CHAPTER 27 Principles of Occlusion in Implantology
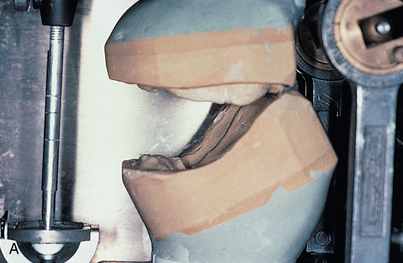
Finally, the natural resorption pattern of edentulous alveolar bone is almost never parallel to the ideal occlusal plane of the dentition. In determining abutment height and position, not only adequacy of interarch space but also orientation of the plane of occlusion must be considered, because a disrupted or incorrectly oriented plane of occlusion makes achieving the optimum occlusal scheme impossible (Fig. 27-1).
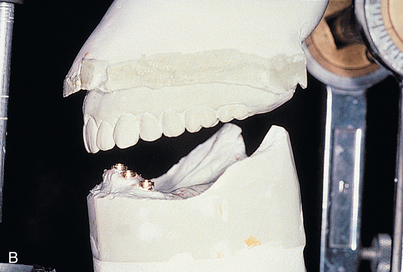
In all phases of prosthetic rehabilitation, the occlusal scheme is designed to meet the requirements of the oral situation. When an implant-supported prosthesis replaces a single tooth in an otherwise intact dental arch, the occlusion is designed like that of a tooth-supported single restoration. This generally is agreed to include lighter than normal tripodal centric occlusal contacts, to prevent supereruption of the opposing natural tooth. Because teeth have a periodontal ligament, they are microscopically compressible. Centric stops are taken by having the patient close hard in centric. The adjacent periodontal ligaments must be compressed to prevent hyperocclusion of the implant restoration. The implant-supported prosthetic crown should follow the guidance of natural teeth in working relationships, similar to other fixed restorations bounded by intact natural teeth (Fig. 27-2).
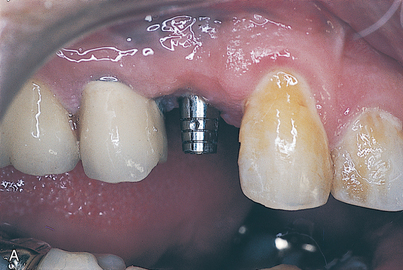
Canine disclusion is used in cases in which natural canine teeth are present and periodontally strong. Where canine teeth are replaced with implant-supported prostheses that occlude with natural teeth or other implant-supported prostheses, group function occlusion supported by natural teeth or other implant-supported prostheses is preferable, to avoid loading a single supporting implant during disclusion. Group function occlusion provides occlusal contact in centric position and in working movements but complete disclusion in balancing positions (Fig. 27-3).
In the complete denture or implant-supported prosthesis, only the maxillary denture moves in function. Soft tissue resiliency and denture movement cannot be relied upon to help balance dynamic occlusal contacts without excessive compressive and tensile forces under the denture base. Occlusal forces generated against the maxillary denture by the implant-supported prosthesis are similar in magnitude to those for cantilever restorations using natural teeth. These forces are many times greater than would be possible with even a well-supported mandibular complete denture, and tissue proprioception of the mandibular denture base is no longer significant. An occlusal scheme that requires movement of the maxillary restoration could predispose the patient to combination syndrome, as has been documented in patients using maxillary denture restorations that provide only anterior tooth contacts in protrusive position.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses