the required restoration according to the requisite space demands and make good the tooth-tissue deficit for retention and resistance form with a core retained by a dowel (Fig. 14.26). Spicules of tooth tissue that would not contribute to the strength of the tooth and may jeopardize uncomplicated construction of a core may be sacrificed at this stage (Fig. 14.27). In this way, a more conservative restoration may be constructed.


Fig. 14.27 (a) Following preparation for a crown, spicules of tooth tissue that do not contribute to the strength of the tooth should be sacrificed; (b) this also makes post/core construction easier
1. A temporary post crown may be suitable if the post has adequate length and is well fitting. Otherwise, its decementation may not only cause inconvenience but also allow coronal leakage, further compromising the prognosis of the tooth
2. A permanent post and core may be cemented permanently following root canal treatment if there is a risk of losing the temporary post-crown (Fig. 14.28a), followed by placement of a temporary crown (Fig. 14.28b). This reduces the chances of coronal leakage and, should periapical surgery be required (Fig. 14.28c), allows modification of the margin for a permanent crown once the gingival margin has stabilized (Fig. 14.28d)
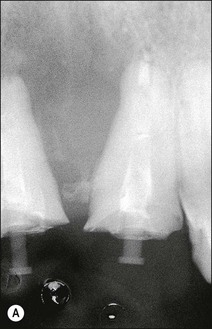

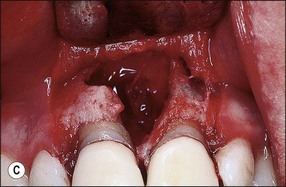

Fig. 14.28 (a) The use of temporary post crowns may be complicated by recontamination of the root-canal system; (b) permanently cemented post, core and temporary crown; (c,d) if surgery is required, the preparation margins may be modified after healing to avoid exposure of the crown/tooth junction
3. A temporary overdenture instead of post-crowns allows the temporary seal to remain intact (Fig. 14.29). If the roots ultimately need extraction, the overdenture also serves as an immediate replacement. The disadvantages include additional cost, time and acceptability to the patient.
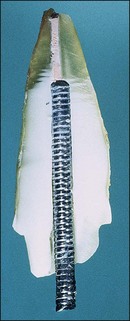
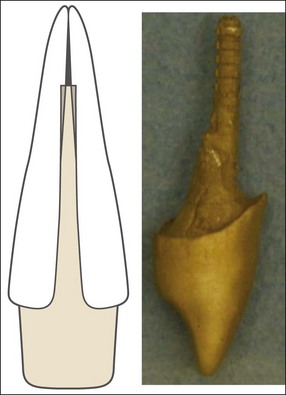
Characteristics of dowels or posts
Dowels may be selected from a range of prefabricated designs (Fig. 14.30) or may be custom-made (Fig. 14.31). Dowels are selected on their properties of retention, stress distribution, ease of application and cost. The characteristics determining retention and stress distribution include material of composition, shape, length, diameter, surface configuration and the presence of a diaphragm.
Shape
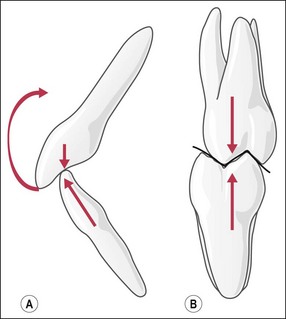
Dowels may be parallel-sided or tapering (Fig. 14.32). The parallel-sided dowels provide better retention per unit length than the tapered dowels. An increase in taper reduces retention. The stress-distributing characteristics of the two designs differ during installation and functional loading. Tapered dowels generate the least stress during cementation (Fig. 14.33a), parallel-sided dowels generate greater stress by virtue of the hydraulic pressure developed (Fig. 14.33b). However, the parallel-sided posts perform better in function (Fig. 14.33c) because tapered posts generate a wedging force (Fig. 14.33d). This may be alleviated if the shoulder rest is firm but this would concentrate stress at the shoulder.
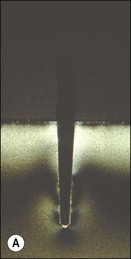

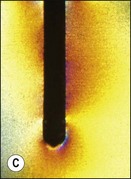
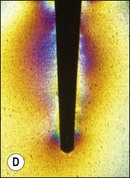
Fig. 14.33 (a) Tapered dowels generate least stress during cementation; (b) parallel dowels generate greater stress during cementation; (c) parallel dowels provide better stress distribution in function; (d) tapered dowels generate a wedging force during function (all courtesy of Mr P O’Neilly)
Although parallel-sided dowels are considered more desirable, the natural tapering shape of roots and prepared root canals mitigate against a dowel parallel along its entire length. Inevitably, the dowel will be tapered in the coronal portion and be parall/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses