15
Gerodontology
- Physiological age changes
- Pathological age changes
- Dental and oral conditions in the elderly
- Treating the dentate elderly
- Domiciliary care, equipment and treatment
- Treatment of the terminally ill patient
Introduction
Gerontology also comes under the title of geriatric dentistry or gerodontics and can be most simply defined as dentistry for the elderly. How older people are defined can be problematical. For some it is those who have reached the age when they receive a state pension (65 for men and women, as from 2010), but for those who have just reached that landmark it could be 75 years! It has been suggested that rather than having a defined chronological age, a biological age should be considered to be more relevant.
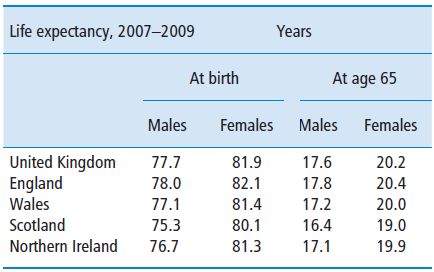
The UK has an ageing population (Figure 15.1). The population grew by 6.5% in the last 30 years, from 55.9 million in 1971 to 59.6 million in mid 2003. Continued population ageing is inevitable during the first half of this century, since the number of elderly people will rise as the relatively large numbers of people born after the Second World War, and during the 1960s baby boom, become older. The working age population will also fall in size as the baby boomers move into retirement, because relatively smaller numbers of people have been born since the mid 1970s. Current (2007-based) life expectancy of 77.7 years for men and 81.9 years for women compares with the1901-based life expectancy of 45 years for men and about 49 years for women (Office of National Statistics, 2009) (Table 15.1).
Figure 15.1 UK population by age.
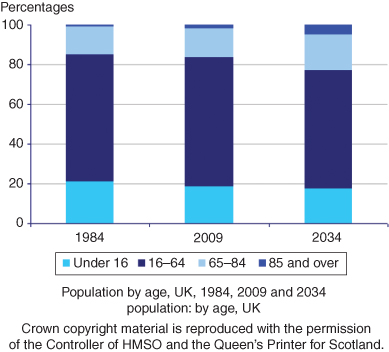
Table 15.1 Interim life tables.
Source: Office for National Statistics: Interim Life Tables 2007–09.
There has been an increasing demand for dentistry for the elderly. There are three main reasons for this:
- The population of the UK is ageing. The increased life expectancy along with the falling birth rate means that the proportion of the population aged over 65 is projected to rise from its current figure of 16% to nearly 23% by the year 2034.
- The improvement in general dental health has meant that people are keeping their teeth for longer. In 1988 21% of all adults in the UK were edentulous; in 1998 this had reduced to 13% (Kelly et al., 2000) and to 6% in 2009. This has resulted in a corresponding reduction in the wearing of full dentures.
- This has, in turn, led to a general expectation and a desire in the older age groups to retain teeth for as long as possible.
There are several factors associated with dental care for the elderly. These are:
- Age changes.
- Diseases.
- Medication.
- Delivery of care.
Physiological age changes
An exact dividing line between changes which are physiological and pathological cannot always be drawn.
General body changes
In general the changes in the elderly are:
- A lengthening in the time taken to repair tissues. This can have important implications when surgery is involved.
- Loss of muscle mass (sarcopenia) and strength, which is one of the most obvious effects of ageing.
- A reduction in the metabolic rate. Basal metabolic rate (BMR) is the minimal caloric requirement needed to sustain life in a resting individual. The BMR reduces with age. After 20 years of age it drops about 2% per decade. It is generally accepted that decreased lean body mass (LBM) with ageing is responsible for a decline in BMR in the elderly.
- Reduction in cellular reproduction. This delays the repair process.
- Reduction in the blood circulation. The elderly tend to restrict their body movements more and more so that eventually, their capacity for mobility becomes markedly reduced and they generally perceive stiffness. Mobility is important to tissue fluid exchange, and so limited mobility seriously reduces blood flow. Blood flow in some circumscribed areas can become so sluggish that the tissues become ischaemic (decreased blood flow).
- Increase in fibrosis. This can occur in many organs, such as the lungs and heart, reducing their function.
- Degeneration of the elastic and nervous tissue. Ischaemia can lead to nerve tissue degeneration and loss of sensory input.
- General reduced function of most body systems.
- A loss of cartilage and bone. A loss of cartilage in bone joints can lead to pain, stiffness and loss of function. Osteoporosis, which literally means porous bones, occurs when the holes within bone become bigger, making it fragile and liable to break more easily. Osteoporosis usually affects the whole skeleton but it most commonly results in fractures to bone in the wrist, spine and hip. The decrease in the reducible collagen cross-links without an alteration in collagen concentration tends to increase bone fragility. When bone tissue becomes too highly mineralised, it tends to become brittle. One in 3 women and 1 in 12 men in the UK experience osteoporosis over the age of 50. The increased bone turnover following the menopause reduces overall tissue mineralisation. At the time of writing the jury is out as whether there is a link between osteoporosis and periodontal bone loss, but two of the most recent studies; Gomes-Filho et al. (2007) and Nicopoulou-Karayianni et al. (2009) have shown a link. However, it is worth noting that not all studies have shown a link. In practical terms, the periodontal disease is treated and the osteoporosis is treated and any link is academic.
Patients with oesteoporosis can be treated with bisphosphonates and evidence has emerged that patients taking bisphosphonate drugs are at risk of developing oesteonecrosis of the jaws, sometimes spontaneously, but more usually following dental extractions or oral bone surgery.
Bisphosponates are principally used in the treatment of oesteoporosis, Paget’s disease, multiple myeloma, bony metastic lesions and hypercalcaemia of malignancy. The incidence of bisphosphonate-related oesteonecrosis of the jaw (BRONJ) in patients taking oral bisphosphonates for oestoeporosis has been estimated at 1 in 10 000 to 1 in 100 000. Patients taking high dose IV bisphosphonates for cancer are much more at risk (estimated at 1 in 10 to 1 in 100). Other factors associated with an increased risk include dental infection, denture trauma and the risk increases with the length of time the patient has been taking the drugs, with 3 years being the threshold.
Presenting features of BRONJ are:
- Delayed healing.
- Pain.
- Swelling.
- Loosening of teeth.
- Paraesthesia.
- Purulent discharge via intra- or extraoral sinus.
If any of these features develop, early referral to an Oral Surgery or Oral Maxillo Facial Surgical Department is important.
Oral
Oral soft tissues
- Decrease in taste bud function.
- Increase in the size and number of Fordyce spots (enlarged ectopic sebaceous glands in the mucosa of the mouth, lips, cheek and tongue), lingual varices and foliate (leaf-like) papillae.
- Decrease in the thickness of the epithelium and mucosa.
- Decrease in saliva flow (xerostomia) and changes in its composition.
Dental hard tissues
- Tooth wear is a natural age-related factor. There is a loss of tooth tissue due to attrition, resulting in a loss of occlusal morphology. Abrasion can be excessive at the cervical margins as a result of prolonged incorrect toothbrushing techniques. Erosion may be more evident as a result of prolonged intake of acid-based or sugary medication.
- Enamel is less permeable.
- Cementum undergoes continuous deposition with age. This is mainly functionally induced and is more pronounced in the apical third of the root.
- The volume of secondary dentine increases, although the rate of deposition decreases with age. The amount of sclerotic root dentine increases with age, proceeding from the apex towards the crown of the tooth. There are obvious optical changes in the dentine, which becomes translucent (dentine is normally opaque). The dentine of older people is characterised by the continuous narrowing of the lumen of the dentinal tubule, increased calcification, a reduction in the amount of peritubular fluid and reduced sensitivity. As a result, dentine tends to be able to take on the function of enamel as it wears.
- There is a reduction in cellularity in the alveolar bone and the surface in contact with the periodontal ligament appears more jagged.
Dental pulp
- Increase in fibrosis and a decrease in vascularity result in the pulp’s defensive properties being reduced, but the pulp does not suffer any appreciable loss of vitality. Circulation in the pulp is affected by deposition of mineralised tissue in the apical part of the root canal.
- Increase in pulp calcification. Pulp stones are more evident.
- The volume of the pulp decreases with age, owing to the deposition of secondary dentine.
Periodontium
- An increase in fibrosis. It is generally agreed that the degree of periodontal breakdown increases with increasing age. The extent to which ageing of periodontal tissues plays a part in this respect poses a question which has yet to be answered. Ageing is accompanied by a variety of periodontal changes. The periodontal tissues themselves show evidence of ageing; there are indications that the composition of the plaque changes, and the reaction of the periodontium to the presence of plaque probably changes as well. In plaque there is a decrease with age in the number of viable microorganisms, an increase in the number of spirochaetes and a reduction in the number of streptococci (Milward and Cooper, 2005). There is as yet no significant evidence of a physiological apical migration of the epithelial attachment. It seems plausible that periodontal breakdown can occur only in the presence of plaque, or as a result of trauma with consequent inflammation of the periodontium. Whether changes in plaque composition with age exert any influence on the course of periodontal breakdown is uncertain: the data available are not yet sufficient to warrant definite conclusions. The same applies to the influence which a changing reaction of the periodontium to the presence of plaque may have on the course of periodontal breakdown. Research findings do suggest that the degree of periodontal breakdown increases with age; that with increasing age inflammation of the periodontium tends to develop more rapidly; and that in the process of ageing the periodontium shows a slower rate of wound healing. However, these phenomena are overshadowed by the patients’ susceptibility to periodontal disease. This implies that firstly, the susceptibility to periodontal disease is more significant for the rate of periodontal destruction than the length of time plaque is present (the age effect) and secondly, the greater the susceptibility to periodontal disease, the slower the rate of wound healing and the more rapidly inflammation of the periodontium tends to develop (Van der Velden, 1984).
- A decrease in cellularity, vascularity and cell turnover is found with an increase in age.
- Collagen and protein synthesis decrease.
Pathological change
Systemic
There are several systemic conditions which are not uncommonly seen in the elderly, which may have an effect on treatment planning and delivery of care. The reader is referred to a more comprehensive text addressing the large number of pathological conditions affecting patients of all ages and having an impact on oral health care (Nunn, 2004) but the conditions more specifically related to the elderly are described below.
Endocrine disorders
Hypofunction of the adrenal glands (Addison’s disease)
This can produce symptoms of tiredness and confusion and lead to a greater incidence of heart attack. Patients may feel dizzy on getting out of the dental chair and do not respond well to the stress of dental procedures. It may be advantageous to keep appointments short.
Hyperfunction of the adrenal glands (Cushing’s syndrome)
This can be due to, for example, a pituitary tumour, or the symptoms may be simulated by high steroid dosage. Patients on steroid therapy are susceptible to a steroid crisis and their physician may advise an increase in dosage when undergoing stressful dental treatment.
Diabetes
This is due to a lack of insulin and can occur in several forms. Type 2 diabetes is the most common type seen in older people. These patients may exhibit signs of decreased salivary flow, increased caries if uncontrolled, periodontal problems due to microvascular changes and slow wound healing.
Hyperparathyroidism
Excess of parathyroid hormone (PTH) is usually as a result of a tumour. It results in demineralisation of the bone, causing possible bone fractures, and renal calculi may develop because of the excretion of high levels of phosphate and calcium.
Hypothyroidism (myxoedema)
This is a condition in which the body lacks sufficient thyroid hormone (thyroxine). Since the main purpose of thyroid hormone is to maintain the body’s metabolism, people with this condition will have symptoms associated with a slow metabolism. Its incidence increases with age and such patients appear lethargic and slow, have cold dry skin and may have an enlarged tongue. They respond poorly to stress.
The immune system
A reduction in the cell-mediated response and a decreased number of circulating lymphocytes results in an increased incidence of autoimmune disease, combined with a reduced defence against infection with age. As stated above, steroid treatment for autoimmune disease can influence dental treatment because of the suppression of the patient’s natural adrenal activity.
Cardiovascular disorders
Hypertension and ischaemic heart disease become more common with an increase in age. Anaemia is also more common in the elderly. Generally, the greatest problems with patients with cardiovascular disorders are associated with general anaesthesia.
Pulmonary system
Lung capacity is decreased with age and chronic obstructive airway diseases are more common.
Muscular system
There is a number of muscular dystrophic diseases which are associated with a decrease in the bulk of the muscle, with slower contractions and less precision of control.
Neurological disorders
There is a physiological decline in function associated with age-related disease.
Parkinson’s disease
This is a condition seen mainly over the age of 50 years. Parkinson’s disease occurs when a group of cells, in an area of the brain called the substantia nigra, that produce a chemical called dopamine, begin to malfunction and eventually die. Dopamine is a neurotransmitter, or chemical messenger, that transports signals to the parts of the brain that control movement initiation and co-ordination. When Parkinson’s disease occurs these cells begin to die at a faster rate and the amount of dopamine produced in the brain decreases. The symptoms include tremor of the hands and arms, drooling due to swallowing difficulties, postural instability and speech difficulties.
Dental treatment can be improved by the provision of mouldable head supports and mouth props. Patients are best treated upright in the dental chair because of the difficulty in controlling the airway. Treatment can usually be more successful if undertaken within 2 hours of taking anti-Parkinsonian medication.
Dementia
Dementia is due to a wasting of nerve fibres in the brain. Alzheimer’s disease accounts for half of all cases of dementia in older people (5% of people over 65 years; 20% of those over 80 years of age). Patients may be treated by a variety of drugs, although older people tolerate these less well. Some of these drugs have xerostomia as an important side effect. Dental treatment can become increasingly challenging as the condition degenerates. Teeth with a poor prognosis, such as those with a furcation involvement, are probably better removed.
Cerebrovascular accident (stroke)
In older patients this can be due to high blood pressure, the use of anticoagulants (e.g. warfarin), or following heart surgery. Tolerance of dental treatment may be reduced and therefore short appointments are advisable. Patients may have difficulty in swallowing and may tolerate treatment better in an upright position. They may have to be treated in their own wheelchair or in a domiciliary setting.
Psychiatric disorders
Depression
This condition is not specifically related to age but is not uncommon in the elderly. These patients may exhibit signs of oral neglect through lack of self-motivation and low self-esteem. They may have symptoms of xerostomia due to drug therapy. They usually require extensive oral hygiene instruction and supervision with plenty of positive encouragement combined with a high dosage of topical fluoride. Appointments are best kept short.
Schizophrenia
These patients demonstrate thought disturbances, sometimes experience bizarre delusions and have difficulty in communicating with other people. Antipsychotic drug therapy tends to increase the heart rate and patients are generally restless when having dental treatment. They don’t respond well to sudden movements of the dental chair. The drug therapy also causes xerostomia with the added problem of an increased risk of extensive dental caries.
Oral
These conditions are covered in more detail in Chapter 3 but there are several mucosal diseases which are more common in the elderly. Some examples are given below.
Leukoplakia
This presents as white patches on the oral mucous membranes, which cannot be removed by scraping. The condition does not reverse with the removal of local irritants. It most commonly occurs between the ages of 40 and 70 and is more common in males (65%). It is usually located around the buccal gingivae or the floor of the mouth. It can be associated with tobacco, alcohol, candida infections or chronic persistent irritants, such as ill-fitting dentures. It requires investigation since these lesions can be considered to be pre-malignant until proven otherwise.
Oral cancer
Whilst oral cancer is a relatively uncommon condition it does increase in occurrence in older adults. If it is not detected early, the survival rate in the elderly is poor. The most common sites are the lips followed by the tongue. Depending on the stage of the disease, survival can be as low as 50%. Approximately 90% of oral carcinomas are squamous cell carcinomas.
If an ulcer with a raised, rolled edge with hardening around the periphery of the lesion is detected, then a thorough history of the ulcer should be taken and the patient referred back to the prescribing dentist as soon as possible.
Candidal infection
This can be either chronic or acute. Acute/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


