15
Assessment of Root Position and Morphology by Cone Beam Computed Tomography
Introduction
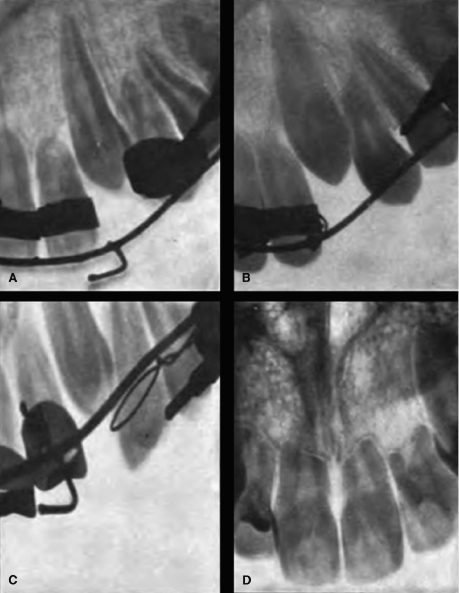
Following the groundbreaking invention of X-ray technology by W.C. Roentgen, C.E. Kells wasted no time in adapting it to dentistry. Roentgen introduced radiology to the world in November 1895, and Kells began using dental radiographs in the spring of 1896 (Hubar, 2000). Not long afterward, dental radiography was commercialized for use in every dental specialty. R. Ottolengui was one of radiography’s early adopters and he published a manuscript entitled The Physiological and Pathological Resorption of Tooth Roots (1914), complete with startling images of severely resorbed roots in an orthodontics patient (Figure 15.1). F.C. Kemple, who opened the discussion of Ottolengui’s paper, set the trajectory on inquiry in this field for future clinicians and researchers:
The radiographs shown by Dr. Ottolengui seem to open up a new field of difficulty and complication and study, not only for the orthodontist, but also for the physiologist and the pathologist…. [T]he absorption of the roots of permanent teeth, which are to all appearances perfectly healthy, is a phase of the subject that has not been studied, or at least it has not been discussed in the dental literature. It is this phase of the subject that so vitally interests the orthodontists, and I hope that Dr. Ottolengui and others will continue to study and discuss this question from year to year until a satisfactory solution of the question has been reached.
Kemple would no doubt be surprised to learn that 100 years of study and discussion have not yielded the satisfactory solution he eagerly sought to the problem of root resorption.
This historical snippet serves two purposes. First, it emphasizes the indispensable role radiology plays in diagnosing pathology, thereby justifying continued research to improve radiographic technology to ensure safe high quality imaging of our patients. Second, it serves as a cautionary tale for researchers, clinicians, and patients who misjudge the promise of powerful new technologies. Cone beam computed tomography (CBCT), like two-dimensional (2D) radiography in Ottolengui’s day, offers unprecedented images of teeth before and after orthodontic treatment. But, as clearly demonstrated by the past 100 years of imaging, radiography alone is powerless to solve the problem of understanding and preventing root resorption. Radiographs, regardless of their dimensionality, map the resulting topography of ectopic eruption or orthodontic forces but offer no insight into the complex biological processes and genetics that account for the pathology. In this chapter, we will continue what Ottolengui and Kemple began in 1914 by discussing how the latest radiographic technology—CBCT—contributes to our understanding of physiological and pathological root resorption, with a special focus on orthodontics patients. This discussion traces CBCT’s emergence as an accurate and reliable methodology for assessing root angulation and morphology, which are among the most well-studied risk factors for root resorption. In addition, we will discuss the contribution of CBCT to our understanding of other clinically relevant aspects of root morphology, such as dentoalveolar compensations and dilacerations, as well as the emerging use of CBCT root imaging to gain insights into the biological connections between root morphology and complex craniofacial anomalies.
Accuracy of Root Angulation and Length Measurements on 2D and 3D Radiographs
Any emerging technology must be put through its paces before it can be incorporated into the clinician’s armamentarium rightfully. CBCT has been available commercially for more than 10 years, and its value to dentists for diagnosis and treatment planning is now accepted widely (Scarfe et al., 2012). Orthodontists have embraced CBCT imaging because its three-dimensional (3D) rendering capability is suited ideally for imaging skeletal and dental malocclusions, which are 3D problems. Moreover, combining 3D radiographs with clinically observable dental crowding, spacing, or anomalies gives a much more complete picture of how the teeth develop, erupt, and take their final positions as the primary and permanent occlusions emerge. This information is vital for orthodontic diagnosis and treatment planning because correcting malocclusion is not a simple matter of aligning the crowns. Root position and morphology are critical considerations for ideal orthodontic treatment for two reasons: (1) root position and parallelism are considered critical for an ideal stable occlusion (Bert, 1981; Mayoral, 1982; Casko et al., 1998); and (2) external apical root resorption (EARR) is one of the few common adverse side effects of orthodontic treatment. As will be discussed, one risk factor for EARR is the magnitude of apical root movement, which can be determined only from radiographs. CBCT radiographs are valuable especially because they allow precise measurements of root angulation and length before and after orthodontic treatment. Given the importance of angular and linear root measurements for orthodontic diagnosis, treatment planning, and outcomes assessment, we will compare measurement accuracies of 2D and 3D radiographs.
Methodological Approaches to Measuring Root Angulations
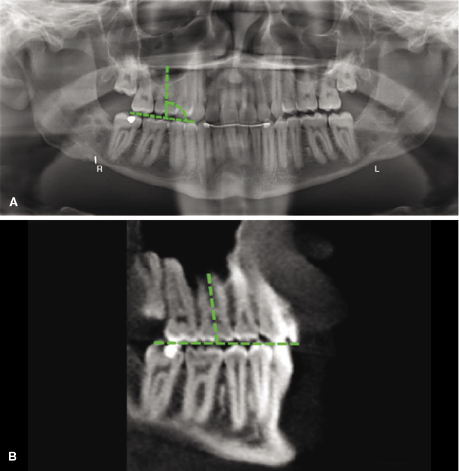
Before proceeding to a discussion of radiographic studies of root angulation, it is important to understand how root angles are measured on radiographs, typodonts, and living human subjects. Root angulation measurements on radiographs methodologically are the simplest. Most often, root angulation is assessed on either conventional 2D or CBCT-extracted panoramic radiographs and is defined as the angle formed by the tooth’s long axis and the occlusal plane (Figure 15.2). Ideally, this angle is 90° on a conventional 2D panoramic radiograph. When periapical radiographs are used, the tooth’s long axis again is used to form an angle with some other researcher-defined reference line or plane. These approaches are used both for typodont- and human subject–based studies.
In typodont-based studies, root angles measured directly on the typodont are compared with the corresponding angles on the radiograph. The question that arises with this approach is this: How does one measure root angles on a typodont? A common method employs a coordinate measuring machine (CMM), which uses a probe to digitize researcher-determined landmarks on the typodont teeth (McKee et al., 2002; Garcia-Figueroa et al., 2008; Owens & Johal, 2008; Tong et al., 2012a, 2012b). This establishes a tooth’s x, y, and z coordinates, which are input into a computer program that then calculates the tooth’s angle relative to a reference archwire that was placed on the teeth prior to digitizing.
Root angulation measurements in living human subjects cannot be obtained directly without surgical intervention. This highlights a caveat that must be acknowledged when designing or evaluating root angulation studies. Regardless of the medium from which root angles are measured—whether 2D radiographs, 3D radiographs, or dental casts—all of the measurements are indirect, and there currently is no way to verify the accuracy of these measurements. The best a clinician or researcher can hope for in human subject–based studies is to determine how the measurements obtained from different media compare with each other (e.g., 2D vs. 3D radiographs) or to determine how the measurements taken from a single medium change over time or after a specific treatment regimen. However, dried skull phantoms can serve as proxies for living human subjects to assess radiographic accuracy, but obviously not to assess treatment outcomes.
Accuracy of Root Angulation Measurements on 2D and 3D Radiographs
Andrews (1972) proposed six keys to normal occlusion based on his analysis of 120 dental casts from individuals with an ideal occlusion; among these keys is crown angulation and crown tip. Since crown-to-root angulations can range from normal to severely dilacerated (Carlsson & Rönnerman, 1973; Knösel et al., 2009; Xuan et al., 2010), the need for radiographic data on root angulation to diagnose accurately and plan treatment for orthodontics cases now is recognized widely (Tong et al., 2012a). Root angulations are assessed to ensure that the teeth are positioned stably in the alveolus. Proclined or retroclined incisors and lingually/palatally or buccally inclined posterior teeth are considered unstable and potentially harmful as dehiscences or fenestrations may result (see also Chapter 14). In this section, we will discuss the importance of radiographic accuracy when assessing root angulations.
Root parallelism typically is assessed on conventional 2D panoramic radiographs. Unfortunately, parallelism on these radiographs is an optical illusion due to multiple confounding problems (McKee et al., 2001; Hardy et al., 2009; Dholakia & Bhat, 2011; Pfeiffer et al., 2012). The preset arc of the panoramic X-ray machine, highly variable craniofacial geometries, and inconsistent head positioning prior to imaging all distort and magnify anatomic structures on 2D panoramic radiographs. While CBCT machines also have a preset arc, the collection of multiple images throughout that arc allows a volumetric or 3D image to be generated, rather than the single flattened image on conventional films. Using specialized software, the 3D volumes can be rotated to visualize structures directly, place landmarks, and take measurements that are free of the distortion and magnification artifacts that plague conventional 2D radiographs.
The magnitude of angular distortion that affects our perception of root parallelism on 2D panoramic radiographs is assessed readily on radiographs of typodonts or dried skull phantoms. This approach not only allows for precise manipulation of tooth angulation within the arch, but also (1) allows for manipulating how specific root features (dilacerations, resorbed areas, multiple roots) are oriented relative to the X-ray beam, (2) enables the measurement of root length and width, and (3) permits the rotation of the phantoms within the X-ray unit to assess the effect of head tilt on geometric distortion. Using this approach, approximately 73% of the root angulations measured from conventional 2D panoramic radiographs of typodonts are inaccurate (Owens & Johal, 2008). Whether the inaccuracy skews larger or smaller than the actual angulation depends on which teeth are being evaluated and greatly affects the perceived parallelism. The roots of all mandibular teeth appear tipped more mesially on the radiograph than they actually are (McKee et al., 2002; Garcia-Figueroa et al., 2008; Owens & Johal, 2008). In the maxillary arch, roots of the anterior teeth also project as tipped more mesially, but roots of the posterior teeth appear distally tipped relative to their true angulations. As a result, maxillary canines and first premolars that are parallel to each other appear excessively divergent on conventional 2D panoramic films. Orthodontic correction of this apparent divergence would result in roots that are approximated too closely. In fact, because the canine angulation is distorted in particular, the American Board of Orthodontics explicitly states that canine root angulations are not to be scored when assessing root parallelism on panoramic radiographs. Thus, clinicians must be aware that root positions are distorted significantly on conventional 2D panoramic radiographs (Lucchesi et al., 1988).
Given CBCT’s 3D rendering capacity, it should surprise no one that root angulation measurements taken from CBCT images are significantly more accurate than measurements taken from conventional 2D radiographs. While statistically significant angulation error was measured for 16 of 28 typodont teeth on a CBCT image relative to the true angulations, the errors are less than comparable angulation errors measured on 2D radiographs (Van Elslande et al., 2010). Part of the measurement error in this and all radiographic studies is the result of human error in identifying and connecting landmarks to make linear or angular measurements. To help overcome this, typodonts also have been used to develop a computer algorithm that improves the accuracy of angular measurements on CBCT images (Tong et al., 2012a). When compared with the gold standard of CMM-generated angular measurements, the algorithm accurately measured root angulation on 23 of 28 teeth on CBCT images (Figure 15.3). While this methodology currently is not available to clinicians, this study establishes the groundwork for computerized analysis of root angulation that should eliminate or at least greatly reduce measurement inaccuracies.
An important point must be made concerning the measurement error in these typodont-based CBCT studies. While angular measurements taken from CBCT radiographs of typodont teeth are more accurate than angular measurements taken from 2D radiographs, the CBCT-generated measurements are not always accurate. In fact, the angles measured from the CBCT images were different statistically from the actual angles measured on the CMM in the studies by Tong and associates (2012a) and Van Elslande and colleagues (2010). However, most of the differences were not considered to be significant clinically because they were within ±2.5° of the true angulation; indeed, only measurements of the maxillary lateral incisor angles appear to be the most consistently erroneous in these studies. Why these teeth in particular differ from the actual measurement is not clear, although it is possible that differences in the buccolingual angulation or torque may contribute to these variances (Garcia-Figueroa et al., 2008; Van Elslande et al., 2010).
Accurate angular measurements are important clinically because root torque rarely is a treatment plan when a tooth’s mesiodistal angulation is within ±2.5° of its standard reference plane as measured on conventional 2D radiograph (Sämfors & Welander, 1974; Tronje et al., 1981; McKee et al., 2001; Stramotas et al., 2002; Hardy et al., 2009). However, if the mesiodistal angulation exceeds ±2.5° from normal in 2D radiography, then torquing of the roots often is factored into the treatment plan toward correcting this discrepancy. Thus, in a direct comparison of 2D panoramic and CBCT radiographs, root torque would be planned unnecessarily as treatment for 34% of the maxillary teeth and 38% of the mandibular teeth for which the tooth angulation exceeds ±2.5° of normal on the 2D panoramic, but within ±2.5° of normal on the CBCT radiographs (Bouwens et al., 2011). In fact, consistent with the studies of Tong and colleagues (2012a) and Van Elslande and coworkers (2010), Bouwens and associates (2011) suggested that because the lateral incisor angulations on 2D and 3D radiographs differ so significantly from the actual angle, the American Board of Orthodontics should consider eliminating the radiographic scoring of lateral incisor angulations from finished cases, as is done for canine angulations.
Similar to findings on typodonts, angles measured from CBCT images of patients differ significantly from those measured on 2D panoramic radiographs. Emphasizing the need to assess root parallelism accurately at the end of orthodontics treatment, contact between adjacent roots was assessed on CBCT and 2D panoramic radiographs (Leuzinger et al., 2010). Of the 235 sites examined, root contact was detected in 47 sites on 2D panoramic radiographs. When those same 235 sites were examined by CBCT, only five sites had actual root-to-root contact, giving an 89% false-positive rate on 2D images. This raises the possibility that a clinician who diagnoses root contacts on a 2D panoramic radiograph taken near the end of treatment may continue treatment unnecessarily in trying to address a perceived root proximity or contact.
Using an intriguing study design, Peck and coworkers (2007) assessed angular measurements on five subjects who wore splints studded with radiopaque markers at the occlusal plane and root surfaces. Conventional 2D panoramic and CBCT radiographs were taken of each subject wearing his or her splint. Linear and angular measurements were made on each radiograph and compared with dental casts for each subject. CBCT-derived root angulation measurements consistently were more accurate than those taken from 2D panoramic radiographs. Similar to findings of Bouwens and associates (2011), there are significant differences (75% of the time) between tooth angulation measurements taken from CBCTs and 2D radiographs. While it remains to be determined conclusively if head position adversely affects the accuracy of angular measurements on CBCT images (El-Beialy et al., 2011; Frongia et al., 2012), it is clear that 2D radiographs cannot be considered a reliable medium for assessing root angulation in patients.
Another clinical application of CBCT not only demonstrates the accuracy of 3D imaging for measuring root angulation, but also highlights the ability of 3D imaging to capture angulations that 2D imaging simply cannot. Mandibular canine and first molar root buccolingual angulations were assessed on CBCT radiographs taken on Class I and II subjects prior to orthodontics treatment (Shewinvanakitkul et al., 2011). Mandibular canine angulation had a mean of 98° relative to a line connecting the inferior border of the right and left mandible in the coronal plane and did not differ between the Angle groups. However, the buccolingual angulation of the first molar was higher in Class I patients (76°) compared with Class II patients (74°). Whether a 2° difference in first molar buccolingual angulation between Class I and Class II is relevant clinically depends on whether buccolingual crown torque is considered in the treatment plan. This decision, in turn, may depend on the boundary conditions around the roots of these teeth for which CBCT assessment may improve diagnosis and treatment planning decisions further (see Chapter 14).
While analysis of buccolingual angulation currently is not a standard part of the orthodontics evaluation, either before or after treatment, there are cases where this knowledge would prove invaluable. Decision making in borderline cases where orthodontics treatment alone is a potential treatment option without extractions, camouflage, or surgery certainly would be improved by knowing the amount of buccal or lingual tipping of the teeth that the alveolar bone may tolerate or to which it may adapt. Since the only way to obtain this information is by analyzing relative buccolingual dimensions of teeth and bone on CBCT radiographs, clinicians could justify taking the radiographs in these cases if it helps them decide whether or not extractions or surgery are necessary. This topic is covered in more detail in Chapter 14.
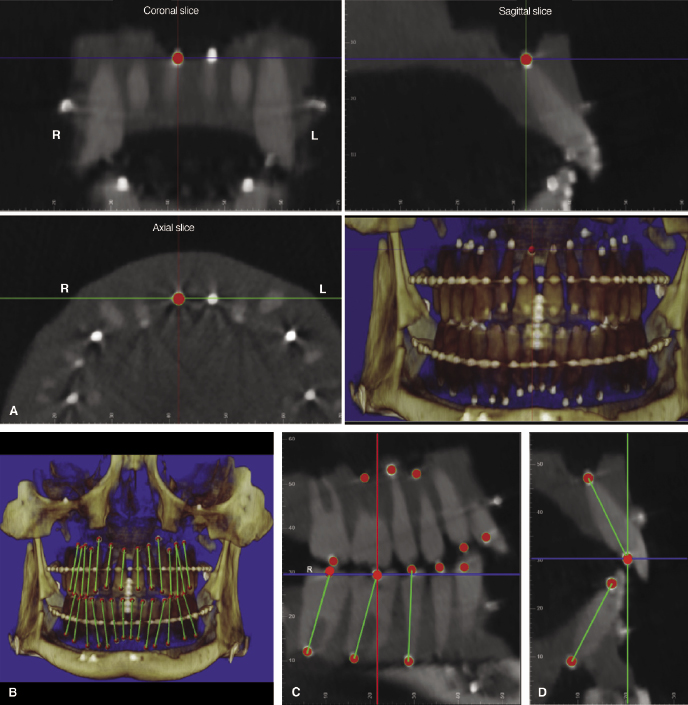
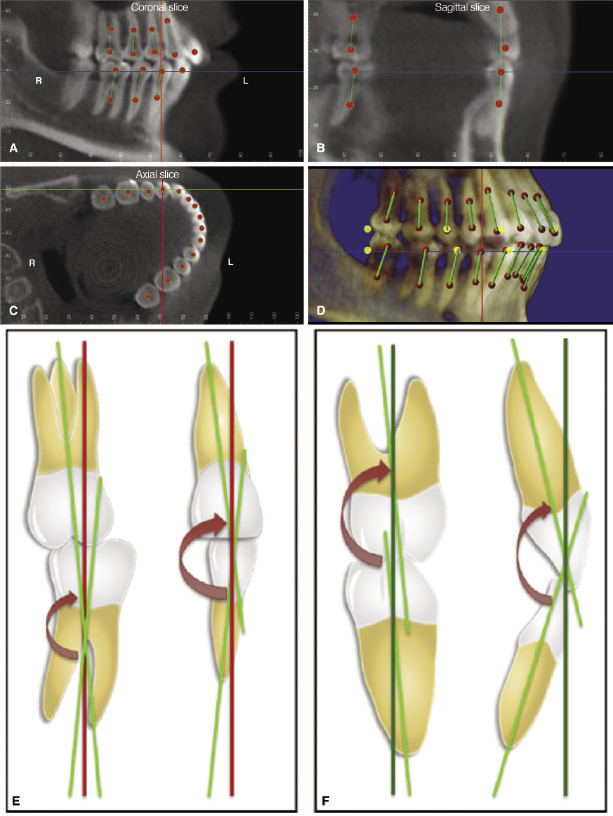
In an elegant example of translational research, Tong and associates applied their CBCT-based approach to tooth angulation measurements on a typodont (2012a) to human subjects (2012b). Using root apex and mid-occlusal markers to define the tooth’s long axis, the whole tooth angulation relative to the occlusal plane in the CBCT images could be determined (Figure 15.4). Equally important, this approach allows interdental angulations to be determined from both the mesiodistal and faciolingual perspectives. These data offer an exciting opportunity to introduce individualized treatment planning objectives for our orthodontics patients. If we are to believe that Andrews’s six keys to ideal occlusion (1972) are correct, then it should follow that tooth angulations are most stable in the context of strong supporting alveolar boundary conditions (see Chapter 14). By collecting and combining angulation data with alveolar boundary condition data from long-term follow-up studies of occlusal stability in orthodontics patients, we could define individualized ideal tooth positions for every patient, based on his or her pre-treatment dentoalveolar relationships.
In closing this section on the accuracy of angular measurements taken from 2D and 3D radiographs, one last caveat is offered. As CBCT studies proliferate, readers wanting to compare data from CBCT studies with each other and with data from conventional 2D radiographic studies face a potential danger in doing so if they fail to recognize the importance of the reference lines used to make the angular measurements. In general, lines through the long axis of the tooth and a clearly defined reproducible vertical or horizontal plane form the angle of interest. Unfortunately, the vertical or horizontal reference planes rarely are the same across studies. This has important implications if cross-study comparisons or meta-analyses are to be conducted. For example, the maxillary right lateral incisor in mixed dentition subjects (mean age 8.6–8.9 years old) is tipped distally at 88.4° relative to the right posterior occlusal plane on the conventional 2D panoramic image, but tipped mesially at 16.8° relative to the sagittal plane when viewed in the coronal CBCT image (Jesuino et al., 2010; Baratieri et al., 2011). There is no way for the reader to determine if these two measurements are equivalent because the reference lines used in each study generate unrelated angles. Moreover, there is no way for the reader to calculate or measure the corresponding angle directly in each study. This is a significant issue because it prevents us from developing a cohesive picture of root positioning. In all likelihood, this problem will be resolved at least partially when standardized 3D CBCT analyses are developed and researchers begin publishing data in which measurements are made relative to accepted, well-defined, and reproducible reference planes.
External Apical Root Resorption in Orthodontics Patients
External apical root resorption (EARR) is a type of pathologic root resorption unique to orthodontically moved teeth. As Kemple stated and as every orthodontist knows, there is another reason for turning our focus to EARR:
When an orthodontist discovers a beautifully developed permanent tooth, strong and of good structure, becoming very loose—apparently almost ready to drop out of its socket—he is suddenly seized with something very akin to heart-failure. (Ottolengui, 1914)
EARR is the most common sequelae of orthodontic treatment (Harris, 2000). Irreversible and unpredictable, EARR occurs in 60–95% of orthodontics patients; in 2–5% of EARR cases, it is severe enough to diminish the prognosis of effected teeth (Spurrier et al., 1990; Baumrind et al., 1996; Kurol et al., 1996; Taithongchai et al., 1996). Conventional 2D periapical or panoramic radiographs taken within the first year of orthodontic treatment usually are the first time the orthodontist becomes aware that a patient is at risk for severe resorption. It has been proposed that if moderate EARR is detected on progress radiographs taken within the first year of orthodontic treatment, then severe EARR is likely if treatment is continued (Artun et al., 2005, 2009; Smale et al., 2005). Temporarily stopping orthodontic treatment for 2–3 months followed by treatment using the lightest forces possible appears to be the best approach to managing these cases (Weltman et al., 2010).
EARR can range from mild (less than 1 mm on any tooth regardless of initial root length) to severe (more than 20% of initial root length; Kokich, 2008). Given the inability of conventional 2D radiographs to capture 3D anatomy accurately, it should not be surprising that root resorption cannot be measured accurately from 2D radiographs. EARR is diagnosed correctly only 44% of the time from digitized 2D periapical radiographs (Dudic et al., 2008), and 2D panoramic radiographs overestimate the magnitude of EARR by 20% or more (Sameshima & Asgarifar, 2001). CBCT captures root anatomy in all three planes of space, and researchers have invested considerable time and effort validating the accuracy of root resorption measurements on the 3D images.
Accuracy of Root Defects Measurement in 2D and 3D Radiographs
Simulated root resorption is the approach used most often in radiographic accuracy studies (Lund et al., 2010; Alqerban et al., 2011a, 2011b; Durack et al., 2011; Kumar et al., 2011; Bernardes et al., 2012; de Azevedo Vaz et al., 2012; Neves et al., 2012a, 2012b; Ponder et al., 2012; Ren et al., 2013). Resorption defects of varying sizes, shapes, and locations are placed on typodont or cadaver tooth roots with a dental bur. Compared with 2D radiographs, CBCT radiographs consistently generate more accurate images of defects ranging in size from 0.15 to 3.6 mm (Alqerban et al., 2009, 2011b; Durack et al., 2011; Ren et al., 2013). Interestingly, one group did not find any difference between 2D and 3D imaging for detecting root resorption in vitro due to regression toward the mean as examiners overestimated defect size on CBCT images and underestimated defect size on periapical images (Kumar et al., 2011).
One in vivo study diagnosing post-orthodontic root resorption on conventional 2D panoramic radiographs compared with CBCT radiographs supports the conclusion that panoramic radiographs underestimate EARR (Dudic et al., 2009). In this study, orthodontics patients were referred for CBCT imaging to assess root parallelism that was not visible clearly on the 2D panoramic radiographs. EARR was diagnosed on 43% of all teeth on the panoramic radiographs and 69% of all teeth on the CBCT radiographs. Similarly, EARR of the maxillary incisors, which are the teeth most likely to undergo EARR (Segal et al., 2004, and references therein), was not diagnosed 20% of the time on the panoramic radiographs and 14% of the time on the CBCT radiographs. Moreover, three cases of severe EARR were diagnosed on the CBCT images, but not on the panoramic radiographs. Overall, it is clear that CBCT is better significantly than conventional 2D radiographs for diagnosing EARR.
Regardless of the radiographic modality being used, optimizing the X-ray machine settings is critical for generating diagnostically acceptable radiographs. CBCT machines have variable voxel sizes that usually range from 0.2 to 0.4 mm3 in size. Clinicians considering using CBCT to assess EARR should select a small voxel size to improve EARR diagnostic sensitivity, specificity, and accuracy (Liedke et al., 2009; Neves et al., 2012b). In addition to small voxel size, limited volume exposure is an option for obtaining high-resolution radiographs at a relatively low radiation dose (Durack et al., 2011). The easiest way to do this is to use the smallest sensor to image the region of suspected localized root resorption, rather than the larger sensors that image the whole craniofacial complex. Another limited volume exposure option being tested is to collect images from a 180° rather than a 360° sweep of the skull. Images collected from the shorter scan are equally as accurate as the longer scan for diagnosing periapical bone loss in vitro (Lennon et al., 2011) and may guide the development of targeted imaging protocols for suspected EARR in orthodontics patients. Finally, software development to improve the resolution of post-capture CBCT data is an active area of research (de Azevedo Vaz et al., 2012; see also Chapter 5) that could enhance the capabilities of CBCT further in diagnosis of EARR.
Potential Risk Factors for Orthodontically-Induced External Apical Root Resorption Based on 2D and 3D Data
Despite decades of research, consensus on the predisposing risk factors of EARR has not been reached. While it is agreed that EARR results from the combined influences of biology (patient susceptibility) and mechanics or orthodontic treatment (Weltman et al., 2010), and abundant data on potential risk factors for EARR are available, much of that data are contradictory (Table 15.1). This is not surprising, as most of the existing data were collected from conventional 2D radiographs. Ironically, the amount of contradictory data from studies based on 2D radiographs supports the conclusion that these radiographs are inappropriate for assessing risk factors for EARR. This is not a trivial problem. EARR is an irreversible process that decreases the long-term prognosis of a tooth if rigorous effort is not expended to maintain a healthy periodontal status for the tooth or if the tooth is subjected to trauma, whether extraoral (e.g., blunt force) or intraoral (e.g., fremitus; Kokich, 2008). Yet the need for radiographic evidence of EARR cannot be overstated, as early detection of minor EARR (within the first 6 months of orthodontic treatment) is correlated highly with severe EARR at the end of treatment (Levander et al., 1998a; Artun et al., 2005; Weltman et al., 2010). The conflicting radiographic data on EARR risk factors also highlight the need for combining imaging data with genetic and molecular biological data to identify EARR risk factors definitively in orthodontics patients.
Table 15.1 Conventional 2D radiograph and CBCT studies investigating potential treatment- and patient-related risk factors associated with EARR in orthodontics patients.
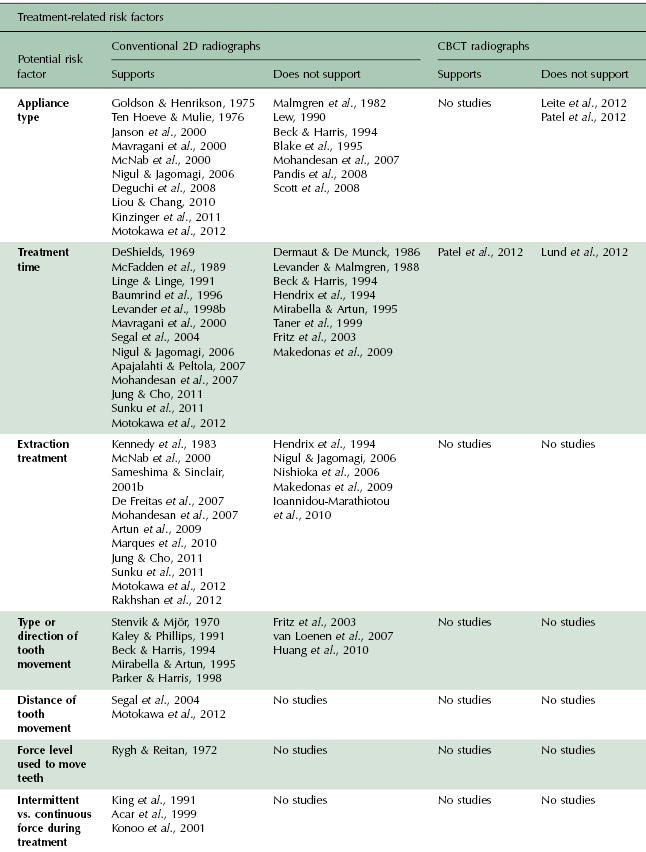
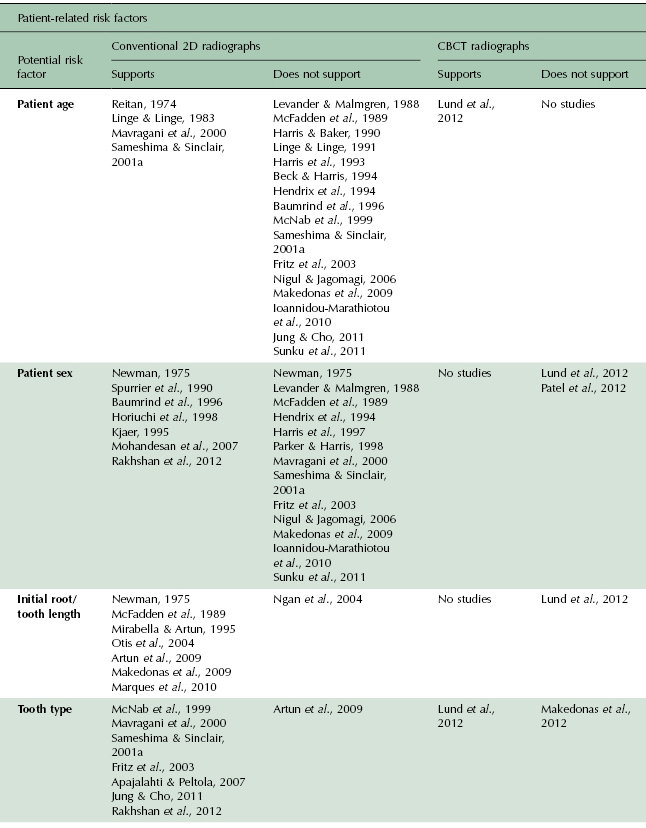
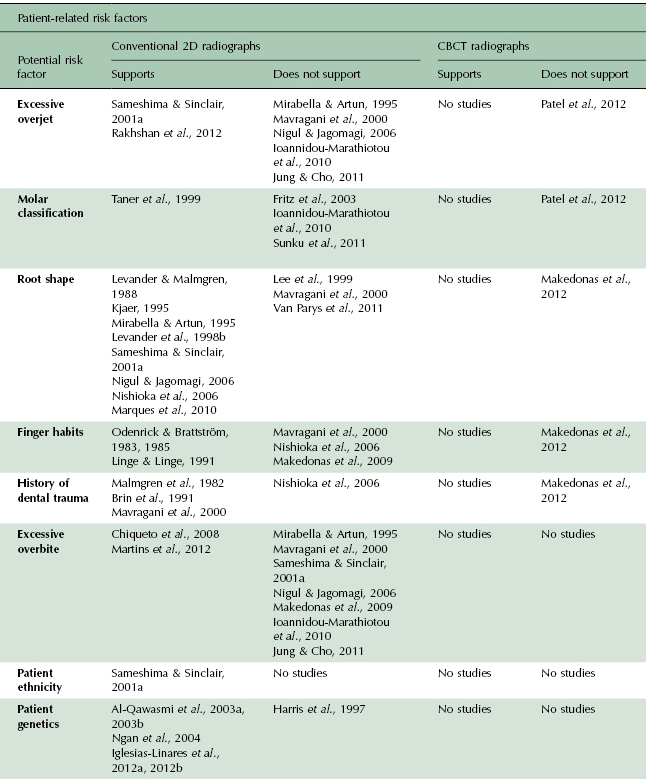
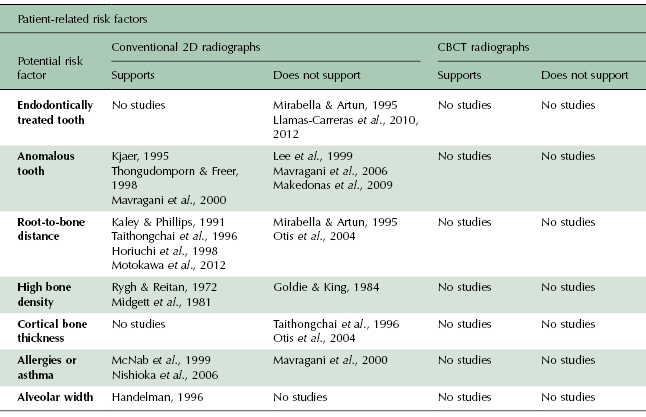
3D imaging certainly offers significant power to measure changes accurately in root length during orthodontic treatment. Because of its relative newness to the field, however, few CBCT-based studies on orthodontically induced EARR are available. Such studies serve several important functions. First, they help to verify the accuracy of CBCT imaging in making and analyzing the submillimeter measurements common in subject-based EARR studies. Second, they help establish protocols for orienting and superimposing CBCT images to ensure reproducibility of these studies. Finally, they provide insight into selected risk factors for orthodontically-induced EARR.
As shown in Table 15.1, relatively few CBCT-based studies have been performed to evaluate EARR risk factors in orthodontics patients. Of all the potential risk factors, CBCT-based studies support patient age, tooth type, excessive overjet, and molar classification as potential risk factors, although, intriguingly, the 2D studies do not support excessive overjet or molar classification as risk factors. Conversely, CBCT-based studies do not support appliance type, patient sex, initial root/tooth length/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


