Impression Materials
Chapter Objectives
On completion of this chapter, the student will be able to:
1. Describe the purpose of an impression.
2. List the various categories of impression materials and explain their differences.
3. Describe important characteristics of impression materials.
4. Describe the factors that make agar hydrocolloid a reversible material.
5. Define sol and gel and describe these states as they occur with the hydrocolloids.
6. List the components of alginate impression material and discuss their functions.
7. Explain why alginate is an irreversible hydrocolloid.
8. List the supplies needed to make an alginate impression and explain how they are used.
9. Demonstrate tray selection for alginate impressions for a patient.
10. Demonstrate mixing alginate, loading and seating the tray, and removing the impression.
11. List criteria for an acceptable alginate impression.
12. Demonstrate the proper handling of alginate impressions.
13. Apply troubleshooting to problems experienced with alginate impressions.
14. Describe the different types of elastomers and explain why they are called elastomers.
15. Discuss similarities and differences among the physical properties of the various elastomers.
16. List the uses of polyether impression material and discuss its advantages and disadvantages.
17. List the uses of polysulfide impression material and discuss its advantages and disadvantages.
18. Explain why polyvinyl siloxane impression material is so popular.
19. Explain the most advantageous clinical feature that polyether impression materials possess.
20. Explain the difference between a hydrophobic and a hydrophilic impression material.
21. Explain why some impression materials should be poured immediately and others can wait until later.
22. Discuss the uses of inelastic impression materials and why they are seldom used today.
Key Terms defined within the chapter
Bite Registration an impression of the occlusal relationship of opposing teeth in centric occlusion (patient’s normal bite)
Hydrocolloid a water-based colloid used as an elastic impression material
Reversible Hydrocolloid an agar impression material that can be heated to change a gel into a fluid sol state that can flow around the teeth, then cooled to gel again to make an impression of the shapes of the oral structures
Irreversible Hydrocolloid an alginate impression material that is mixed to a sol state and as it sets converts to a gel by a chemical reaction that irreversibly changes its nature
Agar a powder derived from seaweed that is a major component of reversible hydrocolloid
Gel a semisolid state in which colloidal particles form a framework that traps liquid (e.g., Jell-O)
Imbibition the act of absorbing moisture
Condensation Silicone a silicone rubber impression material that sets by linking molecules in long chains but produces a liquid by-product by condensation
Polyvinyl Siloxane (PVS) very accurate addition silicone elastomer impression material; it is used extensively for crown and bridge procedures because of its accuracy, dimensional stability, and ease of use
Impression Compound an impression material composed of resin and wax with fillers added to make it stronger and more stable than wax
Impression Plaster an impression material composed of a gypsum product similar to plaster of Paris
Zinc Oxide Eugenol (ZOE) a hard and brittle impression material used in complete denture procedures
In dentistry, an impression material is used primarily to reproduce the form of teeth, including existing restorations and preparations made for restorative treatments, as well as the form of other oral hard and soft tissues. Impression materials are also used by maxillofacial prosthodontists to make molds of facial defects resulting from cancer and trauma, so that they can construct facial prostheses to restore facial form. When used to replicate oral structures, the impression materials must be in a moldable or plastic state that can adapt to the teeth and tissues. Usually, the impression material in its plastic state is loaded into a tray for carrying it to the mouth and supporting it so that it does not slump and distort. Within a specified period of time, the impression material must set to a semisolid, elastic, or rigid state. Elastic impression materials are used more extensively than rigid materials, because elastic materials flex from tissue undercuts when removed from the mouth, whereas rigid materials cannot. The completed impression forms a negative reproduction of the teeth and tissues. When plaster or stone is poured into the impression and hardened, the replica that is formed is a positive reproduction of the teeth and tissues (see Chapter 15). The replica is called a cast or model. In the initial diagnosis and treatment planning phase, the dentist may request that the dental assistant or hygienist make impressions of the teeth and surrounding structures, so that diagnostic casts, commonly called study models, can be made for further study when the patient is no longer present. When an impression is made of a tooth that has been prepared for a restoration, the replica of the prepared tooth is called a die and is used for fabrication of the restoration in the dental laboratory. In some states, dental assistants and hygienists can be licensed in extended functions that include making final impressions for crown and bridge and partial denture procedures. Figure 14-1 shows an impression and the mold and die made from that impression. Use of the die allows the dentist or laboratory technician to perform the procedure by the indirect technique. With the indirect technique, the restoration is not made directly on the tooth, as with the direct placement of amalgam, but is constructed in the laboratory (indirectly) and later is cemented on the tooth.

Many different types of impression materials have been developed over the years, allowing the dentist to select materials according to the demands of the treatment and the oral environment. Participation in the making of impressions is one of the most frequently performed patient contact functions of the dental assistant and is performed increasingly by the dental hygienist. It is important that both have an understanding of the clinical applications, handling characteristics, physical properties, and limitations of these materials. They must also know proper techniques and materials for disinfecting the impressions.
Impression Trays
Impression trays are used to carry the impression material to the mouth and to support it until it sets, is removed from the mouth, and is poured into dental plaster or stone. They should be rigid to prevent distortion of the impression. They can be made for arches with teeth or for edentulous ridges. Impression trays can be pre-manufactured trays, called stock trays, which are purchased in a variety of sizes for both adults and children (Figure 14-2). Stock trays can be metal or plastic, and each of these can be solid or perforated (has holes in the sides and bottom to help retain impression material that extrudes through the holes). Solid trays often have raised borders on the internal surfaces that help lock in the impression material. These are called “rim-lock” trays. Some materials used in solid trays require the application of an adhesive to further retain them and prevent distortion of the impression if they should partially pull out of the tray. Plastic trays are inexpensive and are disposable, whereas metal trays are more expensive and must be cleaned and sterilized between uses. Impression trays can also be custom made. Custom trays are usually constructed in the laboratory with chemically cured, light-cured, or thermoplastic resins on casts of the teeth (see Chapter 16). They are custom fit to the mouth of the individual. They can also be made by lining a stock tray with a putty material that is adapted to the dental arch of the individual, and then an impression is made in this arch-adapted custom tray. Both stock trays and custom trays can be made for full arch impressions or for sectional impressions for part of an arch. The triple tray (also called double-bite, dual-arch, or check-bite tray) is a stock sectional tray that is used to make an impression of the teeth being treated and the opposing teeth at the same time and, if used properly, will capture the correct centric occlusion (bite) of the patient. Bite registration trays are typically U-shaped plastic frames with a thin fiber mesh stretched between the sides of the frame. The mesh retains the impression material (called bite registration material) and is thin enough so as not to interfere with closure of the upper and lower teeth in proper bite relationship. Bite registration material is placed on both sides of the mesh, the frame is positioned over the teeth to be recorded, and the patient closes into the normal bite relationship until the material sets.

Elastic Impression Materials
Hydrocolloids
A colloid is a glue-like material composed of two or more substances in which one substance does not go into solution but is suspended within another substance. Hydrocolloids are water-based colloids that function as elastic impression materials. The two hydrocolloids used in dentistry are agar hydrocolloid (or reversible hydrocolloid) and alginate hydrocolloid (or irreversible hydrocolloid). Much like gelatin, when agar powder is mixed with water, it forms a glue-like suspension that entraps the water, making a colloidal suspension called a sol. Heating it will disperse the agar in the water faster. When the agar sol is chilled, it will gel, becoming semisolid or jelly-like (like Jell-O). When the agar gel is heated, it will reverse its state back into a liquid suspension (sol). Therefore, it is a reversible hydrocolloid. Alginate powder will also form a sol that gels. However, with alginate, a chemical reaction occurs that prevents it from reversing back to a gel when heated. Therefore, it is an irreversible hydrocolloid.
Reversible Hydrocolloid (Agar)
Reversible hydrocolloid was introduced into dentistry in 1925 and was the first elastic material to gain popularity. It overcame many of the problems with inelastic materials (discussed later in this chapter) in that it could take accurate impressions of teeth and arches with tissue undercuts and could be removed from the mouth without injuring the patient or breaking. Its main clinical use is for impressions of operative and crown and bridge procedures. It also has uses in the laboratory for the duplication of casts (models). Its use has declined over the years as elastic (rubber) impression materials have been introduced.
Composition
The agar is derived from an extract of seaweed called agar-agar. The impression material is made from reversible agar gels. The components of the agar gels are 12% to 15% agar, 1% potassium sulfate to ensure proper set of the gypsum material poured in the impression, 0.2% borax as a strengthener for the gel, 0.1% alkyl benzoate as an antifungal during storage, and 85% water. Borax and agar retard the set of gypsum products, so potassium sulfate is added to cancel out their effect (Table 14-1).
TABLE 14-1
Composition of Agar Hydrocolloid Impression Material
| Material | Percentage (Approximate) | Purpose |
| Agar | 12%–15% | Colloidal particles as basis of the gel |
| Potassium sulfate | 1% | Ensures set of gypsum materials |
| Borax | 0.2% | Strengthens gel |
| Alkyl benzoate | 0.1% | Antifungal agent |
| Water | 85% | Dispersing medium for the colloidal suspension |
Clinical Application
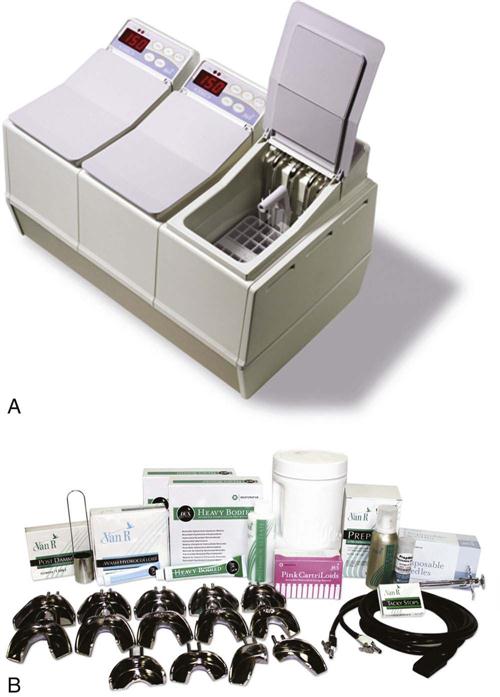
The agar hydrocolloid impression material has been known for many years as simply “hydrocolloid.” The use of hydrocolloid requires equipment specific for its use. The impression trays are stock metal trays (called water-cooled trays) with tubing running through them that connects to a water line by rubber hoses to circulate tap water through the tray. The water cools the impression material so that it gels within a reasonable period of time (about 3 minutes). Stock trays also allow for an adequate thickness of material to minimize the dimensional changes seen when hydrocolloid is too thin.
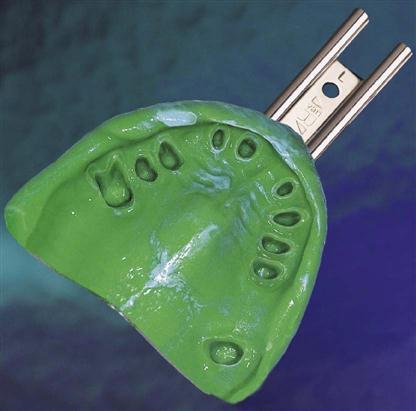
Hydrocolloid is supplied in plastic tubes, as sticks supplied in a glass jar, and as gel in glass cartridges. Two viscosities of hydrocolloid are used to make the impression. The variation in viscosity is achieved by altering the agar content. A stiffer hydrocolloid has more agar. A stiffer hydrocolloid is used to load the tray. A more fluid type is supplied in a glass cartridge that fits the syringe. To prepare the material for making an impression, a special heating unit called a hydrocolloid conditioner is used (Figure 14-3). The conditioner has three water bath chambers, each set to a different temperature. When the hydrocolloid gels are heated to 71°C to 100°C (160°F to 212°F), they become liquid (sol state). The tray and syringe hydrocolloid are liquefied in 10 minutes in boiling water (100°C) in the first chamber. A second chamber is maintained at between 60°C and 66°C and acts as a storage chamber where the tray and syringe hydrocolloid can be maintained in a liquid state for several hours, if needed. In a busy dental office, the hydrocolloid can be prepared in the morning and kept ready for use all day. A third chamber is kept at 45°C to 47°C and is used to temper the tray hydrocolloid for 3 minutes before the impression is taken. Tempering prevents burns to the oral mucosa or potential pulpal damage to prepared teeth. The syringe hydrocolloid is not tempered, because it is dispensed in such a small stream that it cools quickly as it passes out of the needle-shaped dispensing tip and flows around the prepared teeth and into the gingival sulcus. After delivering the syringe material, the tray is quickly connected to the water hoses and is seated over the teeth, and then the water is turned on to cool the material. When the hydrocolloid is cooled to 30°C to 45°C (86°F to 113°F), it returns to a solid (gel). The temperature at which the hydrocolloid liquefies is not the same temperature at which it solidifies (a phenomenon called hysteresis) and is unlike that of other substances, such as water, that have the same melting and freezing points. After the hydrocolloid has adequately gelled, the tray is removed from the mouth quickly with a snap. This allows the material to be removed from undercuts without tearing. Slow removal is more likely to cause the material to tear, particularly where it is thin. The gel reproduces fine detail of the preparations (Figure 14-4).
An advantage of the hydrocolloid is related to its hydrophilic (water-compatible) nature. It can be used in a moist field. The teeth are not dried before the hydrocolloid is placed. In situations where there is little bleeding or moisture, the hydrocolloid can still obtain an accurate impression, whereas the elastomeric impression materials (discussed later in this chapter) require a dry field. A wetting agent is sprayed on the preparation to aid in establishing intimate contact of the hydrocolloid with the prepared tooth.
Physical Properties
The impression must be poured immediately after it is made and disinfected, because it is dimensionally unstable. The gel will lose moisture and shrink if left in the air. If it must be stored for a short period of time, the impression should be placed in a humidor with 100% relative humidity or wrapped in a wet paper towel and sealed in a zippered plastic bag. The risk of distortion of the impression is great if it is not poured within an hour. The impression will imbibe water and swell if left in water or disinfecting liquid for more than a short period of time (10 to 30 minutes). Shrinkage or swelling will result in an inaccurate cast and a poorly fitting restoration. When left standing, many gels undergo a process called syneresis, whereby they contract and some of the liquid is squeezed out of the gel, forming an exudate on the surface. This loss of water changes the properties of the material. Hydrocolloid impressions can be poured only once to make a cast, because they lose water and change dimensionally.
The tear strength for agar hydrocolloid is similar to that of alginate, but it not as strong as the elastomeric rubber materials discussed later in this chapter. Both agar and alginate hydrocolloid will deform if compressed, but may recover or rebound to the original shape if the compression is not too great. If the compression is too great, the deformation will be permanent.
Although agar hydrocolloid is an inexpensive impression material with excellent accuracy, many practitioners have switched to newer generations of elastomeric impression materials for some of the following reasons: (1) the impressions do not need to be poured immediately; (2) they can be poured more than once; (3) they are highly accurate and dimensionally stable for longer periods; (4) they do not require expensive equipment such as hydrocolloid conditioners; and (5) they do not require the use of water-cooling hoses that sometimes leak.
Irreversible Hydrocolloid
Alginate, also called alginate hydrocolloid or irreversible hydrocolloid, is by far the most widely used impression material. It is inexpensive, is easy to manipulate, requires no special equipment, and is reasonably accurate for many dental procedures. Alginate is used for making impressions for diagnostic casts, partial denture frameworks, and repairs of broken partial or complete dentures, as well as for fabrication of provisional restorations, fluoride and bleaching trays, sports protectors, preliminary impressions for edentulous arches, and a multitude of other uses. However, it is not accurate enough for the final impressions for inlay, onlay, crown, and bridge preparations. It does not capture the fine detail of the preparation needed for a precise fit of the restoration. Also, it is thick and does not flow well into embrasures or occlusal surfaces. Final impressions are made with more accurate materials such as agar hydrocolloid or one of the elastomers. Final impressions are used to make detailed replicas of the prepared teeth. It is from these detailed replicas that precisely fitting restorations will be made.
Composition and Setting Reaction
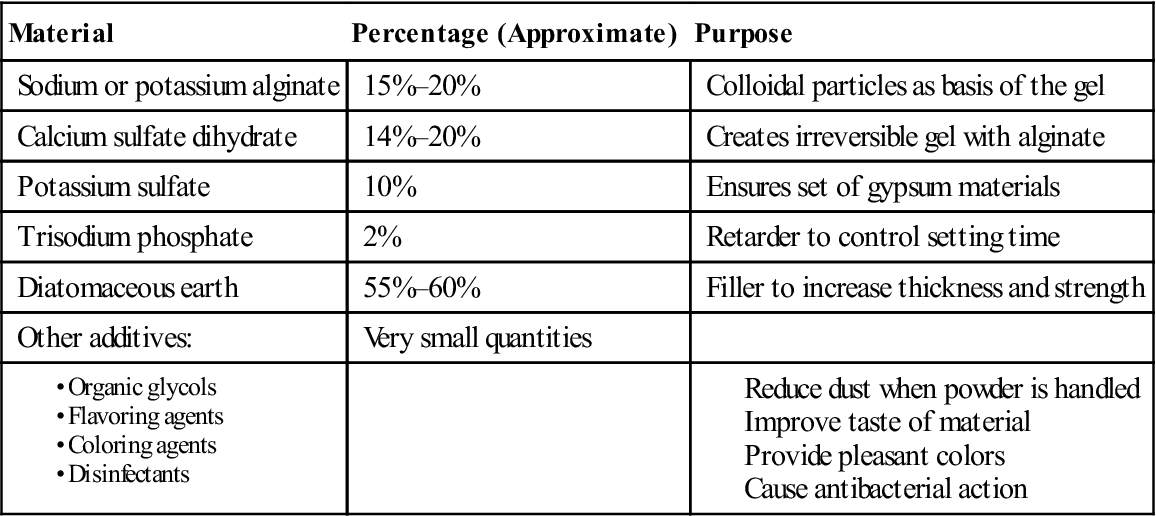
The main active ingredient in alginate is potassium or sodium alginate, which makes up 15% to 20% of the powder. Proportions of ingredients vary from manufacturer to manufacturer and with fast-, regular-, and slow-set materials. It is produced from derivatives of seaweed. Other components of the alginate powder include calcium sulfate dihydrate (14% to 20%), potassium sulfate (10%), trisodium phosphate (2%), and diatomaceous earth (55% to 60%). The “dustless” alginate powders have organic glycols added to keep powder from becoming airborne when it is dispensed. Other additives may include flavoring agents, coloring agents, and disinfectants (Table 14-2).
TABLE 14-2
Composition of Alginate Impression Material
< ?comst?>
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
When alginate powder is mixed with water, calcium sulfate dihydrate reacts with sodium alginate to form calcium alginate. Calcium alginate is insoluble and causes the sol of mixed powder and water to gel. Because this occurs by a chemical reaction, it cannot be reversed back to the sol state as can agar hydrocolloid. It is a fairly rapid chemical reaction, so trisodium phosphate is added as a retarder to delay the reaction. The amount of retarder that is added will control the time of the set and will differentiate between fast- and regular-set alginates. Diatomaceous earth is added as a filler to increase stiffness and strength and to prevent the surface from being sticky. Potassium sulfate is added to keep the alginate from interfering with the set of the gypsum products used to pour the impression. Some manufacturers have added chemicals to the alginate that change color as the chemical reaction progresses to indicate when it is time to insert the impression, and that change again when it is time to remove the impression.
Working Time
Regular-set alginates have a working time (from start of mix to seating in the mouth) of 2 to 3 minutes, and fast-set alginate has a working time of 1.25 to 2 minutes (American Dental Association [ADA] specification no. 18 sets the minimum at 1.25 minutes). The longer the time used to mix the alginate, the faster it must be loaded into the tray and seated in the mouth.
Setting Time
Regular-set alginates set in 2 to 5 minutes, and fast-set alginates set in 1 to 2 minutes. Setting time can be lengthened by using cold water or shortened by using warm water. Adjusting the powder-to-water ratio can affect the set but also adversely affects the physical properties and therefore is not recommended. It is advisable to leave the impression in the mouth for an additional minute after it appears set, because the tear strength and the ability to rebound from undercuts without permanent deformation increase during this time.
Permanent Deformation
Alginate will be compressed when it is removed from undercuts in the mouth. The greater the compression, the more likely it is that the alginate will be permanently deformed to some degree. A certain thickness of alginate (2 to 4 mm) is needed between the impression tray and the teeth or tissue undercut. Thin alginate will deform more and will tear more easily. As with the reversible hydrocolloid, when the alginate impression is removed, it should be removed by a rapid “snap” to prevent the deformation of critical surfaces. If 8 to 10 minutes elapse from the time the impression is removed from the mouth until it is poured, some recovery or rebound will occur from the deformation. That deformation which does not recover is the permanent deformation, and it will be recorded in the poured gypsum cast as a distortion. As long as the distortion is small, it may not be clinically significant. Usually, the time needed for disinfecting the impression is at least 10 minutes, and most of the rebound will have occurred by then.
Dimensional Stability
Similar to agar hydrocolloid, alginate is very sensitive to moisture loss and will shrink as a result. Once the impression is removed from the mouth, it should be rinsed and disinfected (see Procedure 14-4), wrapped in a damp paper towel, and sealed in a zippered plastic bag. Enclosing the impression this way will create an environment with 100% humidity to minimize water loss. Some moisture will be lost from the impression even in 100% humidity from syneresis, as with agar hydrocolloid. The paper towel should not be loaded with water, or the surface of the impression may become wet. If it imbibes water, it will swell and create some distortion. Ideally, the impression is poured after it is disinfected. If the impression must be stored until it can be poured a few hours later, it must be kept in 100% humidity (as with the damp towel and zippered plastic bag).
Tear Strength
The tear strength of alginate is more important than its compressive strength, because most commercial alginates far exceed the minimum allowable value for compressive strength. Alginate mixed with too much water will be weaker and more likely to tear on removal from the mouth. Thin sections of alginate are also prone to tearing. Additionally, slow removal of the alginate from the mouth will contribute to tearing. If the impression can be left in the mouth for an additional minute beyond the point when it is set, it will increase in tear strength. When properly handled, alginate has adequate tear strength.
Impression Making
(See Procedure 14-1.)
Objective
The objective of impression making is to reproduce the oral structures with acceptable accuracy while practicing good infection control and maintaining patient comfort. The dental assistant and the dental hygienist can make alginate impressions for diagnostic casts. They will need to prepare the patient for the impressions and to dispense, mix, and load alginate into trays. Following removal of the impression, the assistant or the hygienist disinfects and properly handles the impression until it is poured with the appropriate gypsum material. The assistant or hygienist also may be responsible for clearing residual alginate from the mouth and face of the patient.
Tray Selection
Stock trays work well with alginate, because they leave plenty of room for an adequate thickness of alginate. Alginate must be tightly adapted to the tray to be accurate. If the alginate pulls loose from the tray, a distortion will occur. If a tray is set on the bench top, unsupported alginate extending from the back of the tray may lift a portion of the impression and dislodge it from the tray. A perforated tray can be used because the alginate oozes through the perforations and locks into place. A solid tray can also be used if an adhesive made for alginate is applied to the inside of the tray before the alginate is loaded. Solid rim-lock trays should also have adhesive applied because alginate will occasionally pull free from the rim-lock on removal of the impression. If disposable plastic trays are used, they should be rigid. Flexible plastic trays have the potential to distort under the weight of the wet gypsum during pouring or when used in areas of undercuts in the mouth.
A properly selected tray will cover all of the teeth and will extend into the facial and lingual vestibules without impinging on the tissues. It will extend posteriorly to include the retromolar area for a mandibular tray and the hamular notch area for a maxillary tray. It will be deep enough to provide at least 2 mm of space for alginate beyond the incisal and occlusal surfaces of the teeth. Occasionally, standard stock trays will not cover all of the desired areas for the impression and must be modified with utility wax to create appropriate extensions of the tray and support the alginate. A common area for this to occur is the third molar area of an individual with large jaws. Wax may also be added to the midpalatal area of the tray to support the alginate when the patient has a very deep palatal vault (see Procedure 14-1, Figure 14-13). Usually, the patient is asked to rinse the mouth to remove loose debris and thick saliva before the impression is made. An antimicrobial rinse may be used to reduce the number of oral pathogens.
Dispensing
Manufacturers supply measures for powder and water for their alginates. Use the appropriate ones and adhere to the recommended proportions of powder and water to maintain the desired physical properties of the alginate. Powder measures (also called scoops) will vary among manufacturers, so do not interchange them with other manufacturers’ scoops. The same principle applies to water measures.
During shipping or prolonged periods of sitting, the powder may pack tightly and some of the ingredients may settle out, so that they are not evenly distributed throughout the powder. The measure of powder taken will be greater than the manufacturer intended when developing the measuring scoop. When the compacted powder is incorporated into the recommended volume of water, the resulting mix will be too thick and will often set too rapidly. To prevent this from happening, containers of alginate such as cans or plastic containers should be turned end-over-end a few times to decompress (fluff) the powder and mix the ingredients. Some alginates are supplied in pre-measured, watertight packages with a quantity suitable for a medium-sized arch (equivalent to two scoops with most manufacturers). This packaging is more expensive, but some practitioners find it to be convenient, to provide a more consistent mix, and to minimize cross-contamination.
Mixing
For a moderate to large upper adult arch, 3 scoops of alginate powder is usually required; a small upper arch requires 2 scoops. Most adult lower arches require 2 scoops. One unit of water is required per scoop. Typical water measures are marked to indicate up to 3 units. Room temperature tap water is placed in the rubber bowl, and the powder is added to it. Cold water retards the set, and warm water accelerates it. The powder is stirred into the water so that the powder is wet. Next, the wet powder is aggressively mixed against the sides of the bowl with a wide-bladed spatula. Some operators prefer to rotate the bowl in one hand while mixing with the other. Some offices use mechanical mixing machines for rapid mixing, ease of use, and a consistent mix. The rubber bowl is attached to the mechanical mixer that spins the bowl. With both mechanical and hand-mixing, the water-powder mixture is forced against the sides of the bowl to further incorporate the powder into the water and to force out entrapped air. Mixing should be completed within 45 seconds for regular-set alginate and within 30 seconds for fast-set alginate. The completed mix should have a creamy consistency (see Figure 14-14). If it appears grainy, it has not been mixed thoroughly.
Loading the Tray
Mixed alginate is picked up on the spatula and is forced into the depth of the tray. This action forces out air, thus preventing large voids in the impression. The alginate should be loaded in large increments as quickly as possible. The greater the number of small increments added to the tray, the greater is the chance for entrapped air. The tray should be loaded until the alginate is even with the tops of the sides of the tray. A wet, gloved finger is used to smooth the surface of the alginate and to create a shallow trough over the ridge area of the alginate (see Figure 14-1) that reduces the chance for entrapped air and helps to orient the tray over the teeth when it is seated.
Seating the Tray
Once the tray is loaded, the operator should take some alginate from the bowl on the gloved index finger and wipe it on the occlusal surfaces and embrasures of the teeth to force air out from the grooves and embrasure spaces. If regular-set alginate has a 2-minute working time and the alginate was mixed for 45 seconds, the operator has 75 seconds to load the tray, wipe the alginate on the teeth, and seat the tray. For fast-set alginate, the operator has about 45 seconds for the same process after mixing for 30 seconds. On warm days, the tap water may be warmer than usual and may accelerate the set. Conversely, on cold days, cooler tap water may retard the set.
For the lower impression, the operator is usually standing in front of the patient to one side at approximately the 7 o’clock position. The right side of the tray is used to retract the left corner of the mouth, and a finger or mouth mirror retracts the right corner. The tray is rotated into the mouth, aligned over the teeth with the tray handle in the midline, and seated in the posterior first. The tray is then seated in the anterior, and as it is being seated over the incisors, the lower lip is pulled out of the way to allow alginate to flow into the anterior vestibule. The patient is asked to lift the tongue to the roof of the mouth momentarily and then to relax it. This tongue motion allows alginate to flow into the lingual vestibule and defines the lingual frenum attachment. The tray is stabilized by the index and middle fingers of the right hand over the right and left sides of the arch. (All of these procedures should be appropriately repositioned for a left-handed operator.) The procedure is similar for the upper arch with the following modifications. The operator stands just behind the patient at the 11 o’clock position and retracts the right corner of the mouth with the side of the tray while retracting the left corner of the mouth with the index finger of the other hand. The tray is rotated into position, aligned over the teeth, centered with the midline, seated in the posterior first, and gently seated toward the anterior to allow alginate to flow forward and not back into the palate. Trays can also be placed while the patient is in the supine position. A right-handed operator can seat the lower tray from the 8 o’clock position and the upper tray from the 11 or 12 o’clock position, and left-handed operators from comparable positions on the opposite side (4 o’clock for lower and 12 or 1 o’clock for upper). The patient should be seated upright after the tray is placed to minimize the collection of saliva and alginate at the back of the throat. For both upper and lower impressions, the posterior aspect of the tray should be inspected for proper seating and for excess alginate. Excess alginate should be swept away quickly with the mouth mirror or a cotton swab to prevent a gagging or breathing problem for the patient.
Removing the Tray
Alginate left in the mixing bowl can be checked for completeness of set. The impression should be left in the mouth for approximately 1 minute after the set, because it gains in tear strength during this time. This may not be possible with patients who gag easily. When ready to remove the tray, use a finger at the side of the tray to apply pressure to break the seal while pulling the tray quickly away from the teeth with a snap. Protect the teeth in the opposing arch with fingers placed on top of the tray.
Handling the Impression
The impression should be rinsed thoroughly under running water to remove adherent saliva. Next, it should be evaluated to determine whether the impression is acceptable for its anticipated use. If determined to be acceptable, the impression is sprayed with a suitable disinfecting solution. A laboratory knife is used to remove excess alginate out the back of the tray. Any pooled fluid is drained or shaken off, because the alginate can imbibe moisture and swell. It is wrapped in a damp paper towel and placed into a zippered plastic bag marked with the patient’s name until ready to pour. Ideally, the impression should be poured within an hour, because it is not dimensionally stable and can lose water by syneresis even in 100% humidity.
Criteria for Clinically Acceptable Alginate Impressions
Alginate impressions should be evaluated immediately after they are removed from the mouth and rinsed. The determination should be made at this point as to whether or not the impression should be repeated, so it can be done while the patient is still seated and the operatory is set up for it. An acceptable impression will cover all areas of interest (teeth, ridge form, muscle attachments, palate, etc.). The structures should be recorded with sufficient detail to be clearly identified and should not have a grainy surface, which is usually the result of inadequate mixing. There should be minimal voids caused by entrapped air, especially in areas critical to the use of the impression (e.g., occlusal surfaces if a night guard will be made). The alginate should be fully seated in the tray and should not have pulled free or distorted. The impression should be free of debris. Table 14-3 lists criteria used to assess an alginate impression for clinical acceptability. When problems are found with the impression, refer to Table 14-4 for a troubleshooting guide that suggests possible causes and solutions for a variety of problems.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses