Chapter 13
The Narrow Ridge in the Maxilla and the Mandible and Its Correction: Ridge Splitting Using Piezoelectric Surgery and Grafting with or without Simultaneous Implant Placement
INTRODUCTION
Patients requiring dental implant treatment usually require ridge augmentation prior due to the resorptive process of the edentulous ridge following tooth loss. Several methods of augmentation have been reported in the literature, including particulate graft, block graft, distraction osteogenesis, and ridge-splitting technique, also known as the edentulous ridge expansion.
The edentulous ridge expansion (ERE) technique aims at creating a sagittal osteotomy of the edentulous ridge using instruments such as chisels or piezoelectric inserts between the two cortical plates to expand the ridge width and consequently allow for the placement of implants at the same visit or at a later stage.
The ERE technique is not a method for augmenting the ridge vertically; therefore, the presence of enough vertical height for implant placement is a requirement. Also, a minimum of 3 mm of bone width, including at least 1 mm of cancellous bone, is desired in order to insert a bone chisel between cortical plates and consequently expand the cortical bones. It has been shown that when using the piezoelectric inserts this procedure can be attempted in ridges with less than 3 mm bone width. A pyramidal form ridge with a wider base is the ideal indication for this technique because it will prevent the risk of buccal plate fracture. This approach can help in decreasing the treatment time where the implant is placed in the same visit; it also will correct the buccal concavity that is caused by the ridge resorption.
DEFINITION
Ridge splitting is a procedure for augmenting implant sites with a reduced bucco-lingual thickness (Seibert class I), by repositioning the buccal cortical plate.
The ridge-splitting technique aims at the creation of a new implant bed by longitudinal osteotomy of the alveolar bone.
The buccal cortex is repositioned laterally by greenstick fracture, and the space between the buccal and the lingual cortical plates is filled with autologus, allogenic, or alloplastic graft material.
Classification
There are two types of ridge splitting:
1. One-stage (ridge split with immediate implant placement)
2. Two-stage (ridge split plus graft, followed by implant placement at a later date)
HISTORY
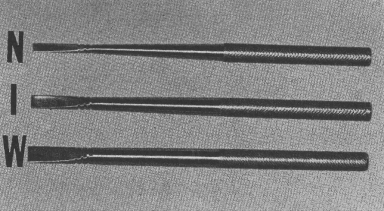
Tatum (1986) first described a technique to expand the cortical wall in cases with inadequate bucco-lingual thickness of bone using various sizes of channel formers (Figure 13.1).
Figure 13.1 Bone splitting chisels (W, wide; I, intermediate; N, narrow).
The edentulous ridge expansion was then reintroduced in 1990 by Bruschi and Scipioni. The technique consists of splitting the vestibular and buccal cortical plates (Scipioni et al. 1994) and further opening the space with Summers’s osteotomes (Summers 1994).
INDICATIONS
Indications for use of ridge splitting include:
1. Sufficient vertical bone height
2. Horizontal defect/narrow ridges (wide apically)
3. Presence of cancellous bone between the cortical plates
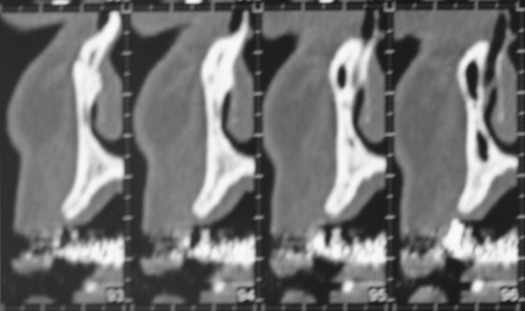
Figure 13.2 CT scan of two different type of ridges. The ridge on the left side is of triangular shape (base wider than coronal portion) and amenable to splitting. The ridge on the right side is parallel and not amenable to splitting.
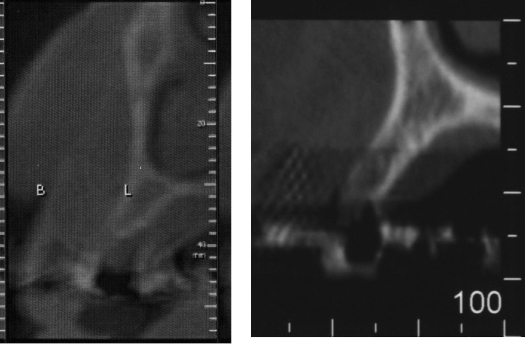
Figure 13.3 Clinical picture of a ridge that is narrow and “parallel”, thus not a good candidate for splitting.
CONTRAINDICATIONS
Contraindications for use of ridge splitting (Figure 13.4) include:
1. Ridge width less than 3 mm
2. Vertical ridge deficiency
3. Overangulated maxillary edentulous ridge
4. Single site in the mandible
Figure 13.4 Scalpel, bone chisels, and mallet used in ridge splitting.

TECHNIQUES
Splitting is classically performed with the following:
1. Chisel and mallet (Tatum 1986; Bruschi and Scipioni 1990; Coatoam and Mariotti 2003; Basa et al. 2004).
2. Oscillating saws (Zijderveld et al. 2004; Figure 13.5).
3. Extension crest device (Chiapasco et al. 2006).
4. Ultrasonic/piezosurgery (Vercelotti 2000).
Figure 13.5 Oscillating bone saw used for ridge splitting.
The use of bone chisel traumatizes and stresses the patient.
Fine-tuning of the splitting can be difficult when the crest is dense, especially in the mandible.
Rotating and oscillating instruments are time effective and less stressful for the patient. For the surgeon, however, the risk of encroaching the gingiva, the lips, or the tongue limits the accessibility and complicates the procedure.
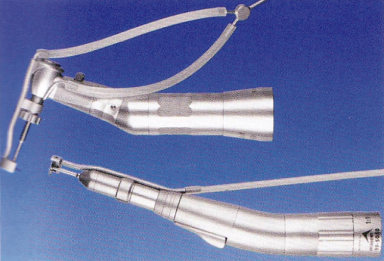
Ultrasonically moved knives have the ability to cut hard tissues, such as teeth and bone (Figure 13.6).
Figure 13.6 Piezotome (Satelec, Acteongroup, Merignac, France). Piezoelectric knife used for ridge splitting.

In contrast, soft tissues such as gingiva, blood vessels, nerves, and sinus membranes are preserved from injury because they vibrate with the tip.
Segmental ridge-split with ultrasonic bone saw (USBS) is predictable and does not lead to bone overheating or bone injury.
Advantages
There are several advantages for using splitting techniques:
- Discards the need for onlay graft (hip, maxillary tuberosity, chin, or the external oblique ridge)
- Avoids the use of a secondary surgical site that exhibits postoperative morbidity associated with bone harvesting
- Shortens the treatment due to immediate implant placement
- Reduces healing time
- Avoids palatally placed implants
- Avoids concave emergence profile
Disadvantages
There are also disadvantages to using splitting techniques:
- Fracture of the buccal plate
- Resorption of the buccal plate
- Possible surgical complications
- Benign paroxysmal positional vertigo
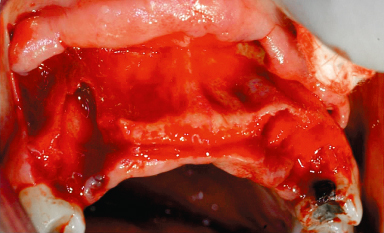
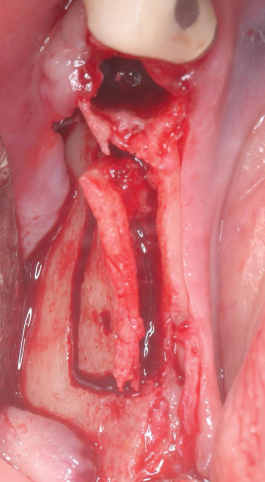
Buccal plate fracture may occur during (1) ridge expansion with chisels/osteotomes, (2) implant site preparation with drills, and (3) implant insertion (Figures 13.7, 13.8).
Figure 13.7 Buccal plate fracture in the front maxilla.
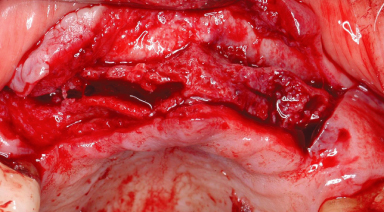
Figure 13.8 Buccal plate fracture in mandible.
THE USE OF DIFFERENT FLAP TECHNIQUES
Three types of flaps can be used in association with the edentulous ridge expansion technique: the full-thickness mucoperiostael flap, the partial-thickness flap, and the osteoperiosteal flap. The presence of osseointegration is not the only criteria of success in ridge-split cases; we need to maintain marginal bone stability and avoid buccal bone resorption or creation of fenestrations, which leads to the long-term success of the implants. It has been shown that the mucoperiosteal flap maintains the blood supply to the expanded area and stabilizes the displaced buccal plate of bone. Alveolar expansion, when done using either a partial-thickness flap or the minimally exposed osteoperiosteal flap approach, appears to consistently lead to sustainable alveolar width and osseointegration according to Jenson, Ellis and Glick (2009). Full mucoperiosteal flap approaches are less predictable with regard to buccal plate bone loss and resorption. The use of a full-thickness flap helps to avoid excessive bleeding, resulting in better visualization of the operating sites and better handling of the surgical steps. In cases where there is thin connective tissue, the partial-thickness flap procedure becomes extremely difficult, and the remaining tissue over the alveolar bone is too thin to protect the bone adequately. The osteoperiosteal flap is more technique sensitive, as it leads to the blind placement of implants and the failure to be able to visualize the entire length of the alveolar crest, which might lead to improper placement and positioning of the implants.
SURGICAL STEPS
Ridge Split without Implant Placement (Two Stages)
The evaluation of the preoperative computed tomography (CT) scan shows a bony structure that is favorable to splitting, but that will not allow simultaneous implant placement (Figure 13.9).
Figure 13.9 Preoperative CT scan prior to two-stage ridge splitting.
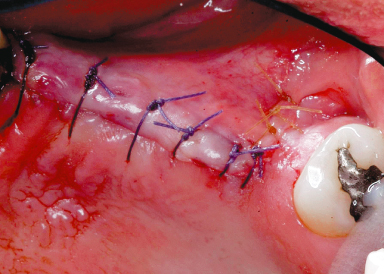
Local anesthesia is achieved by infiltrating xylocaine 2% containing 1 : 100,000 epinephrine. A midcrestal incision is made, and full-thickness flaps are reflected. If this technique is used in the maxilla, then the first bony cut could be done using a Rib-Back Bard-Parker blade (Figure 13.10). Subsequently, the crestal bone incision and the anterior and posterior bone-releasing incisions are completed with a surgical tungsten carbide bone cutter to create a trapezoidal-shape osteotomy. A bony chisel is then inserted in the initial crestal incision using a mallet and a light tapping force. The bone chisel is then gently “wiggled” bucco-lingually to enlarge the width of the osteotomy by gently displacing the buccal bony plate (Figure 13.11). This can be done in the maxilla quite easily as the bone is less dense than in the mandible. Once that opening between the two cortices (buccal and palatal) has been created, a bone graft is placed (Figure 13.12) and covered with a membrane (Figure 13.13). A periosteal release is necessary prior to closing the flaps by primary intention (Figure 13.14).
Figure 13.10 Crestal bony incision using a #15 blade and mallet.
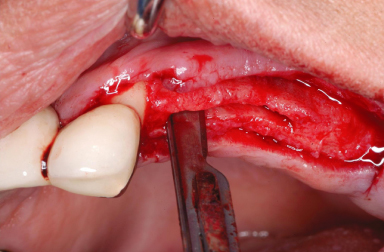
Figure 13.11 Deepening of the crestal bony incision using a bone chisel and mallet.
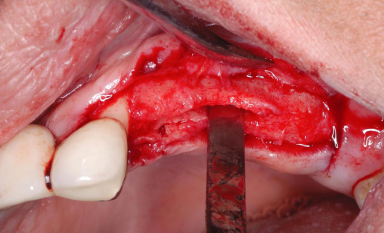
Figure 13.12 Intercortical bone grafting.
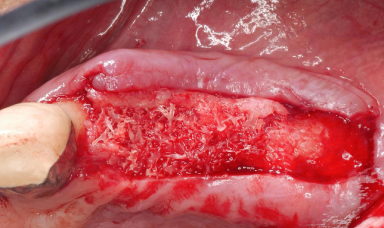
Figure 13.13 Membrane placed over the bone graft.
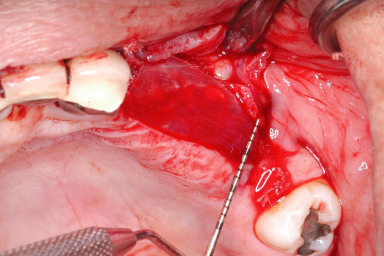
Figure 13.14 flaps sutured together (single interrupted sutures).
Ridge Split with Implant Placement Using the Osteotome Technique (One Stage)
After CT scan evaluation (Figures 13.15, 13.16), local anesthesia is achieved by infiltrating xylocaine 2% containing 1 : 100,000 epinephrine around teeth #8 and 10 (Figures 13.17, 13.18). A soft-tissue incision is made to create a total-thickness flap approximately 5 mm palatal from the crest of the ridge and extended at least 6 mm anterior and posterior to the area where fracture of the bone crest is planned (Figure 13.19). An anterior and a posterior releasing incision should be done, then a labial mucoperiosteal flap reflected, exposing the alveolar ridge and about 5 mm of the buccal cortex (Figure 13.20); the periosteum should then be dissected to produce a split-thickness flap. Different flap designs can be used as explained previously, depending on the surgeon’s preference. If this technique is used in the maxilla, then the first cut should be done using a Rib-Back Bard-Parker blade (Figures 13.21, 13.22). Because of the cortical nature of the mandibular ridge, the bone incision in the mandible should be made over the crest by first using a round diamond bur with diameter 0.8 mm and profuse irrigation to mark a dotted line; subsequently, the crestal bone incision and the anterior and posterior bone-releasing incisions are completed with a surgical tungsten carbide bone cutter to create a trapezoidal shape osteotomy.
Figure 13.15 Preoperative CT scan prior to one stage ridge splitting and implant placement (#9).
/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


