14 Use of Injectable Fillers in Cosmetic Facial Surgery
Over the millennia, various substances have been injected into the face, including wax, silicone, and animal products1,2 (Table 14-1). Contemporary cosmetic facial surgery includes many options to augment lips, folds, and wrinkles. For decades, bovine collagen has been the gold standard for facial filler augmentation in the United States.3 Our European, Canadian, and Australian neighbors have been more proactive in the use of various fillers4; this technology is just reaching our shores and is responsible in part for the enormous media coverage of injectable filler substances.
| Year | Developer | Description |
|---|---|---|
| 1893 | Neuberg | First to use autologous fat for tissue augmentation |
| 1899 | Gersvny | First to use bioinjectable paraffin for cosmetic deformities |
| 1910 | Lexor | First to use large block grafts to treat malar depression |
| 1911 | Burnings | First to describe transfer of free fat employing syringe technique |
| 1953 | Baronders | Use of liquid silicone in medicine |
| 1959 | Peer | Reported 50% survival of syringe-aspirated transplanted fat for 1 year |
| 1976 | Fischer | Cellulosuctiontome extraction of fat |
| 1978 | Illouz | Liposuction as fat source |
| 1981 | FDA approval of Zyderm 1 | |
| 1986 | Fornier | Microliposuction |
| 2003 | FDA approval of Restylane, the first nonanimal hyaluronic acid filler available in the United States | |
| 2003 | FDA approval of CosmoPlast and CosmoDerm | |
| 2004 | FDA approval of Sculptra for facial lipoatrophy | |
| 2006 | FDA approval of Juvederm | |
| 2006 | FDA approval of Artefill | |
| 2006 | FDA Approval of Radiesse | |
| 2007 | FDA Approval of Perlane | |
| 2008 | FDA Approval of Evolence |
* A brief history of fillers. More activity has progressed at the lower end of the chart over a 7-year period than in the entire previous century.
Recent Historical Overview of Facial Fillers Available in the United States
The marketing release of Restylane brought an onslaught of media attention that boosted interest among aging baby boomers. It changed the paradigm in this country for injectable fillers for numerous reasons. First, it is a nonanimal product synthesized from bacteria. Hyaluronic acid is a highly hydrophilic polysaccharide found in all living cells; it attracts and binds more than 1000 times its weight in water and is chemically, physically, and biologically similar in all species.4 There is no reason for allergy testing, one of the biggest drawbacks of bovine collagen products. Additionally, continental outbreaks of swine flu, avian flu, and mad cow disease made fillers derived from animal sources unattractive. Second, studies showed that HA fillers last longer than Zyplast. The longevity of Zyplast has long been a problem for patients and injectors. Although the product was easy to use and produced acceptable results, it lasted only several months in most patients, whereas some studies show that HA fillers can last much longer.5,6 One of the reasons for the extended longevity with the hyalurons (HA fillers) is a process called isovolumic degradation. Normally, collagen fillers are simply phagocytized and degraded, which causes decrease in volume, but in this process, water is drawn into the hydrophilic molecule as the filler degrades. The filler volume is retained longer as more water is continually drawn into the molecule.7
Multiple studies have shown HA to be a safe and effective facial filler.8,9 The Medicis Pharmaceuticals (Scottsdale, AZ) and Allergan HA products are available in various particle sizes. These HA fillers come in larger particle sizes for less viscosity and more robust consistencies.
On February 28, 2003, the FDA’s General and Plastic Surgery Devices Advisory Panel recommended that Artefill be approved, with conditions for marketing in the United States. Artefill is expected to become the first permanent aesthetic injectable implant to gain FDA approval. It is a combination of homogeneous precision-filtered microspheres suspended in a solution of purified collagen gel and 0.3% lidocaine to alleviate discomfort during injection. Artefill is designed with dual action to correct facial wrinkles: 20% precision-filtered microspheres made from polymethylmethacrylate (PMMA) and 80% purified bovine collagen. All microspheres have a defined size of 30 to 50 microns in diameter and have a smooth, round surface. Aesthetic results are visible immediately after injection. PMMA is not taken up by scavenger cells (macrophages) and cannot be degraded by enzymes. Thus, the microspheres will remain intact beneath the creases, providing a permanent structure to support the wrinkle and prevent further wrinkling. As with all products using bovine collagen, a skin sensitivity test must be performed prior to use. Artes Medical declared bankruptcy in 2009 and the product was purchased by Seneva Medical and it is back on the market at the time of this writing. Oral and maxillofacial surgeons have used hydroxyapatite products for augmentation for the past 20 years. Radiesse (BioForm, Franksville, Wisconsin) is an injectable filler that consists of hydroxyapatite microspheres in a soluble gel vehicle10 (Figure 14-1). The author uses Radiesse when requested by patients, primarily in the nasolabial folds. The flow properties are different from other fillers. The most noticeable property of Radiesse is that a little product goes a long way. Because this product is hydroxyapatite based, the longevity is increased. For this reason, overfill or asymmetry can be a problem because it persists for a long time. The author does not recommend this product for the novice injector. Because Radiesse is opaque, lip injection is visible on radiographs; patients and their dentists should be made aware of this (Figure 14-2).
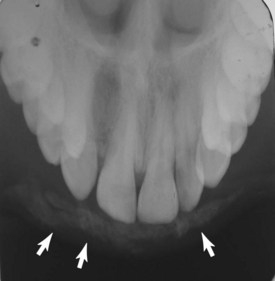
FIGURE 14-2 Radiesse is radiopaque and sometimes visible on radiographs. The patient should be aware of this situation.
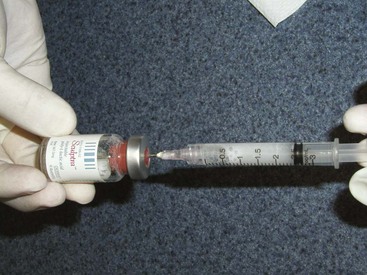
Finally, a plethora of new products that have been used in other countries are knocking at the doors of the FDA. In 2004, Sculptra (Advantis Pharmaceuticals, Bridgewater, NJ), which has been used abroad as Newfil, was FDA approved for the treatment of human immunodeficiency virus (HIV)-associated facial lipoatrophy. HIV patients are living longer and healthier due to new antiretroviral drugs, but a side effect of these medications is lipoatrophy of the temporal and facial regions. This stigmata makes HIV-positive patients stand out and has many negative social implications. Although this condition is amenable to treatment with multiple fillers, Sculptra has become a popular option. Sculptra is an injectable implant that contains microparticles of poly-l-lactic acid, a biocompatible, biodegradable, synthetic polymer from the alpha hydroxy acid family. Sculptra is reconstituted prior to use by the addition of sterile water for injection to form a sterile nonpyrogenic suspension (Figure 14-3). Since a large part of my practice consists of facial implants, I have not used this filler much; however, many colleagues sing its praises, especially when used in the midface and temporal regions for volume restoration.
Autologous fat is another common filler technique and will also be discussed later in this chapter.11,12
Evolence is the newest non-HA filler to hit the market and was FDA approved in 2008 for filling nasolabial folds. Evolence has been most popular in Israel and has been used with success for over a decade, since it is a medical treatment considered Kosher. This filler consists of porcine collagen with proprietary cross-linking. The manufacturing process removes many of the immunogenic substances, and therefore no allergy testing is required, which is different from previous collagen fillers. Porcine collagen is very close to human tissue and is used in heart valves and skin grafts. Since this filler is a collagen derivative, it has hemostatic properties that are said to reduce bruising. In addition, the substance is not as hydrophilic as HA fillers and produces less swelling. At the time of this writing, Johnson and Johnson has stopped the production and marketing of Evolence in the United States, but like other fillers that have been discontinued, I anticipate another company reintroducing Evolence in the near future. Older surgeons have seen a paradigm shift from having a single filler product to having many choices, and this will increase yearly as filler science continues. In my early days of practice, I dictated the filler choice, but today’s cosmetic consumers are much more informed and frequently request the type or brand of filler they prefer. The contemporary filler injector is a “bartender” of sorts and must have expertise in all commonly available injectable fillers (Figure 14-4). With the older, faster-absorbing fillers, overcorrection was a necessity, but with the newer fillers, the what-you-see-is-what-you-get technique is employed.
Tissue Deposition of Injectable Fillers
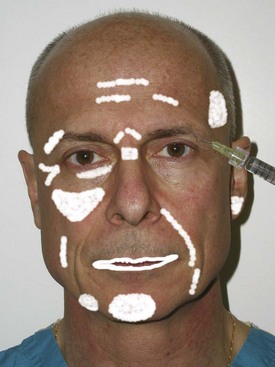
It is far more important how the filler is used than which filler is used. A competent injector can achieve aesthetic results from any filler if he or she knows how to use it and where to put it. Conversely, an inexperienced injector can use a premium filler and get poor results. The key to success with all fillers is correct placement in the skin, and various anatomic sites have specific injection techniques. Figure 14-5 shows common areas of filler injection.
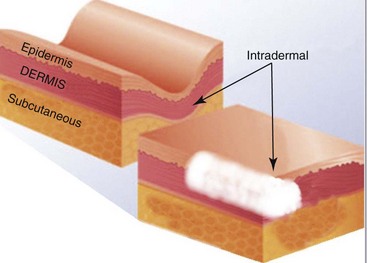
Most fillers are specifically designed to be placed at a certain level (Figure 14-6). The exact level of filler placement is a debatable subject. Many fillers say their intended target is the “dermis,” and some injectors describe injecting in the mid or deep dermis. Obviously this is a histologic determination, and in reality, the filler needs to be placed where its most optimum action can be exerted, including the dermis and subcutaneous planes. There is no doubt that this varies from patient to patient and is affected by skin thickness, region to be injected, amount of aging, and the specific filler composition. There are some general rules that make sense and can serve as guidelines to tissue placement. The less viscous fillers with smaller particle sizes are intended for more superficial dermal placement. The medium-particle fillers are meant for the mid-dermis, and the more robust or particulate fillers are intended for deep dermal or subcutaneous placement. Again, an experienced injector can push these boundaries. Placing viscous or particulate filler too superficially may produce contour irregularities or be visible through the tissue. Conversely, placing a small-particle filler in the deep tissue planes can result in premature resorption. A common mistake of the novice injector is to place HA gel fillers too deeply in the nasolabial fold region. This produces inadequate augmentation and dissolves faster. There is a “sweet spot” on the skin where the placement of filler produces controlled augmentation, and that differs from patient to patient. Experienced injectors know where to put the filler for maximum result, and this is a learned skill guided more by feel and visual result than by science. In reality, histologic examination shows that the injected filler occupies multiple planes, including dermal and subcutaneous regions. Placing fillers such as silicone, Radiesse, fat, and Sculptra in the superficial dermis can produce contour irregularities. Placing fillers such as Restylane or Juvederm Ultra in the subcutaneous tissues is a less judicious choice than their more robust larger-particle counterparts.
Injectable Fillers: Treatment Considerations
Due to the marketing hype, some patients confuse fillers with Botox. In addition, some patients desire massive rhytid injection, but because they have such a large amount of wrinkling, this would not be practical. These patients are informed that they would be better treated with lifting or resurfacing procedures. In theory, fillers can be injected anywhere on the face; however, blindness has been reported with the periorbital injection of Zyplast and fat due to intravascular injection.13–15 This rare but devastating complication calls attention to the care that must be exercised in this area. The surgeon should always inject very superficially, use the smallest-gauge needle possible, and never use extreme plunger pressure on the syringe. Although the injection of fillers is simple, many problems can result in terms of patient expectations and satisfaction. The main consideration is to accurately explain what can be realistically expected as a treatment result. Showing patients a series of before-and-after images for specific anatomic areas is one way to provide a reasonable expectation. In addition, the injection of fillers should not be presented as a one-time procedure but as a sculpting treatment sequence to approach a result. Especially for HA fillers—which because of their hydrophilic properties cause immediate swelling in the lips—judging the endpoint and symmetry can be difficult (Figure 14-7).
Informed Consent Process
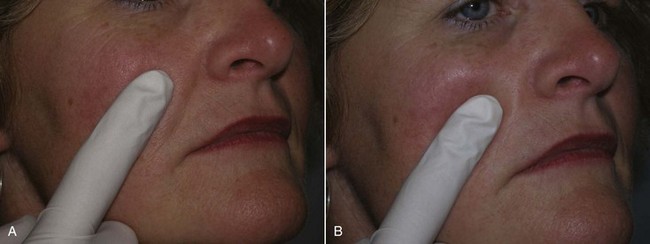
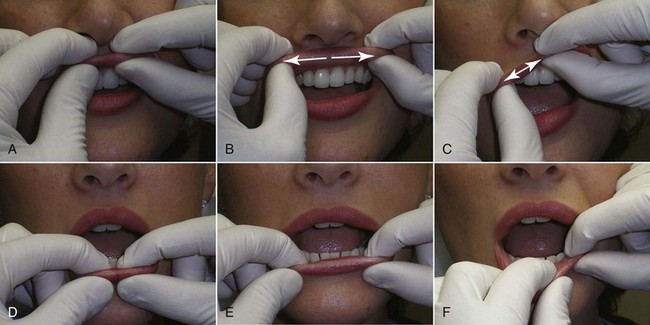
To give the patient an idea of anticipated result, I use the following method to demonstrate an approximate goal of nasolabial and lip injections. For the nasolabial folds, I place my index finger lateral to the patient’s nasolabial fold and gently push in on the skin. This elevates the nasolabial fold, simulating an augmentation (Figure 14-8). I let them know that the fold will improve but not disappear.
For the lips, I take both gloved index fingers and roll the upper lip up and the lower lip down. This allows increased vermilion show, similar to injecting filler, to increase pout and volume (Figure 14-9).
Injection Techniques
Having taught hundreds of injectors over the years, I open my lectures in jest by saying that if you can decorate a cake or caulk a bathtub, you can become proficient in filler techniques (Figure 14-10). There is actually some truth in this, since there is a distinct similarity of injection pressure and continual movement with the cake and caulk examples. Push the plunger too hard or fail to maintain a continuous motion, and you will get blobs instead of controlled lines. It is this combination of tactile pressure sensation and motion the novice injector needs to develop.
Diagnostic Decisions and Patient Expectations
Although it sounds painfully simple, the surgeon has to (1) ask the patient what changes they desire, (2) make an accurate diagnosis of the problems that exist, and (3) decide how to treat them (Figure 14-11). Patient input is extremely valuable. There have been times when I was about to augment the upper nasolabial fold, and the patient was not bothered by this region but expected lower-fold augmentation. The price of the treatment and the expected outcome warrant careful prefiller conversation.
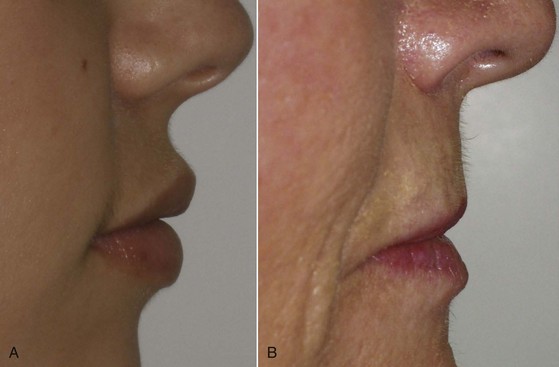
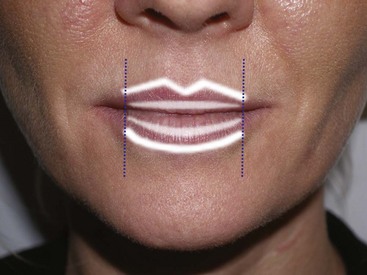
Treating young patients without significant photodamage is usually straightforward. They may simply need a touch of volume to plump the lips or some basic vermilion outline for definition. Treating the senescent lip, on the other hand, can be very challenging. The youthful lip is shorter, curvaceous, and has volume (Figure 14-12, A). The aging lip lengthens for numerous reasons, including volume loss from skin, muscle, and fat changes (see Figure 14-12, B).
Anesthetic Considerations
Some fillers contain inherent local anesthesia, but I strongly recommend using topical and local anesthetics when treating ultrasensitive areas like the lips and skin around the mouth. Local anesthetic technique for pain control is covered in Chapter 4. I truly believe that many injectors are simply lazy and do not invest the proper time and effort to make patients numb. Giving a patient a ball squeeze is not competent anesthesia. Undoubtedly, anesthesia care takes time and lengthens filler procedures, but this extra time spent will come back to the surgeon many times over in happy, painless patients and referrals. I like to supplement traditional anesthesia by having compassionate staff hold the patient’s hand (“handesthesia”) and conduct a relaxed, comforting conversation with the patient during the more painful portions of the injection procedure (“talkesthesia”).
Pharmacologic anesthesia should begin with an application of topical anesthesia on the skin if wrinkles or folds are to be treated. If the lips are to be treated, the inside and outside are covered with a thin coat of topical anesthetic, with care to include the upper and lower sulcus (Figure 14-13). I prefer 20% benzocaine, 6% lidocaine, and 4% tetracaine in a combination cream formulation. This is left in place for at least 5 minutes. The patient is then allowed to rinse their mouth; the anesthetic stimulates saliva and also will cause numbness in the pharynx, which is disconcerting for some patients (Figure 14-14).

FIGURE 14-13 The lip vermilion, intraoral mucosa, and sulcus are coated with a thin layer of topical anesthetic.
Although many surgeons employ local anesthetic blocks,16 I no longer use them, because they are more difficult and less dependable than infiltration techniques.17 Blocks are more technique sensitive, can be difficult in some patients, and will affect distant anatomy. Most patients do not like this. Using an infiltration I refer to as the “miniblock” technique, a series of injections is performed across the upper and/or lower sulcus. A 1-mL syringe with a 32-gauge needle is used with 2% lidocaine and 1 : 100,000 epinephrine (which can be electively omitted). Lidocaine in 0.2-mL aliquots is injected just above the upper sulcus (Figure 14-15) and just below the lower sulcus (Figure 14-16). This is generally performed in four to five areas from the canine tooth on one side to the canine tooth on the other side. The patient is then allowed 5 minutes for the anesthetic to take action. The local anesthetic will affect lip animation, which may become asymmetric, and this is another important reason for marking the patient prior to local anesthesia so landmarks are not lost. In addition, some of the wrinkles that existed with animation may not be visible if the lip is not moving normally (Figure 14-17).
Lip-Enhancement Techniques
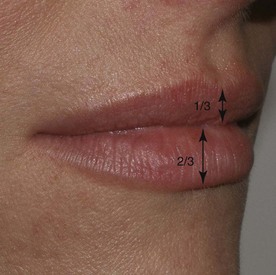
A successful injector is a student of lip form and function and needs to be cognizant of the differences between youthful and senescent lips. In youth, the upper lip constitutes about a third of the total lip volume, and the lower lip constitutes about two-thirds of the mass. This varies among patients and ethnicity (Figure 14-18). Another way of measuring the average ratio is 1 : 1.6 for the upper and lower lip, respectively. The youthful perioral region is defined by numerous anatomic components that undergo changes with aging. The astute injector is aware of normal lip volume, outline, philtrum, and philtral columns (Figure 14-19). Like any other body part, some patients exhibit outstandingly aesthetic lips. This patients may exhibit three distinct prominences or tubercles in the upper lip and two in the lower lip. On the upper lip, these natural “pillows” lie in the midline, one centrally and one on each lateral region. On the lower lip, the two prominent tubercles lie on each side of the midline. Some injectors strive to duplicate these prominent regions. My experience is that this looks good on some patients, but most patients feel that the discontinuous tubercles look less aesthetic than simply having full, contiguous lips.
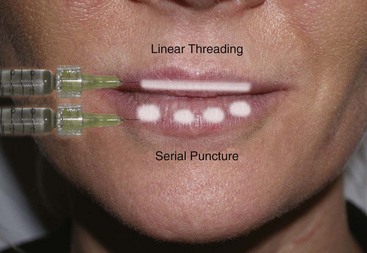
Every practitioner has his or her specific lip-enhancement techniques. The two most popular are linear threading and serial puncture (Figure 14-20). Linear threading involves inserting the needle and injecting the filler in a straight line while continuously moving in either a forward or backward direction. This process would be analogous to placing a line of toothpaste on one’s toothbrush, laying down a seam of calking, or decorating a cake. Although I personally inject while withdrawing, other injectors advocate injecting antegrade to push structures out of the way. The other injection method is known as the serial puncture technique. This involves placing small boluses of filler with multiple punctures along the lip or wrinkle. In reality, many instances call for a combination of both techniques.
Lip Outline
Each patient requires different filler techniques based upon their specific needs. Some patients (young and old) lack the specific outline of a “Cupid’s bow” or “white roll.” The Cupid’s bow of the upper lip is a lazy-M shape, and the corresponding border of the lower lip is curvilinear. In patients with well-defined lip borders, a pleasing light reflex is visible and contributes to maximum aesthetics. If a patient has adequate lip volume, they may only need border outline, but some patients need both volume and outline as well as vertical rhytid injection. Each patient is different (Figure 14-21).
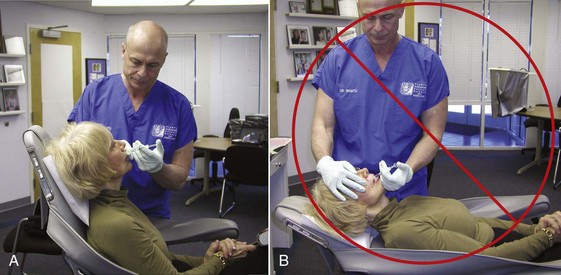
It is important to inject patients in a more upright position; gravity will distort a supine patient’s normal anatomy (Figure 14-22).
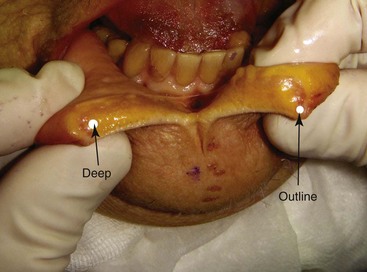
When injecting the lip borders, needle placement is critical. A potential space exists between the mucosa and orbicularis oris muscle, and this space is the target of border outline (Figure 14-23). The guide for novice injectors is both visual and tactile. When the needle is in the correct plane, the filler will visually flow both antegrade and retrograde. This can be seen and also palpated by the noninjecting hand. By pinching the border between the noninjecting thumb and index finger, the injector can feel the free-flowing filler as well as corral the filler to stay within the border (Figure 14-24).
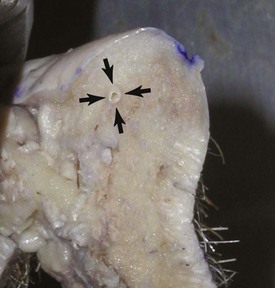
If the needle is in the correct plane (the described potential space), the filler will flow freely with minor syringe pressure. This is confirmed by observing the border being properly created. If the needle is too deep, no distinct outline is seen. If the needle is too superficial, the filler will not flow but instead “ball up,” and the syringe pressure will increase. In this case, the needle must be redirected into the proper potential space (Figure 14-25).
Creating the Vermilion Outline
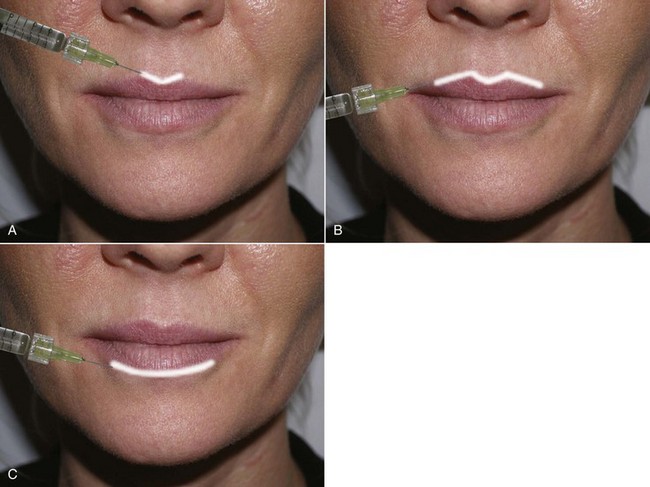
When augmenting the vermilion border for outline or white-roll enhancement, I begin with the central V of the Cupid’s bow. If the patient does not have a well-defined Cupid’s bow, I draw it on during preinjection marking as a guide for filling. Care is used to form crisp, angular contours in the downward legs of the lazy M in the area of the central lip (Figure 14-26, A).
The next step is to continue the vermilion outline augmentation laterally (see Figure 14-26, B). In the average patient, the white roll only needs to be augmented in the central one- to two-thirds of the upper lip that corresponds with the “pucker area.” I rarely carry this out to the lateral commissure. The needle is inserted all the way to the hub, and the filler is injected with even syringe pressure upon withdrawal. Most filler needles are  inch long, and the border is augmented at
inch long, and the border is augmented at  -inch intervals, taking care to not leave a gap between needle insertion points. The white roll is similarly created in the lower lip, which is more curvilinear than in the upper lip (see Figure 14-26, C).
-inch intervals, taking care to not leave a gap between needle insertion points. The white roll is similarly created in the lower lip, which is more curvilinear than in the upper lip (see Figure 14-26, C).
Increasing Deep Lip Volume
Although vermilion border augmentation is a powerful means of enhancing the lip, many patients have adequate outline and a defined white roll or Cupid’s bow and do not require outline. The most common presentation in my practice is the patient who presents with the desire for more lip volume. These patients request plumper, fuller, pouty, and more voluptuous lips. Many are younger and already have adequate vermilion border. These patients will benefit from deeper fill that will increase the general lip volume and pout. By augmenting the deeper portion of the lip, the actual lip will roll out and produce increased pout. The target for deep lip augmentation is basically the center of the lip. This is deep to the muscle and contains connective tissue, minor salivary glands, and fat (see Figure 14-24, “deep”).
For deep augmentation, the needle is inserted at the wet/dry line, deep into the central lip. The needle is inserted to the hub and slowly withdrawn while continuous, steady injection is performed. In this area, the goal is to produce a “tube” of filler for deep volume (Figure 14-27, A). As noted earlier, some injectors attempt to reproduce the prominent lip tubercles seen in some aesthetic lips, and instead of a continuous tube of filler, the tubercles are reconstructed, three in the upper lip and two in the lower lip (see Figure 14-27, B).
The center of the lip is generally a safe plane, because the labial artery lies at the posterior third of the lip (Figure 14-28). Generally a single syringe will treat the average patient requiring deeper volume and is appropriately split between the upper and lower lip based upon volumetric need.
A lumpy result with visible and palpable nodules of filler is frequently the result of not massaging the filler after injection. I strongly believe massaging the injected filler is a critical (and oftentimes overlooked) step in obtaining natural and aesthetic results. Most fillers have the consistency of soft gels or paste and when injected will not always be homogenous. Massaging the filler more evenly distributes and forms it and produces a smoother, more homogenous result (Figure 14-29). In addition, the injector can actually level out an area of excess by moving the filler through the tissues. Since there is friction between the skin and surgical gloves, massage is difficult and jerky without a lubricant. My assistant keeps a small bolus of petroleum jelly on the back of her glove during all filler injections, and I dab this and coat the lip and skin just prior to massage. Again, controlled massage is a critical part of filler injection.
Some injectors carry vermilion and deep volume injections all the way to the corner of the mouth, but I generally do not (Figure 14-30). In my opinion, one of the most common unnatural filler results is the “ducky” lip, due in part to an eversion of the lateral lip reminiscent of the familiar rubber duck bath toy, which is unfortunately visible on many female celebrities.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses