Chapter 14 Materials used in temporization
Learning Objectives
From this chapter, the reader will:
• Understand why temporary restorations are required prior to the placement of the definitive (indirect) restoration
• Understand how the materials currently used for temporization achieve these aims
• Be aware of the range materials available for temporization
• Understand the indications and contraindications of materials used to temporize
• Have an increased appreciation of how to use the materials more effectively and to their best effect
• Know the names of currently available commercial products.
Introduction
It is widely acknowledged that good temporization is one of the most important factors in the fabrication of good quality, definitive indirect restorations. While there is some truth in the urban myth that temporary restorations should never be made too good as the patient may not return to have the definitive restorations fitted, it is essential that good-quality temporary cover is provided. Attention to detail during their construction facilitates the subsequent stages of the procedure, so producing a better definitive restoration. Temporary crowns protect the oral tissues and allow the patient to function while maintaining their appearance until the definitive restoration can be fitted. This chapter discusses the various materials used to provide temporary coverage.
Temporization: the construction of a temporary restoration, which restores form and function to the tooth while the definitive restoration is being made.
Definitive restoration: a restoration provided with the intention of being the long-term solution.
Indirect restoration: a dental restoration constructed outwith the mouth.
The Biological Importance of Good Temporization
• Some 30 000 to 70 000 dentinal tubules are opened per square millimetre during tooth preparation. The passage of oral bacteria into the freshly cut dentine must be minimized as this will cause pulpal inflammation, which manifests as sensitivity if the dentine is exposed to stimuli from the oral environment such as hot, cold and sweet.
• A well-fitting temporary restoration will prevent the gingival tissues from migrating over the preparation margins.
• It also allows the area to be cleaned more effectively and thus maintains a state of gingival health. This decreases the incidence of gingival inflammation and bleeding at the time of fitting the definitive restoration, which is particularly important when the restoration is being bonded using a hydrophobic resin-based composite material.
• A good provisional restoration will maintain occlusal and approximal contacts so preventing over-eruption and tilting of the prepared tooth, or adjacent and opposing teeth. This minimizes the need for occlusal or approximal adjustment of the definitive restoration at the fit appointment.
The Benefits of Quality Temporization
Benefits for the dentist
• The temporary restoration should be made prior to impression taking for the definitive restoration. When the occlusion has been verified and the temporary deemed satisfactory, the clinician can measure the width of the occlusal part of the restoration using an Iwannson gauge (Figure 14.1). This distance denotes the interocclusal clearance. If this is deemed to be insufficient, the dentist can adjust the preparation to create the required clearance prior to taking the working impression.
• In more complicated cases temporary restorations may provide the clinician with invaluable information for use in diagnosis and treatment planning, such as the construction of a new occlusal scheme or when an aesthetic case is being planned.
Benefits to the patient
The purpose of temporization may therefore be summarised as listed in Box 14.1.
Box 14.1 The purpose of temporization
• Maintenance of aesthetics and function
• Protection of prepared dentine from thermal and chemical trauma
• Maintenance of gingival contour and health
• Maintenance of good oral hygiene
• Maintenance of occlusal stability
• Prevention of drifting or tilting of adjacent teeth
• Allows the dentist to check that sufficient interocclusal reduction has been prepared
• Assists the clinician in diagnosis and treatment planning
• Assists the clinician in the construction of a new occlusal scheme
The Temporization ‘Balance’
A temporary restoration, be it an inlay, onlay, crown or bridge, must be effectively retained for the period of time between fitting and placement of the definitive restoration. Equally it must be removed easily at the fit appointment without damage to the preparation. A balance between good retention for this period and ease of removal must be established. Generally speaking, the most satisfactory combination is that of a well-prepared (mechanically retentive) preparation with a well-constructed temporary restoration grouted by a soft luting cement (see Chapter 12).
Types of Temporary Restoration
• An acrylic, such as heat- or self-cured polymethylmethacrylate
• A bis-GMA-based material such as resin composite
• Acrylic or ceramic bonded to metal – non-precious metal alloys (Chapter 21) are normally chosen on grounds of lower cost.
Acrylic: a generic term for chemical compounds that contain the acryl group derived from acrylic acid
Acrylate: the acrylate ion is the ion of acrylic acid and these are a group of materials that are derived from acrylic acid, that is, they are the salts and esters of acrylic acid. They contain vinyl groups, that is, two carbon atoms double bonded to each other, directly attached to the carbonyl carbon. Acrylates easily form polymers because the double bonds are very reactive. Acrylates and methacrylates (the salts and esters of methacrylic acid) are common monomers in polymer plastics, forming the acrylate polymers
Direct Temporary Restorations
Preformed crown forms
The first method of direct temporization involves the use of a preformed crown, which is trimmed to the margins of the preparation and refined using another material. The crown forms available are made of:
Crown forms used to construct tooth-coloured temporaries
Polycarbonate crown forms
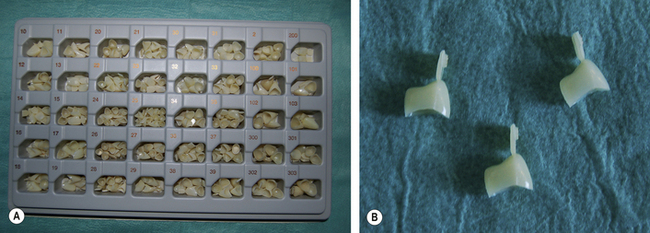
These temporary crown forms are made of a polymer with high impact resistance. This means they have sufficient strength to withstand occlusal forces. As the name implies the polycarbonates contain multiple carbonate groups. These may be linked by a variety of chemical groups, with the commonest one being bis-GMA. They are presented in various sizes in a tray (Figure 14.2).
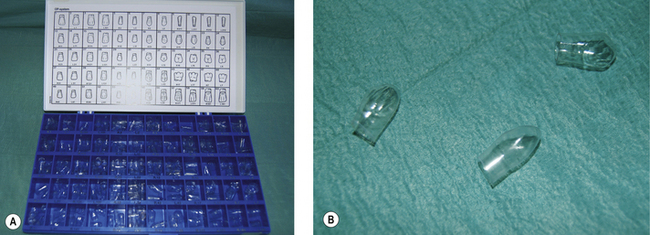
Cellulose acetate crown forms
These crown forms are transparent (Figure 14.3). They are used in essentially the same manner as polycarbonate crowns: they are trimmed to size using crown shears or scissors and then packed with another material matching in shade to the surrounding teeth. Some clinicians use resin-based composite for this purpose. These crown forms have the disadvantages that:
• They merely act as a matrix and so must be removed after their refining material has set
• When the cellulose crown form is removed, the thickness of the crown reduces (by about 0.2 mm). This may lead to instability in the occlusion and movement of adjacent teeth
• The refining material (often resin composite or compomer) can lock into undercuts, thus compromising removal of the crown and the patient’s ability to keep the (gingival) area clean.
Metal crown forms
Aluminium crown forms
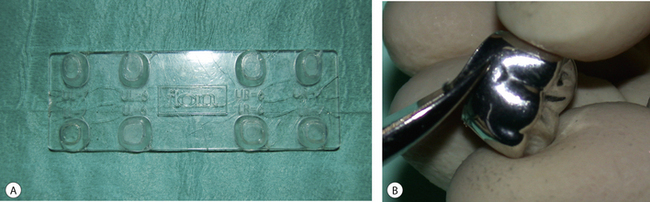
Aluminium crown forms have been used for many years as the material is easy to manipulate, and it is malleable and ductile. This makes their handling easy for the dentist as they can be bent and trimmed to shape easily. Aluminium crown forms can corrode with time as saliva can react with them. There is also a risk that if they are placed adjacent to a freshly packed amalgam or gold restoration, a galvanic cell may be established (see Chapter 6). Figure 14.4 shows some molar aluminium crown forms.
The crown form of the approximate size is selected. It is often expanded using the expander provided to fit over the prepared tooth (Figure 14.5A) and then cut to the approximate size of the preparation using a pair of crown shears (Figure 14.5B). The ability of the aluminium to be worked and shaped lends itself to this process.
• It will not be possible to perforate the metal shell should the occlusion dictate it.
• No other information may be gleaned from it, for example, whether sufficient interocclusal clearance has been prepared, as described earlier.
• If there is any wear on the restoration, the temporary cement will be exposed and the restoration is more likely to fail.
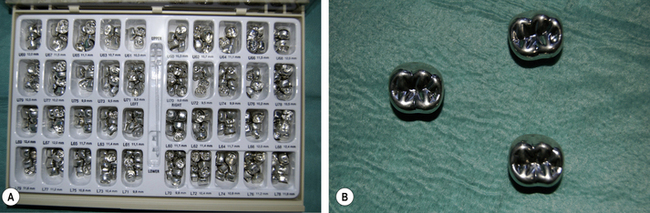
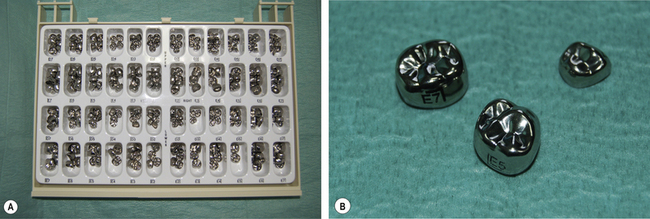
Stainless steel crown forms
The other metal crown form available is made of stainless steel (Figure 14.6). Its main indication is in paediatric dentistry for the restoration of badly broken down deciduous molars, particularly if pulpal treatment has been performed. These crown forms are much less malleable and ductile than the aluminium crown forms, thus they are harder wearing and are less likely to deform under load. They are usually not refined but trimmed using crown shears until their fit approximates to the prepared tooth. They are placed over the buccolingual bulbosity and snapped into place. They are then luted using a glass ionomer or polycarboxylate cement. The success rate with stainless steel crowns is very high and these crowns are useful to maintain the space that may be lost when a deciduous tooth is lost prematurely.
Acrylic materials used to refine temporary crown forms
All of the aforementioned crown forms except stainless steel crowns are used in conjunction with another material to enhance the fit between their internal surface and the preparation. The closeness of the fit between the inside of the temporary restoration and a retentive preparation will ensure that the restoration is retained satisfactorily. The original refining materials were chemically cured acrylics formed by mixing methylmethacrylate monomer with polymethylmethacrylate micro-bead powder. Unfortunately there were some problems associated with these materials (Table 14.1). These shortcomings have made these materials almost obsolete and other materials have evolved in an attempt to eliminate their disadvantages. Monofunctional acrylate monomers with a higher molecular weight became available as their properties were an improvement on the original material. This family of materials is called the higher methacrylates and these are the most commonly used materials to refine a temporary crown form.
Table 14.1 Disadvantages of methylmethacrylate/polymethylmethacrylate temporary material and their clinical ramifications
| Disadvantage | Clinical impact |
|---|---|
| High polymerization shrinkage | Unsatisfactory fit |
| Poor mechanical strength | Breakage during function |
| Highly exothermic setting reaction | Thermal trauma to the pulp |
| High level of monomer release | Significant pulpal irritation |
| Poor wear resistance | Undesirable wear during function leading to perforation or fracture of the temporary leading to occlusal instability |
| Poor aesthetics | Unsightly restoration |
| Chemical interaction with eugenol | Non-eugenol-containing products should be used |
Higher Methacrylates
Chemically these materials are a combination of polyethylmethacrylate beads and the liquid polybutylmethacrylate (Table 14.2). The presence of a tertiary amine results in these materials tending to turn yellow after setting. This is particularly marked in sunlight as the solar ultraviolet breaks down the amine, causing a colour change.
Table 14.2 Components of a higher methacrylate material and their role in the reaction in the powder and liquid
| Chemical | Role | |
|---|---|---|
| Powder | Polyethylmethacrylate | Polymer |
| Benzoyl peroxide | Initiator | |
| Liquid | Polybutylmethacrylate | Monomer |
| Tertiary amine | Activator |
Setting reaction
Higher methacrylates set by a polymerization reaction, and, as there is no inert filler, they will exhibit significant polymerization shrinkage on curing, which is in the order of 7% linearly. It is important to try to compensate for this large amount of shrinkage clinically (see Box 14.2, p. 223).
Box 14.2 Preformed crown form and refining using an acrylic material
2. Select a crown form that approximately corresponds to the tooth being temporized.
3. Trim this crown form (using an acrylic bur for a polycarbonate crown form and crown shears for a stainless steel crown form) so that the margins approximate those of the preparation. Roughen the internal surfaces of the polycarbonate crowns.
4. Mix the acrylic material to the consistency of wet sand.
5. Fill the crown form by running the material down the sides to ensure no air bubbles are incorporated inside the crown form.
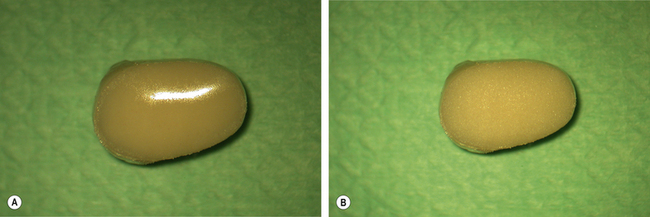
6. Allow the excess monomer to evaporate and watch the surface until it turns from a shiny to matt finish (Figure 14.7).
7. At this point fully seat the temporary crown onto the moist preparation and remove the obvious excess using a probe or flat plastic to prevent it setting into the undercuts so that the crown can be removed easily later.
8. Remove and reseat the crown several times to reduce the effect of polymerization shrinkage.
9. Place in hot water to accelerate the setting reaction.
10. Trim the margins using an acrylic bur and reseat on the preparation to verify the margins.
When the powder and liquid are combined, a mass is produced which has the consistency of wet sand. At this point the monomer is starting to soften and dissolve the outer surface of the resin polymer beads. The mass then develops a glossy surface. This dough stage is convenient as it aids clinical handling. As the reaction progresses, the surface of the material loses its gloss and turns to a matt appearance (Figure 14.7). It now corresponds to the snap stage and is now ready for use. For more information on acrylics, see Chapter 23. The polymerization reaction is exothermic in nature and care must be taken when using this material on a vital preparation to prevent thermal injury to the pulp.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses