CHAPTER 15 Maxillary Pterygohamular Subperiosteal Implant Surgery
COMPLETELY EDENTULOUS DESIGNS
Procedure
Reflection
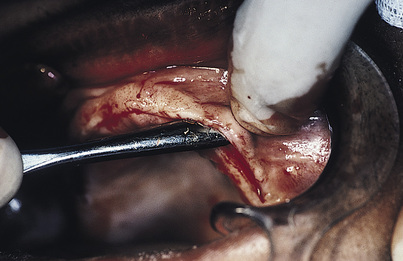
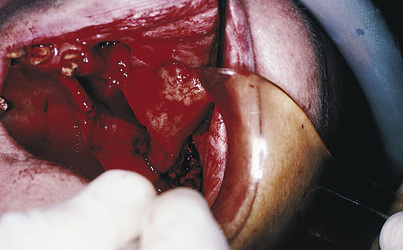
A sharp periosteal elevator is used to lift the palatal flap cleanly from the bone. It is lifted as close posteriorly to the junction of the soft palate as can be managed (Fig. 15-1). This cannot be done without severing the incisive neurovascular bundle, but no significant harm results from doing so. The structures that prevent a complete soft tissue reflection are the greater (anterior) palatine neurovascular bundles bilaterally, and they must be preserved. They may be seen clearly running anteriorly from their foramina (located just medial to the ridge crests in the second molar areas) in the periosteal surface of the reflected palatal flaps. The periosteal elevator is extended behind and lateral to these foramina, and the overlying tissues are lifted away from the hamulus bilaterally (the hamulus is found just at the anterior end of the medial pterygoid plate) (Fig. 15-2).
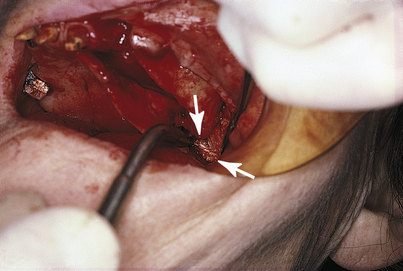
The remainder of the pterygohamular complex is the last structure to be exposed. A Bard-Parker (BP) No. 15 blade on a long handle is used to extend the original incision from the distal end of the tuberosity downward in the mucosa overlying the pterygomandibular raphe. As the mucosa falls open, the gleaming white fibers of the raphe become evident (Fig. 15-3). Blunt dissection with the forefinger on either side of the raphe reveals the attachment of these fibers to the pterygoid plates. The raphe is stretched with the periosteal elevator, and curved or angled, long-handled scissors (Dean) are used to snip away the fibrous attachments, with care taken to stay directly against bone. In most cases, the raphe is extensive, and considerable cutting is necessary. When it finally comes free, it is intact and easy to identify because of its glistening whiteness.
Before making the impression, the surgeon should note the exposed structures: the anterior nasal spine, the pyriform apertures, the canine fossae up to the infraorbital foramina, the base of the zygomas (including a minimum of 3 cm of exposed arch), the lateral maxillae, the lateral and medial pterygoid plates, the hamuli, the greater (anterior) palatine foramina, the palatal surfaces of the maxillae, and the incisive foramen. Sharp spicules of crestal bone and knife-edge ridges are rounded with burs, rongeur forceps, and bone files.
Impression Making
An EZ Tray sheet (see Chapter 14) is placed in the hot water heater at 178° F until it softens. The surgeon lifts the material from the bath while the assistant removes the saline sponges from the wound. As the assistant retracts the flaps, the soft material is slipped beneath them and then teased, massaged, and pushed peripherally to the fullest extent of the dissection. The forefinger is used to press the compliant material over the pterygohamular structures. Before it sets completely, the material is lifted out and reseated several times so that it does not become locked into undercuts.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses