Chapter 15
Management of Emergencies Associated with Pediatric Dental Sedation
Introduction
Medical emergencies, sometimes life-threatening, can and do occur in the pediatric dental office. While one generally thinks of these as affecting the patient, many medical emergencies occur to others in the dental office such as parents or caregivers, the pediatric dentist, and dental staff. Additionally, many pediatric dentists treat patients with special needs who tend to be relatively older, with more “adult” types of medical emergencies. However, the focus of this chapter will be management of medical emergencies directly associated with pediatric sedation. For all other emergency situations, the reader is referred to textbooks devoted entirely to this subject (Bennet and Rosenberg 2002; Malamed 2007).
In-office sedation to treat children has increased over the past fifteen years. It is estimated that up to 20% of children will require pharmacosedation to safely and efficiently complete dental treatment. Children present the highest risk and lowest error tolerance in patient safety during sedation procedures. Although rare, the most serious adverse outcomes of pediatric sedation are brain damage and death. Precipitating adverse events to these tragic outcomes are primarily respiratory, owing to the child’s respiratory and cardiopulmonary physiology and anatomy (Chika 2012). Prevention of an emergency is much more desirable than managing one once it occurs. Most sedation medical emergencies are avoidable. Strict adherence to sedation guidelines does not guarantee that emergencies will not occur, but it will definitely prevent most of them. A recent study of malpractice incidents shows that guidelines were not followed in the majority of cases (Chika 2012). Potential problems also may occur due to poor patient screening before treatment, overdoses of sedation or local anesthesia agents, improper monitoring, and failure to react properly once an emergency situation has been detected.
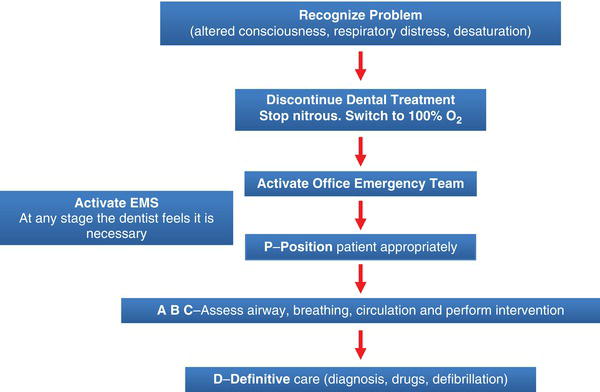
The basic algorithm for the management of most medical emergencies is: (P) position, (A) airway, (B) breathing, (C) circulation, and (D) definitive care: differential diagnosis, drugs, defibrillation. The algorithm will be discussed in detail as it relates to pediatric dental sedation.
Medical History
Familiarity with the patient’s medical history is highly important in preventing medical emergencies. Knowing what to expect of the patient based on her medical history is invaluable. Completion of the medical history questionnaire before the start of any dental treatment is mandatory. The questionnaire may be completed by the patient’s parent or legal guardian (Malamed 2010). In recent years, computerized medical history forms have become available, simplifying the history-taking process.
Next, the pediatric dentist reviews the completed form with the patient’s parent and questions any medical problems that have been reported. Through this dialogue, the dentist seeks to determine any reported medical disorder’s significance to the proposed sedation. For example, if a patient has had an asthmatic attack, the review of the medical history will include the following questions: “How often does the patient experience attacks?” “Are there any specific triggers?” “When was the last attack?” “Did it require a visit to the emergency room or hospitalization?” “Has the child ever required intubation in the hospital to manage the asthmatic attack?” “What medications is the patient taking?” “Does the child carry albuterol with them on a regular basis?” Obtaining medical histories for all patients has been discussed in Chapter Six; however, it is of utmost importance when scheduling a patient to receive sedation.
Physical Examination
The next step is a physical exam. Pediatric dentists actually perform a physical exam on each patient, whether they realize it or not. It may not be as comprehensive or time-consuming, nor is it done in exactly the same fashion as those conducted by physicians, but nevertheless, one is done. The physical exam that pediatric dentists perform is partially formal and partially informal. The informal part consists of things like a simple visual inspection of the patient. By simple observation, the pediatric dentist can determine if a patient has various gross diseases such as obesity, jaundice, exophthalmos, breathing difficulties (asthma or other bronchospastic diseases), or heart defects; possibly even conditions such as attention deficit hyperactivity disorder (ADHD) may be determined. These two items, history and physical examinations, are referred to as the H&P.
The more formal portion of the physical exam consists of such things as recording blood pressure, pulse rate, respirations, height, weight, body mass index (BMI), Mallampati classification and American Society of Anesthesiology (ASA) Score.
Body Mass Index (BMI)
BMI is used as a screening tool to identify possible weight problems for children. The Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP) recommend the use of BMI to screen for overweight and obesity in children beginning at age two.
BMI for age percentile results are divided into four main groups: children under the 5th percentile are considered underweight; those between the 5th to 85th percentile, healthy weight; those between the 85th to 95th percentile are overweight; and those above the 95th percentile are obese, by definition. A recent study examined childhood overweight/obesity as a risk factor for adverse events during sedation for dental procedures (Kang et al. 2012). Overall, weight percentiles were higher in children who had one or more adverse events. Similarly, patients with higher BMI percentiles were more likely to experience adverse events. Although preliminary in nature, these findings suggest that childhood overweight/obesity may be associated with adverse events during sedation for dental procedures. Obese child patients in need of sedation may be referred to a medical center or may be treated together with a dentist anesthesiologist.
Mallampati Airway Classification
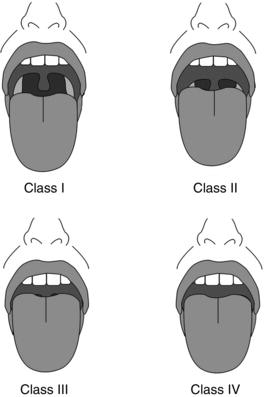
The original Mallampati classification consisted of three classes (Mallampati et al. 1985), but was subsequently expanded into the widely known four-class version (Nuckton et al 2006), as shown in Figure 15-1.
Mallampati (Samsoon and Young) grading of the upper airway is as follows:
- Class I: everything visible (tonsillar pillars)
- Class II: uvula fully visible, fauces visible
- Class III: soft palate and base of uvula visible only
- Class IV: cannot see soft palate
The Mallampati score is an independent predictor of the presence and severity of obstructive sleep apnea. On average, for every one-point increase in the Mallampati score, the odds of having obstructive sleep apnea increase more than two-fold (Nuckton et al. 2006). Patients with obstructive sleep apnea are generally not good candidates for moderate sedation administered by the pediatric dentist, as the perioperative risk to patients increases in proportion to the severity of sleep apnea. The pediatric dentist should consider working with a dentist anesthesiologist to treat these patients (see Chapter Thirteen).
Figure 15-1. Mallampati classification, as modified by Samsoon and Young. Class I: uvula, faucial pillars, and soft palate are visible. Class II: faucial pillars and soft palate are visible. Class III: soft palate is visible. Class IV: hard palate only is visible. Baker, S. and Yagiela, J.A. (2006). Pediatric Dentistry, 28,487–493. Reproduced with permission from AAPD.
By age eight or so, most children have an airway that resembles that of an adult more than that of an infant or small child. Prior to this point, there are significant anatomical differences compared to adults. Infants have a larynx at C3–4—not C4–5, as in adults—that pushes the tongue, that is larger, superiorly. The epiglottis is also larger, stiffer, and angled posteriorly. Pediatric patients have a large thyroid cartilage and a narrow cricoid cartilage—the narrowest portion of the airway in pediatric patients. Infants may require shoulder or neck rolls in the event that they require facemask ventilation. When evaluating infants, pay particular attention to the chin: if it is posterior to the upper lip, a difficult airway can be expected. Nasal and oral airways can be particularly useful in infants or pediatric patients.
After completion and review of the H&P, the dentist assigns the patient to a physical status category. Most patients, especially pediatric dental patients, are quite healthy. By definition, these are “ASA I” patients with low risk of complications.
American Society of Anesthesiology (ASA) Score
The American Society of Anesthesiology (ASA) proposed the physical status (ASA PS) classification of preoperative patients for anesthetic risk assessment in 1963. The ASA score is a subjective assessment of a patient’s overall health based on five classes (see Table 10-3 in Chapter Ten). Only patients with an ASA score of I (a completely healthy, fit patient) or II (a patient with mild systemic disease) should be sedated in a private dental setting. Wolters et al. (1996) examined the strength of association between ASA physical status classification and perioperative risk factors and postoperative outcome, concluding that ASA physical status classification was a predictor of postoperative outcome. To summarize, a patient’s BMI, airway evaluation and ASA score may all be used to screen out potentially complicated patients.
Medical Emergencies
Early recognition of medical emergencies begins at the first sign or symptom (Norris 1994). The pediatric dentist needs to focus on what is happening second-by-second during a medical emergency. Distractions slow response time, and pediatric patients have physiological and anatomical differences from adults. This causes pediatric medical emergencies to proceed much more rapidly than with adults. When treatment is indicated, the dentist should immediately proceed. Management of medical emergencies in the dental office may be limited to supporting a patient’s vital functions until emergency medical services (EMS) arrive, especially in the case of major morbidity. It may also involve real, aggressive action to address a particular situation such as anaphylaxis. Treatment should always minimally consist of basic life support and monitoring of vital signs (Fukayama and Yagiela 2006).
The dentist should never administer poorly understood medications. The drugs discussed in this chapter will be limited to those that a pediatric dentist is trained to use and administer. Since there is no venous access during minimal and moderate sedation, drugs given intravenously will be avoided.
Emergency Kit
A medical emergency kit for a pediatric dental office should consist of three broad categories: equipment, supplies, and drugs. Only equipment and drugs that the pediatric dentist should be able to use confidently will be discussed. However, other components of both equipment and drugs may be required in the dental office. Readers are referred to the AAPD guidelines and to their relevant state or national regulations for other requirements.
Equipment
- Oxygen E tank with regulator, including pressure gauge and flow adjustment
- Pediatric non-rebreather face mask
- Resuscitation bag, adult 1000 mL, with pressure manometer and face mask
- Stethoscope
- Blood pressure cuff (small and medium) and aneroid sphygmanometer
- Automatic external defibrillator programmed to current AHA Guidelines
- Magill forceps. These can be lifesaving in retrieving foreign objects lost in the hypopharynx during dental therapy.
Supplies:
- Yankauer tip. This suction tip is designed to allow effective suction without damaging surrounding tissue. It is used to suction oropharyngeal secretions in order to prevent aspiration.
- Suction tubing, vacuum high volume system adapter
- Nasal cannula
- Nasopharyngeal airways (soft): 4.0, 4.5, 5.0, and 6.0 mm I.D.
- Oral airways (Guedel): 40 mm, 60 mm, and 80 mm
- Laryngeal Mask Supraglottic Airway Sizes 1.5 (5–12 kg), 2 (10–25 kg) and 2.5 (25–35 kg)
Drugs
The following list relates to the limited discussion of this chapter. The basic drug kit for medical emergencies consists minimally of seven drugs:
- Oxygen (E-Cylinder)
- Epinephrine Pediatric auto-injectors (0.15 mg/actuation), epinephrine adult auto injector (0.3 mg/actuation) and 1:1000 (1 mg/ml) ampule—quantity two.
- Albuterol (Ventolin) inhalation aerosol (90 mcg/actuation)
- Diphenhydramine parenteral injection, 50 mg/mL
- Aspirin 325 mg, non-enteric coated
- Nitroglycerin, 0.4 mg tablets
- A form of sugar
Additional required medications if oral sedation using narcotics and/or benzodiazepines are used include Naloxone (0.4 mg/mL, 1 mL vial) and Flumazenil (0.1 mg/mL, 10 mL vial). The latter drug is to be administered IV only.
- Albuterol is used in bronchospastic medical emergencies (acute asthmatic attack) as an inhaled beta-2 specific agonist. It causes bronchodilation that increases the lumen size of the bronchioles, leading to better oxygen uptake.
Dose: Two puffs with deep inspiration.
[source: drug package insert] - Epinephrine is the universal agonist; it affects alpha one, alpha two, beta one and beta two receptors. This is the only drug in the medical emergency kit that must be given rapidly in order to save a patient’s life. In case of anaphylaxis, the severe life-threatening allergic reaction, this is the only drug that will help. Alpha one agonistic activity increases blood pressure by causing a vasoconstriction. Beta one effects of epinephrine increase heart rate, force of contraction, stroke volume, and cardiac output. Epinephrine’s beta two effects cause bronchodilation, making breathing easier. It may also be used for severe asthmatic attacks unresponsive to albuterol.
Dose: Pediatric 0.01 mg/kg IM maximum 0.3 mg/dose. Adult: 0.3 mg/dose
[source: drug package insert] - Diphenhydramine is used for mild allergic reactions. Histamine blockers reverse the actions of histamine by occupying H1 receptor sites on the effector cell, and are effective in patients with mild or delayed-onset allergic reactions.
Dose: 1–2 mg/kg IM up to 50 mg.
[source: drug package insert] - Naloxone is required in the medical emergency kit only if sedation using an opioid is used in the pediatric dental office. Naloxone is the specific antagonist for any of the opioids. It may be administered IV or IM, and has a duration of action of roughly 45 minutes if administered IV, and four hours if administered IM.
[source: package insert for Narcan] - Flumazenil. Most regulatory jurisdictions will require the immediate availability of flumazenil as a required component of the medical emergency kit if sedation using a benzodiazepine is used in the pediatric dental office. While this drug may be legally required, it must be strongly emphasized that the package insert for flumazenil, in no uncertain terms, explicitly says that this drug must be administered IV only. Therefore, if no one in the pediatric dental office is trained to start an IV and uses it regularly, the reality is that flumazenil will not be a valuable drug in a medical emergency.
[source: package insert for Romazicon]
Management of Medical Emergencies
An emergency management plan, as described by Haas (2010) and by Peskin and Siegelman (1995), is of paramount importance. It is recommended that all medical emergencies be managed in the same way by using what is known as the basic algorithm (Malamed 2007): (P) position, (A) airway, (B) breathing, (C) circulation and (D) definitive care: differential diagnosis, drugs, defibrillation (see Figure 15-2).
The one exception is cardiac arrest, where the currently suggested algorithm is (C) circulation, (A) airway, and then (B) breathing. The basic algorithm for managing all medical emergencies is consistent—that is, one algorithm fits all cases, and all cases are worked through in the same organizational method each and every time. This adds consistency and predictability to a response to a medical emergency. Prevention, prompt recognition, and efficient management of medical emergencies by a well-prepared dental team can increase the likelihood of a satisfactory outcome. Note that drug therapy is always secondary to basic life support. The basic intent in responding to a medical emergency is always the same: ensure that the patient’s brain receives a constant supply of blood containing oxygen and glucose with enough perfusion pressure to keep it functioning, and without morbidity.
Recognize the Problem
Prior to initiating the emergency logarithm protocol, the pediatric dentist needs to recognize that an emergency situation is present. Recognition of the sedated pediatric patient’s problem comes about by continuous monitoring, as per AAPD guidelines. The patient’s pulse, oxygen saturation, and breathing should always be within age-appropriate normal ranges. Heart rates are typically higher in children and decrease with increasing age. For example, the normal ranges are 80–130 BPM in a two-year-old, and 70–110 BPM in a ten-year-old (Haas 2010). Any changes need to be immediately identified and analyzed. The following can be regarded as warning signs:
- Change in saturation level: If this occurs, reposition pulse oximeter probe (or, if the extremity is restrained, loosen strap), reposition head, and raise the chin. If level returns to normal, continue treatment.
- The unresponsive sedated patient: For the most part, pediatric dentists only administer minimal and moderate sedation. Patients undergoing such sedations should be responsive.
Figure 15-2. Dentists should initially manage all medical emergencies in the same way by using what is known as the basic algorithm. Based on Malamed, S.F. (2007). Medical Emergencies in the Dental Office. 6th ed. St. Louis: Mosby.
A sedated patient who fails to respond may have advanced to a state of deep sedation, which represents an emergency situation. Therefore, the dentist should cease treatment and evaluate the patient’s state. To begin patient evaluation, try to elicit a response. After verifying unresponsiveness by stimulating the patient, including head tilt and jaw lift (Figure 15-3), remove rubber dam.
If using nitrous oxide sedation, immediately deliver 100% oxygen. Activate the office emergency team/plan/protocol. Emergency medical assistance (EMS) should be sought once the dentist, who is legally responsible for the patient, feels it is needed.
Following these steps, proceed immediately to (P) position: place the patient supine in the dental chair with legs elevated slightly (Figure 15-4).
Figure 15-3. The head-tilt chin-lift maneuver. Courtesy of Dr. Ari Kupietzky.

Figure 15-4. The patient is placed supine in the dental chair with legs elevated slightly. Courtesy of Dr. Ari Kupietzky.

Chest compression, if needed, can be effectively performed in the dental chair. Lepere (2002/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


