Healing of Oral Wounds
Factors Affecting Healing of Oral Wounds
A number of factors influence the healing process of wounds in the oral cavity. Although interference with the normal healing phenomena is not a common occurrence, the dentist must recognize the possible causes.
Hormonal Factors
Adrenocorticotropic hormone (ACTH) and cortisone are substances that have been repeatedly shown to interfere with the healing of wounds. Not long after ACTH and cortisone were first used clinically, it was noted that wounds in recipients of these compounds exhibited delayed healing. Since this observation, a number of careful experimental studies were carried out in which it was shown that, in patients receiving ACTH or cortisone, the growth of granulation tissue was inhibited, apparently because of inhibition of proliferation of new fibroblasts and new endothelial sprouts and because of a depression of the inflammatory reaction. There is apparently not an actual suppression of mesenchymal activity, but rather a delay in the mesenchymal reaction. An experimental study by Shafer on the healing of extraction wounds in rats receiving cortisone showed that the healing of such wounds was delayed. This would suggest that patients under long time steroid therapy or with Cushing’s syndrome, should be carefully evaluated by the dentist before he or she carries out oral surgical procedures.
Complications of Wound Healing
Keloid and Hypertrophic Scar Formation
Keloids are overgrown scar tissues with no tendency for resolution. They occur in wounds, which heal without any complications. The common sites of occurrence include chest, back and shoulders.
Biopsy and Healing of Biopsy Wound
Types of Biopsy
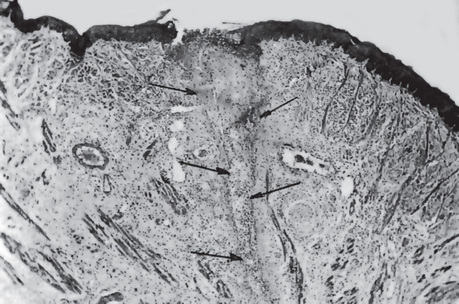
Some lesions are too large to excise initially without having established a diagnosis, or are of such a nature that excision would be inadvisable. In such instances, a small piece is removed for examination. This is termed an incisional or diagnostic biopsy (Fig. 14-1). It is most useful in dealing with large lesions, in which the operator suspects may be treated by some means other than surgery once the diagnosis is made, or lesions in which the diagnosis will determine whether the treatment should be conservative or radical.
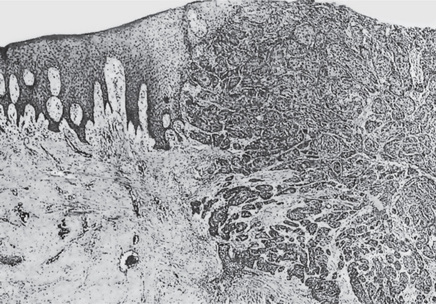
Figure 14-1 Epidermoid carcinoma, diagnostic biopsy.
An adequate border of normal mucosa was obtained with the biopsy of the neoplastic mass, and no attempt was made initially to excise the lesion completely.
There are several methods by which material may be obtained from a lesion for microscopic study:
• Surgical excision by scalpel
• Surgical removal by cautery or a high-frequency cutting knife
• Removal by biopsy forceps or biopsy punch
• Aspiration through a large bore needle
• The exfoliative cytology technique (q.v.) whereby the surface of a lesion is scraped and smeared on a microscope slide and studied by the pathologist after suitable staining.
Biopsy Technique
Biopsy technique is a simple procedure and may be carried out by any dentist as a routine clinical procedure if certain precautions are taken and certain rules are followed. The advantages of a biopsy so far outweigh its disadvantages or potential dangers that the biopsy is seldom, if ever, contraindicated in case of a lesion in which the diagnosis has not been established. To ensure obtaining a proper specimen for the pathologist, the following points must be considered:
1. Do not paint the surface of the area to be biopsied with iodine or a highly colored antiseptic.
2. If using infiltration anesthesia, do not inject anesthetic solution directly into the lesion. Inject around the periphery of the lesion instead.
3. Use a sharp scalpel to avoid tearing tissue.
4. Remove a border of normal tissue with the specimen if at all possible.
5. Use care not to mutilate the specimen when holding it with forceps.
6. Fix the tissue immediately upon removal in 10% formalin or 70% alcohol. If the specimen is thin, place it upon a piece of glazed paper and drop into fixative to prevent curling of tissue.
Healing of Biopsy Wound
Primary Healing
When there is a close apposition of the edges of the wound, the surface epithelium proliferates rapidly across the line of incision and re-establishes the integrity of the surface. The delicate connective tissue fibrils eventually coalesce into denser bundles and usually contract, so that in time all that is left to indicate the biopsy area is a small linear scar which may be depressed below the surface. Because there is no defect which must be filled with new tissue, this type of wound heals rapidly (Fig. 14-2).
Exfoliative Cytology
Exfoliative cytology is the study of cells which exfoliate or abrade from the body surfaces. The rationale for exfoliative cytology lies in epithelial physiology. Normal epithelium undergoes exfoliation of its superficial cells due to physiological turnover. The cells of the deeper layers are adherent to each other normally. When the epithelium becomes seat of any pathological condition, the cells may lose their cohesiveness, and cells in the deeper layer may shed along with the superficial cells. These exfoliated cells as well as cells which are scrapped off by means of specific instruments, can be studied quantitatively or qualitatively. Considerable interest has developed in the use of exfoliative oral cytology for the diagnosis of oral mucosal lesions (Fig. 14-3). Application of cytodiagnosis as a routine procedure in the detection of cervical cancer was introduced by George N Papanicolau in 1941. Its application in oral cancer has been known for a long time. In a review of the historic background of oral cytology, von Hamm cited numerous series of cases of patients with oral cancer in which the diagnostic accuracy of cytologic smears was compared with that of the surgical biopsy and was found to be almost identical. He concluded that:
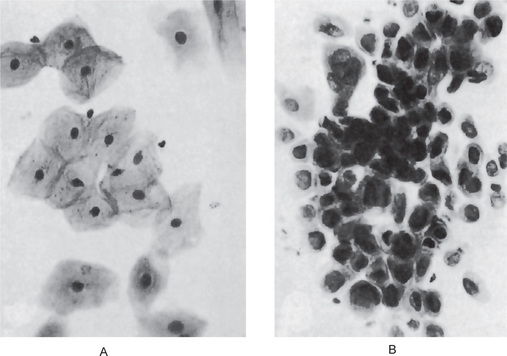
Figure 14-3 Oral mucosa, cytologic smears.
Normal epithelial cells are shown (A), contrasted with malignant cells from a patient with epidermoid carcinoma (B).
• Cytology is not a substitute but an adjunct to the surgical biopsy.
• It is a quick, simple, painless and bloodless procedure.
• It helps as a check against false-negative biopsies.
• It is especially helpful in follow-up detection of recurrent carcinoma in previously treated cases.
• It is valuable for screening lesions whose gross appearance is such that biopsy is not warranted.
Obviously, the use of the cytologic smear is predicated upon the proper preparation of the smear by the clinician and sufficient experience in its evaluation by the cytologist.
The cytologic smear will usually be reported by the cytologist as falling into one of five classes:
Though exfoliative cytological study has a significant role in cancer diagnosis, it has its own limitations. The presence or extent of invasion cannot be assessed. It should be remembered that the majority of benign lesions that occur in the oral cavity do not lend themselves to cytologic smear. For example, lesions which have a normal appearance and an intact surface, such as a fibroma, should be excised and never smeared. In addition, most authorities agree that leukoplakia does not lend itself to cytologic diagnosis because of the scarcity of viable surface cells in the smears taken from such lesions. Finally, it should be remembered that a negative cytology report does not rule out cancer and that a repeat smear or biopsy is indicated in all clinically suspicious lesions.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 . Factors Affecting Healing of Oral Wounds
. Factors Affecting Healing of Oral Wounds . Complications of Wound Healing
. Complications of Wound Healing . Biopsy and Healing of Biopsy Wound
. Biopsy and Healing of Biopsy Wound . Exfoliative Cytology
. Exfoliative Cytology . Healing of Extraction Wound
. Healing of Extraction Wound . Complications in Healing of Extraction Wounds
. Complications in Healing of Extraction Wounds . Healing of Fracture
. Healing of Fracture . Complications of Fracture Healing
. Complications of Fracture Healing . Replantation and Transplantation of Teeth
. Replantation and Transplantation of Teeth . Implants
. Implants