The ortho–endo interface
The nature of contemporary orthodontic management
The application of a continuous force to a tooth results in remodelling of alveolar bone, reorganization of the periodontal ligament and tooth movement. Orthodontic tooth movement is a complex process involving the coordinated activity of many cell types and numerous chemical mediators. The application of a continuous force to a tooth surface results in the development of areas of compression and tension within the periodontal ligament. Tipping forces, resulting from single point contact on a tooth surface, such as those resulting from springs on removable orthodontic appliances, produce loads that are greatest at the alveolar crest and root apex on diagonally opposing sides. Bodily tooth movement results from even compressive loads along one side of the periodontal ligament, resulting from a force couple from a fixed orthodontic appliance. The magnitude of the force delivered is important in determining the tissue response. Ideally, orthodontic forces should not exceed the capillary pressure within the periodontal ligament, in order to prevent ischaemia and tissue necrosis. The optimal force for tooth movement also depends on the type of tooth movement required and the root surface area of the teeth to be moved (Table 13.1); teeth with smaller roots require reduced forces for movement. The forces for intrusion are the lightest as the forces are concentrated at the root apices, which have a small surface area.
Table 13.1
Optimal force levels for different types of tooth movement
| Type of tooth movement | Force level (g) |
| Bodily movement | 60–120 |
| Tipping | 30–60 |
| Rotation | 30–60 |
| Extrusion | 30–60 |
| Intrusion | 10–20 |
Effect of orthodontic tooth movement on the pulp
Orthodontic tooth movement by virtue of direct interruption and interference with the neurovascular supply and, to a lesser extent, indirectly by tooth flexure, may affect the pulp physiology and status. Although the literature is relatively restricted, studies have been performed on animal and human teeth, which were thoroughly reviewed by Hamilton & Gutmann (1999). The nature, direction and extent of forces exerted (type of orthodontic technique and its execution) during tooth movement, their intermittent or continuous nature, the apical root maturity and age of patient may all influence pulp changes. A variety of outcome measures have been used to determine the effect of orthodontic tooth movement on the pulp, including effects at a tissue level (pulpal inflammation, pulpal degeneration, cellularity, fibrotic changes, predentine width, reparative dentine formation, pulpal space obliteration, Hertwig’s epithelial root sheath), cellular level (pulp cell metabolism and cell respiration rate, survival or degeneration of odontoblasts), vascular level (vascularity, blood flow, circulatory disturbances, angiogenesis), neural level (neuronal cell density, distribution of myelinated versus non-myelinated cells), molecular level (expression of various molecular factors including calcitonin-gene-related neuropeptide [CGRP], methionine encephalin, β-endorphin, substance P, neurokinin A, vasoactive intestinal polypeptide, neuropeptide Y) and clinical level (pulp response to pulp testing, signs and symptoms, discoloration, pulpitis, pulp necrosis).
Although the results were sometimes conflicting and contradictory, the overall findings suggest that orthodontic tooth movement can cause neurovascular disturbances, which result first in inflammatory and then degenerative changes in the pulp, particularly in teeth with mature root apices. The effects are likely to be mediated through variations in the expression of a variety of controlling molecular signalling systems, which would exert their effects at vascular, neural, metabolic, cellular, and tissue levels. The rate and pattern of dentinogenic activity may be altered or affected resulting in tertiary dentine and, rarely, even pulp obliteration (Fig. 13.1). The prevalence and severity of the effects may be affected by the magnitude, direction, continuous or intermittent nature and duration of forces exerted, as well as any previous history of pulpal stimulation, such as through caries, restorations, trauma or periodontal disease. Teeth with immature roots are likely to be less affected because of a richer, thicker and less constrained (apical foramen size) neurovascular bundle.
Clinically evident effects are generally minimal and may include altered sensations to stimuli, such as pulp tests, pulpitis, dentinal pain due to distortions caused by uneven cementing resin polymerization during bracket attachment, pulpal haemorrhage and pulp necrosis. Sensation originating from the pulp may be blended with or masked by those emerging from the stressed periodontal ligament.
Effect of orthodontic tooth movement on root resorption
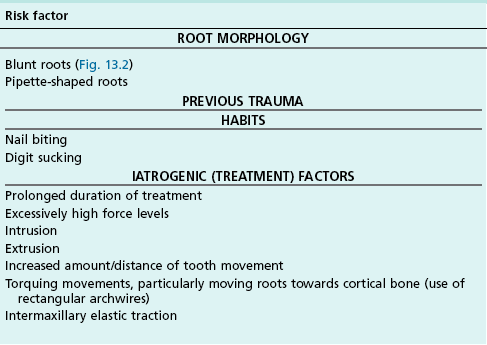
Resorption of roots associated with orthodontic tooth movement is well established and has a logical biological basis. Yet it does not occur consistently and may be affected by pulpal status, root morphology and nature and magnitude of orthodontic forces. Small amounts of root resorption, up to 1–2 mm, occur in the majority of patients undergoing fixed appliance orthodontic treatment, with little known long-term implications. Approximately 15% of patients may be affected by greater than 2.5 mm loss of root length, which may have long-term implications, particularly if it occurs in conjunction with periodontal bone loss. Potential risk factors for orthodontically-induced root resorption are listed in Table 13.2.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses