CHAPTER 15 Periodontics
Gums and Bone Surrounding Teeth
Periodontics is an area of dentistry that has been neglected significantly by both dentists and patients. this area of dentistry involves the supporting structures of the teeth, primarily the bone of the jaws and the gum tissue. During adulthood, more teeth are lost to periodontal disease than to dental caries (decay). Why has periodontal therapy been neglected? the most important reason is that disease of the gums and bone progresses slowly and usually is not painful. Most patients do not seek treatment for periodontal disease unless they are motivated by their dentist or dental hygienist. The majority of general dentists emphasize other parts of dental practices, such as restoring teeth (fillings), and they do not motivate patients to seek treatment of periodontal disease.
WHAT YOU SEE OR FEEL
Conditions, Signs, or Symptoms Related to Periodontics
1. Bleeding From the Gums
(FIG. 15.1). When you eat hard foods, brush your teeth, or use dental fioss, blood may come from the gum tissue. If you can localize the area of gum tissue that bleeds, you will see that it is usually redder than the normal pink color of healthy gums. Unless you have done something abusive to your gums, such as eating hard foods, overbrushing, or overfiossing, the gums should not bleed. Bleeding gums on a regular basis usually indicate that disease is present in the gums and/or bone. The disease is usually gingivitis (gum infiammation) or periodontitis (gum and bone disease). Such bleeding is often upsetting to patients because it does not seem normal or expected. If the bleeding has been present for a short time, the disease process is probably gingivitis. If bleeding has been present for a long time, the disease has probably involved the supporting bone tissue and is periodontitis. Professional care is needed. The following treatment alternatives are available:
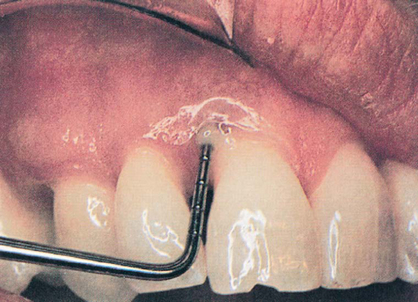
2. Red Gums
(FIG. 15.2). Gum tissue that appears to be redder than normal is usually infiamed and engorged with blood, and the gums may bleed when stimulated. Red gums may be caused by numerous conditions, including frequent mouth breathing that leaves a sticky residue on teeth surfaces, leaving food debris on teeth and gum surfaces for prolonged periods, excessive smoking, or drinking of alcoholic beverages, or presence of long-term gum and bone breakdown that have caused increased blood in the gum tissue.
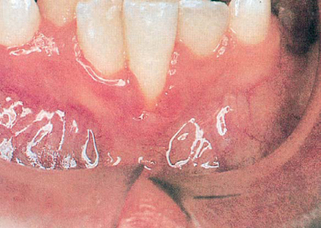
3. Creamy, Yellow Substance Comes From Space Between Tooth and Gums; Foul Odor is Present
(FIG. 15.3). Pus discharge from beneath the gums is a nearly sure sign of advanced periodontal disease (gum and bone degeneration) involving the supporting bone tissue. Pus is food debris, dead cells, and microorganisms (bacteria), and is a sign that infection is present. Stimulation of such gums by eating hard foods or cleaning the teeth can cause the infection to be carried to other parts of the body via the blood (bacteremia). Pus discharge can cause disagreeable mouth odors evident to others close enough to smell the breath. When oral disease is present to this degree, it should be treated as soon as possible to avoid further periodontal breakdown. Although such treatment is more difficult than therapy for less advanced periodontal disease, in most cases teeth can still be saved and effectively used for many years. Alternatives for treatment include the following:
4. Gums Have Receded From Original Adult Level and Are Unsightly or Sensitive
(FIG. 15.4). Over a lifetime, gum tissue slowly recedes naturally, even with healthy and acceptable periodontal structures. Your gums may have receded naturally, and your mouth may be completely normal and healthy for your age. In such situations the gums are pink and firm, and the teeth are strong and immobile when pressure is applied.
Gum tissue may also recede when periodontal disease is present if it has caused significant bone destruction to reduce tooth support (FIG. 15.5). If periodontal disease is present, visible tooth movement may be observed when teeth are moved forward and backward. Tooth roots will be exposed when gums and bone have receded. Tooth roots are a darker color than tooth crowns (enamel-covered portion of the teeth). The point at which the darker root joins the lighter crown of the tooth is the original location of the gums on the tooth for an adult (FIG. 15.6). Root surfaces may be sensitive to touch, hot and cold foods, or cold air. The two colors of the tooth when the gums have receded may look objectionable to you; therefore, there are two separate potential problems related to receded gums: (A) tooth sensitivity, and (B) disagreeable appearance. The following treatment alternatives are available:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses