CHAPTER 14 Pain Management
DENTAL PAIN
Pain is sum total of responses (behavioral, emotional, motivational, psychological) to actual or impending tissue damage from noxious stimulus.
Anxiety Management
Anxiety is the feeling of apprehension and fear characterized by physical symptoms such as palpitations, sweating, feelings of stress. Anxiety keeps many people from receiving necessary dental treatment because of fear of pain or discomfort. Fear is excessive apprehension or anxiety. Understanding dental fear can help in selecting appropriate methods for alleviating patient discomfort. Anxiety and fear are common occurrences in the dental office and can be managed by a variety of techniques. Sometimes fear can become excessive and involve a phobia, which promotes inaction (failure to seek necessary dental treatment).
CLINICAL STUDY
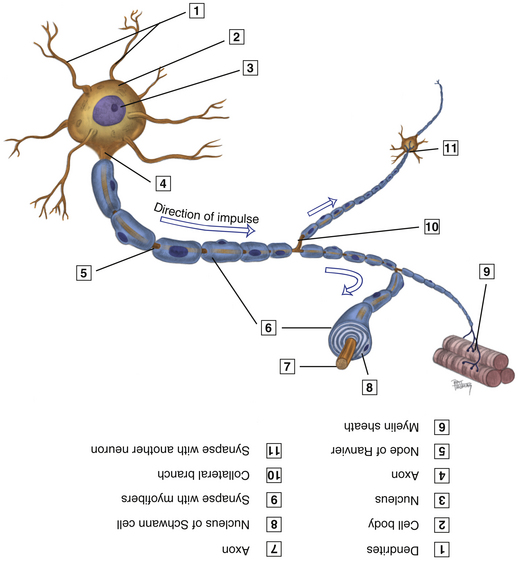
Sensory Innervation
LOCAL ANESTHESIA
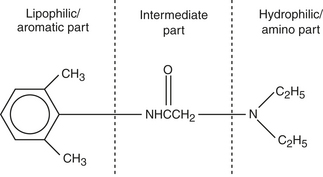
Pharmacology of Local Anesthetics and Vasoconstrictors
Local Anesthetic Agent Action
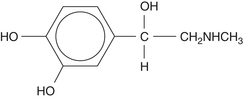
Vasoconstrictor Action
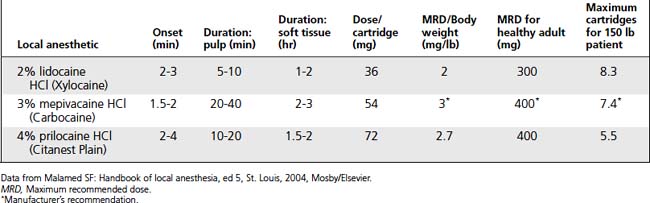
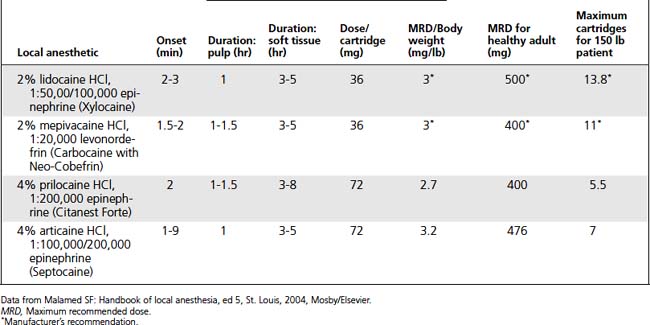
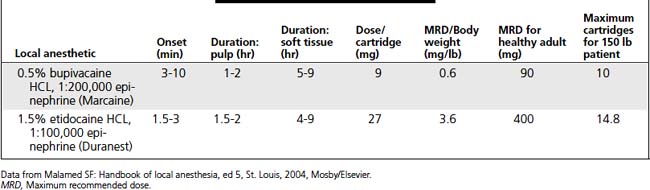
Dosage Calculations
Box 14-1 Local Anesthetic Agent Dose Calculations
QUESTIONS/ANSWERS
Box 14-2 Calculation of Vasoconstrictor Concentration
EXAMPLE: CALCULATION OF CONCENTRATION OF VASOCONSTRICTORS USING 1:100,000 EPINEPHRINE/ML OF SOLUTION
Local Anesthetic Agents and Vasoconstrictors
Topical Anesthetics
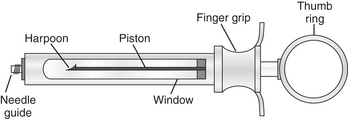
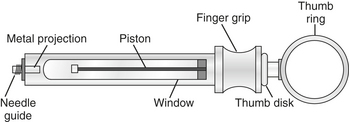
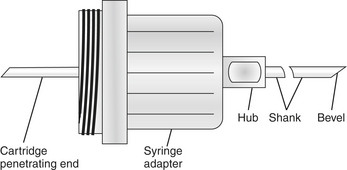
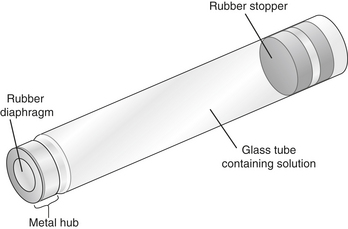
Local Anesthesia Armamentarium
| Anatomy anesthetized | Pulpal and soft tissue and nerve endings in area of injection |
|---|---|
| Needle gauge and length | 27-gauge; short, extra short, or ultra short or CLAD |
| Depth of penetration | Base of pocket until resistance is met |
| Landmarks | Pocket area, mesial of distal root |
| Site of penetration | Long axis of root on mesial or distal with bevel toward root |
| Deposition site | Base of pocket |
| Cartridge amount (1.8 mL/cartridge) | 0.2 mL |
| Complications | Pain |
| Advantages | Minimal dose required; no unnecessary structures anesthetized; works better with CLAD |
| Disadvantages | Leakage of anesthetic; difficult to deposit with nonpressure syringe; not with inflammation or primary teeth present |
∗ See manufacturer’s directions for use of pressure syringe (Ligmaject); dental hygienists may not be allowed to perform intraosseous injections in some states.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 •
•