CHAPTER 14 Dental Imaging
Introduction
IR(ME)R operator: a person who is trained in dental radiography, for example a dentist, therapist, hygienist or a dental nurse who has undertaken a post-registration certificate course in dental radiography. (This involves completion of a record of experience in the workplace and passing an examination.) See also p. 333.
Types of dental radiograph
Dental radiographs are taken to aid:
Intra-oral Radiographs
For these radiographs, the X-ray films commonly used are called the periapical, bitewing and occlusal films (Figure 14.1), all of which are small enough to be partially inserted into the mouth. Intra-oral radiographs are taken to detect dental pathology including small carious lesions. They can be useful in the diagnosis of:
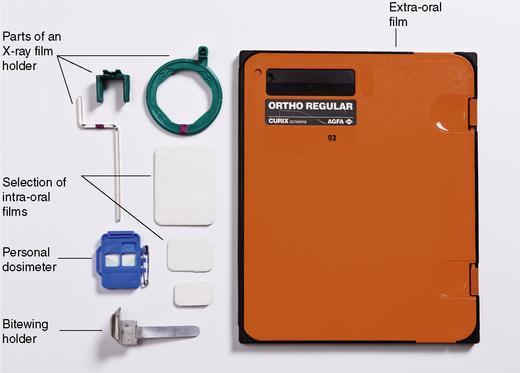
FIGURE 14.1 A selection of intra-oral films, extra-oral film in the cassette, holders and radiographic monitoring badge.
Positioning the patient and the film
Extra-oral Radiographs
Extra-oral radiography means using large films to visualise the skull, jaws, temporomandibular joints and sinuses. These films are used with intensifying screens in a cassette (Figure 14.1).
Examples of the use of intra- and extra-oral radiographs in dentistry are given in Table 14.1.
TABLE 14.1 Examples of the More Common Dental Radiographs and Their Main Uses
| Area to be Examined | Radiographic Film Used | Often Used for |
|---|---|---|
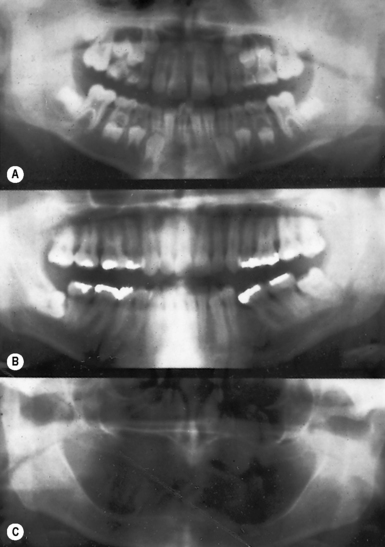
| Whole of the mandible and the maxilla | DPT (dental panoramic tomograph; Figure 14.2) | Presence and position of teeth; jaw fractures |
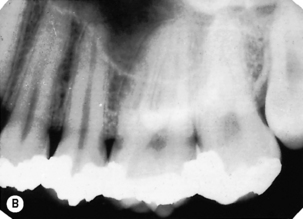
| A single tooth or three to four teeth plus the supporting bone | Periapical film (Figure 14.3): size varies from 35 × 22 mm to 40.5 × 30.5 mm | Assessing the periapical area, for root canal treatment and to assess root fractures |
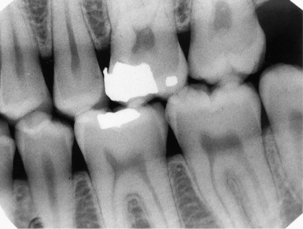
| Molar/premolar region | Bitewing (horizontal) (Figure 14.4): size varies from 35 × 22 mm to 54 × 27 mm | Caries detection interproximally |
| Bitewing (vertical) | Periodontitis | |
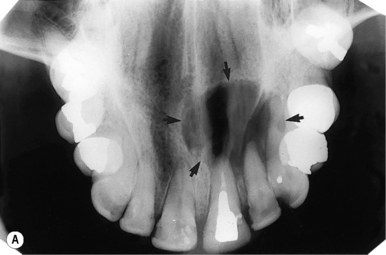
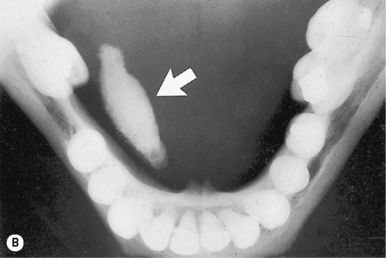
| Maxillary incisor/canine region | Anterior occlusal (Figure 14.5): size is about 57 × 76 mm | Impacted canines; super- numerary teeth; palatal cysts; salivary duct stones |
| Third molars | Oblique lateral, or DPT, or periapical | Inspecting unerupted or impacted third molars |
| Sinuses | DPT or occipito-mental radiograph | Sinusitis, root in sinus |
Cephalometric radiographs
These are a type of extra-oral radiograph often used in orthodontics (see Chapter 11 for more details).
Tomographs
Dental Panoramic Tomographs
A dental panoramic tomograph (DPT or orthopantomograph (OPG)) is used mainly to assess the lower part of the face. A DPT displays both the upper and lower teeth in a long flat film (Figure 14.2). It also gives a good overview of the maxillary sinuses, mandibular rami and the temporomandibular joints. It shows the number and position of all teeth including unerupted ones. However, it does not show fine detail of the anterior part of the jaws, as the spine gets superimposed during taking the film. DPTs are also not adequate for caries diagnosis. One panoramic film gives about the same radiation dose as 18–20 bitewings (see below).
Other types of imaging used in dentistry
Processing radiographs
Digital X-rays need no processing (see below). Otherwise, the radiographic film has several components apart from the actual celluloid film coated with emulsion (Table 14.2).
TABLE 14.2 Components of Radiographic Film, their Function and Disposal
| Intra-oral X-ray Film Packet Component | Function | Dispose into Waste Marked |
|---|---|---|
| Plastic envelope | Protects the film from moisture and light | Clinical |
| Black paper | Protects the film from light | Domestic |
| Celluloid film | Produces the radiograph | Domestic |
| Lead foil | Prevents radiation that has not been absorbed by the film passing on into the patient | Special |
The manual steps are as follows:
Faults in Radiograph Exposure and/or Processing
Faults in radiograph exposure and/or processing are shown in Table 14.3 and the accompanying figures.
| Film Appears | Reasons | Comments |
|---|---|---|
| Faint or blank | Under-developed, under-exposed, not fixed | Low temperature; wrong developing time; wrong strength of developer. See Figure 14.6A |
| Dark | Over-developed or over-exposed | High temperature; wrong developing time; wrong strength of developer. See Figure 14.6B |
| Foggy | Exposed to light before developing or old film | |
| Fading | Under-fixed | |
| Black /> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses