Implant Body Size
A Biomechanical and Esthetic Rationale
Carl E. Misch
The initial treatment plan for implant dentistry should include the ideal implant size based primarily on biomechanic and esthetic considerations. In traditional prosthetics, when a tooth is replaced, the abutment teeth are already provided by nature with wide posterior abutments for posterior teeth. When teeth are replaced with dental implants, the implant team should preselect the ideal implant size based on the ideal esthetic restoration within biomechanical guidelines.
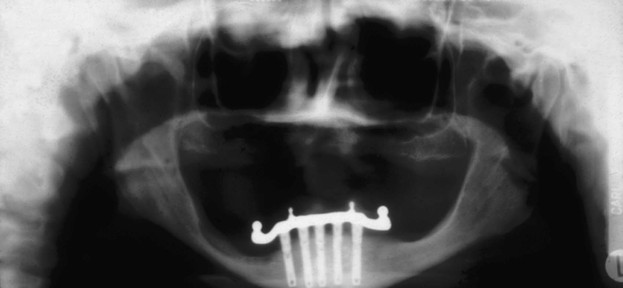
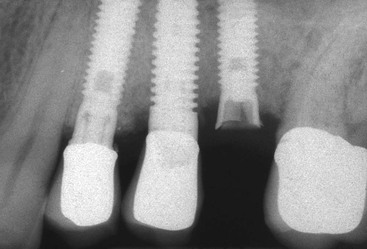
Historically, the size of an implant was determined primarily by the existing bone volume in height, width, and length. The surgeon would select longer implants in the anterior regions of the mouth and shorter ones in the posterior areas (or use cantilevered prostheses) because of the limits of the mandibular canal and maxillary sinus. The width of the implant, also determined during surgery, would relate to the existing width of available bone, and one diameter implant (4 mm) would be used in most all situations1 (Figure 13-1).
Over the years, dental implant treatment plans incorporating biomechanics have been advocated by the author to decrease the most common complications—those related to biomechanical stress.2 (Figure 13-2) The prosthesis first is planned, including whether the restoration is fixed or removable, how many teeth are replaced, and the esthetic demands. The patient force factors are then considered to evaluate the magnitude and type of force applied to the restoration. The bone density is evaluated in the regions of the potential implant placement. The key implant positions are determined followed by the additional implant number based on the patient force factors and the bone density in the implant sites. The key implant positions are important regardless of the patient force factors and bone density. The total implant number, on the other hand, is directly related to these force factors and bone density. For example, more implants should be used when the patient has parafunction or the bone is less dense because the greater force exerted on the implant abutments will transmit greater stresses to the implant–bone interface. In fact, implant number may also be a factor when the ideal size of the implant is inadequate for the biomechanical load. The next consideration in this ideal treatment plan sequence is the implant size2 (Box 13-1).
A comprehensive approach to the overall dental implant size begins with the identification of clinical problems to be addressed. Dental implants function to transfer loads to surrounding biological tissues.3,4 Biomechanical load management is dependent on two factors: the character of the applied force and the functional surface area over which the load is dissipated.5 The implant size directly affects the functional surface area that distributes a load transferred through the prosthesis. Fundamental scientific principles related to force and surface area are then combined with engineering principles to pursue the desired clinical goals. When relevant, esthetic considerations in regard to implant size are part of the evaluation. This chapter builds on and applies basic biomechanics and demonstrates how these principles also relate to the ideal dental implant size to support a prosthetic load. The esthetic guidelines related to implant size are also addressed.
Character of Forces Applied to Dental Implants
Stress and Strain
The presence of fibrous tissue has long been known to decrease the long-term survival of a root form implant.1 Excessive loads on an osseointegrated implant may result in mobility of the supporting device even after a favorable bone–implant interface has been obtained.6 Excessive loads on the bone result in increased strain conditions in the bone.7 These microstrains in the bone may affect the bone remodeling rate and cause pathologic overload, which results in the loss of bone. The amount of bone strain is directly related to the amount of stress applied to the implant–bone interface. The stress may cause complete implant failure, porcelain fracture, uncemented restorations, abutment screw loosening, implant and component fracture, and crestal bone loss (Box 13-2). Although several conditions may cause crestal bone loss, one of these may be prosthetic overload.8 The greater the stresses throughout the implant–bone interface, the greater the risk factor for any biomechanical complication, including crestal bone loss and implant failure.9 Therefore, the stress and strain relationship has been shown to be an important parameter to decrease any biomechanical complication.
Screw loosening is a complication that is especially noted in single-tooth replacement or individual crowns restored with multiple adjacent implants. Prosthetic screw loosening is affected by implant diameter.10 The larger the diameter of an implant, the less the force applied to the abutment screw and the less screw loosening. Hence, when lateral forces or cantilevers are present, especially when crown height or parafunction is greater than usual, the diameter of the implant body or the implant number (splinted together) should be increased to limit this complication.
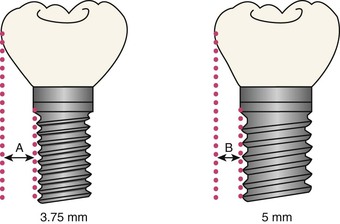
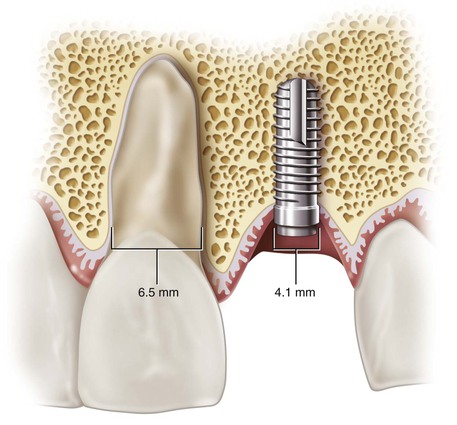
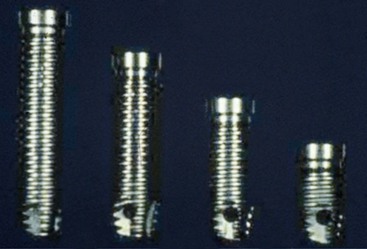
The increase in stress to an implant body also increases the risk of implant abutment screw or body fracture (Figure 13-3). The strength of an implant abutment screw or body is related to the radius times the power of 4. Hence, an implant or abutment screw twice the size is 16 times more resistant to failure. Hence, implant body size has several related biomechanical factors, including abutment screw loosening, crestal bone maintenance, implant survival, and implant component or body fracture. In addition, the emergence profile of the crown is related to the implant diameter (Figure 13-4). A deficient emergence profile from a narrow implant may affect esthetics, food entrapment, sulcular hygiene considerations, and probing assessment to evaluate long-term health.
Forces applied to dental implants may be characterized in terms of five distinct (although related) factors: magnitude, duration, type, direction, and magnification.5 Each factor should be considered within the physiologic constraints on implant size. As a result, a relative risk factor for different implant sizes may be established.
Force Magnitude
The physiology of the stomatognathic system imposes a range on the magnitude of forces that may be applied to an implant in the oral environment. The magnitude of bite force varies as a function of anatomical region and state of the dentition.11 Average bite forces can range from 10 to 350 lb. The magnitude of force is greater in the molar region (200 lb), less in the canine area (100 lb), and least in the anterior incisor region (25–35 lb).12 These average maximum bite forces increase with parafunction to magnitudes that may approach 1000 lb in the posterior regions.13
After sustained periods of edentulism, the bone foundation often becomes less dense. Studies on dentate and edentulous jaws illustrate greater trabecular bone density in the anterior regions compared with the molar regions.14 The bone’s ultimate strength is highly dependent on its density.15 As such, less dense bone may no longer be able to support normal physiologic bite forces on a dental implant. Careful treatment planning, including appropriate implant size selection, is imperative to lower the magnitude of loads imposed on the vulnerable implant–bone interface under these less ideal conditions. Thus, the posterior regions with higher bite forces and lower bone densities should use a different parameter for implant size compared with the anterior regions. As a consequence, the implant size in the molar region should be larger in diameter than the anterior and premolar region. When implant size is not greater than the anterior regions, implant number or design considerations (or both) should compensate for the greater force factors or deficient bone density.
Force Duration
The duration of bite forces on the dentition has a wide range. Under ideal conditions, the teeth come together during swallowing and eating for only brief contacts. The total time of these brief episodes is less than 30 minutes per day.13 Patients who exhibit bruxism, clenching, or other parafunctional habits, however, may have their teeth in contact for several hours each day. Fatigue fractures increase in direct relationship to the amount of the force and the number of cycles of load.5 Therefore, an increase in force duration directly increases the risk of fatigue load to the implant body when the force is higher than the endurance limit of these entities.16 The implant body width is directly related to the strength of an implant, and wider-diameter implants reduce the risk of fatigue fracture. Hence, the bending fracture resistance should be altered in patients with greater bite forces (e.g., parafunctional patients) by increasing implant diameter.
The duration of a force may also alter the implant–bone interface. Fatigue damage to cortical bone has been reported under relatively high-frequency loading rates (e.g., shin splints in runners).17 Although fatigue damage to alveolar bone has not yet been reported in the literature, it is unlikely the alveolar bone reacts differently to parafunctional loads. Roberts et al. report the bone around an implant may be remodeled at a rate of 500% each year after loading compared with normal trabecular physiologic remodeling around a tooth of 40% per year.18 The dramatic increase in remodeling rates may eventually lead to fatigue damage and resultant bone loss.19 This bone loss may be primarily at the crestal marginal regions or extend throughout the interface and cause implant failure.
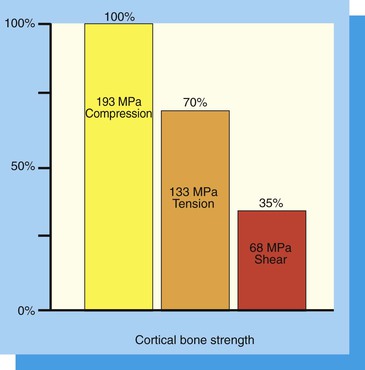
Force Type
Three types of forces may be imposed on dental implants within the oral environment: compression, tension, and shear. Bone is strongest when loaded in compression, 30% weaker when subjected to tensile forces, and 65% weaker when loaded in shear20 (Figure 13-5). Therefore, an attempt should be made to limit shear forces on bone because it is least resistant to fracture under these loading conditions. This is most important in regions of decreased bone density because the strength of bone is also directly related to its density.15 An increased width of an implant may decrease offset loads and increase the amount of the implant–bone interface placed under compressive loads. Hence, when forces are more tensile or shear in nature (as with cantilevers or angled loads), the implant diameter or implant number should be increased to compensate for the weakened bone state (Figure 13-6).
Force Direction
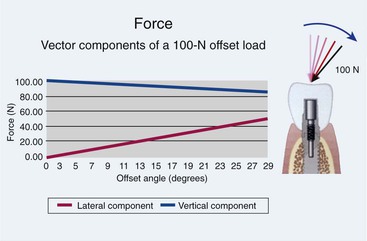
The direction of the load has a significant effect on the magnitude of compressive and lateral load components (tension and shear forces). Angled loads increase the amount of shear loads transmitted from the implant body to the bone, and the bone is weakest to shear-type loads.21 By increasing the angle of the load by only 15 degrees, the lateral component of that load (shear and tensile forces) is increased by 25.9%. Every degree of angled load increases the shear load component to the implants, which is the most damaging component of the load because the bone is weakest to shear. The forces to an implant body are typically greatest at the crestal bone interface.22 Angled loads to the implant prosthesis produce angled loads to the crest module of the implant and hence the marginal bone; therefore, the implant angulation is important to consider (Figure 13-7).
Under ideal conditions, the implant body should be oriented to provide long-axis compressive loads to the implant and to decrease shear loads to the crestal bone region. The occlusal forces are usually the greatest in centric occlusion. As such, the implant should be inserted perpendicular to the curve of Wilson and curve of Spee. Additionally, axial alignment places less stress on the overall implant system (i.e., abutment and abutment screw components) and decreases the risk of screw loosening and fatigue fractures of the implant or its components.
The anatomy of the mandible and maxilla often places significant constraints on the ability to surgically place root form implants for loading along their long axes. For example, resorptive patterns after prolonged edentulism exacerbates the normally occurring angulation challenges of the maxilla and mandible.23 In addition, bone undercuts constrain implant placement in either arch and thus affect load direction imposed on the implant. Almost all undercuts occur on the facial aspects of the bone, with the exception of the submandibular fossa in the posterior mandible.24 Implant bodies are often angled to avoid perforation of the bony undercut during insertion. These angulations increase biomechanical complications and may be reduced by increasing the diameter of the implant (or increasing the implant number).
The maxillary anterior region does not permit an ideal implant position even under ideal conditions. The natural maxillary anterior teeth are 12 to 15 degrees off the long axis of load, and the bone of the premaxilla is in a similar relationship after tooth loss. Therefore, implants in this region are often positioned with a greater relative angle to occlusal loads than any other region.21 To decrease the effect of an angled load on the implant, the implant body may be increased in diameter. It is interesting to note that the maxillary anterior teeth have greater diameter than the mandibular corresponding teeth. Whereas the lower anterior teeth are loaded in their long axis, the maxillary teeth are not. Hence, the diameter of the anterior natural teeth follows this biomechanical rationale.
Force Magnification
Force magnification further increases the stress beyond the usual conditions of load (e.g., a cantilevered prosthesis with a crown height greater than normal, an angled load, or parafunction).5 Multiple force magnifiers, such as a patient with parafunctional habits and an excessive crown height, may exceed the capability of any dental implant to withstand occlusal loads. Careful treatment planning with special attention to the implant position, implant number, occlusal loading, and an increase in implant size to increase functional surface area is indicated when a clinical case presents the challenge of force magnifiers.
A magnifier of force around an individual implant is also affected by the density of bone. Four distinct bone density categories within the maxilla and mandible exhibit a broad range of biomechanical strengths (i.e., ability to withstand physiologic loads).14 Significantly increased clinical failure rates in poor-quality, fine trabecular bone compared with denser bone have been documented worldwide by multiple independent clinical investigators for more than a decade, with failure rates as high as 35% with implants in D4 (type IV) bone.25–28 Bone density is directly related to bone strength, and D4 bone may be more than 10 times weaker than D1 bone and 70% weaker than D2 bone.15 Most implant failures in soft bone are from occlusal overload from a decrease in bone strength, a decreased bone–implant contact percentage, and the type of load transfer to the implant–bone interface on functional loading.29 Therefore, the effect of a resultant force is magnified as to its clinical result when placed in softer bone types.
Considerable effort should be made in the treatment plan to decrease the negative effects of compromised bone density, including implant number and size. The most important factor to decrease stress to the implant–bone interface is usually an increase in implant number, which dramatically increases the effective surface area over which the occlusal loads are dissipated and in turn decreases stress. Implant number also relates to implant position, which can effectively reduce cantilever lengths and subsequent harmful bending loads and shear stresses. After the implant number has been increased in the treatment plan, the next beneficial step to decrease the risk of overload is to increase the implant size, primarily in diameter.
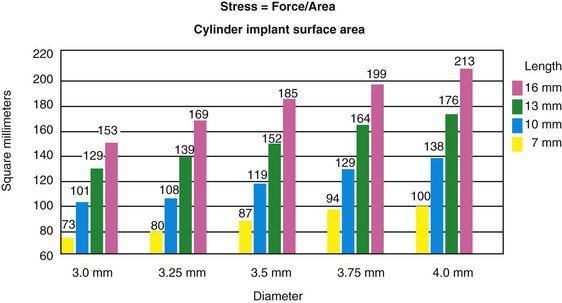
Surface Area
The surface area over which the occlusal forces are applied to the implant system is very relevant and is inversely proportional to the stress observed within the implant system (Stress = Force/Surface area). It can be clearly seen from this basic engineering equation, to reduce stress, the force must decrease or the surface area must increase. Therefore, an increase in implant size is beneficial to decrease the stress applied to the system. The size of an implant may be modified in either length or diameter.
Implant Length
Longer Implant Lengths
Most all dental implant manufacturers provide implants of various lengths. The most common sizes range between 7 and 16 mm (Figure 13-8). The length of the implant is directly related to the overall implant surface area when all other variables are constant. A 10-mm-long cylinder implant increases surface area by approximately 30% over a 7-mm-long implant and has about 20% less surface area than 13-mm-long implants30,31 (Figure 13-9). As a result, a common axiom has been to place an implant as long as possible. However, the length of the implant used for prosthetic support most often corresponds to the height of available bone in the edentulous site. Hence, shorter implants are often used in the posterior regions and longer implants in the anterior sections of the jaw (Figure 13-10).
Conventional thinking suggests that very long implants provide maximum functional surface area in a healed implant interface. However, when the length axiom is reevaluated, several challenges ensue. The available bone height is greater in the anterior regions of the mouth, especially the anterior mandible. Yet the bite forces are lower and the bone density is greater in these regions, especially in the mandible. The posterior regions have less bone height, and the implant cannot engage the dense opposing cortical plate because it is either nonexistent (maxilla) or beyond anatomical limits (neurovascular canal in the mandible). The posterior maxilla often has less height than the mandible, and the bone is less dense. As a result, the anatomic limitations result in shorter implants in the posterior region. On the other hand, many reports indicate similar survival rates in anterior and posterior regions when implants are greater than 10 mm in length.32
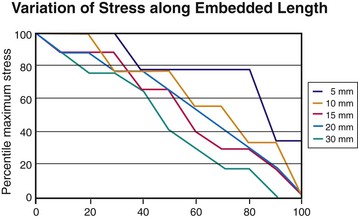
Implants longer than 15 mm have been suggested to provide greater stability under lateral loading conditions. However, reports suggest that increasing the length beyond a certain dimension may not reduce force transfer proportionately.22,33 Finite element analysis provides an analytical means to investigate the influence of implant length relative to functional surface area under such extreme loading conditions. Misch and Bidez placed cylindrical implants of different lengths in a computer bone model with ideal bone density and volume. The embedded implant body lengths were 5, 10, 15, 20, and 30 mm. A 10-mm crown height was designed above the level of bone, and a lateral force of 50 N was applied to the top of the 10-mm crown. For these loading conditions, the percentage of maximum stress was plotted against the percentage of embedded length (Figure 13-11). Peak stresses were not completely dissipated in the 5-mm-long implant model, with approximately 35% of the maximum stress still present at the apex of the implant. The 5-mm implant model, therefore, did not provide sufficient length for lateral force dissipation despite good bone density and volume and ideal crown height.
In the 10-mm implant model, 80% of maximum stress was dissipated in approximately 95% of the embedded length. For the 15- and 20-mm lengths, 80% of the maximum stress was dissipated in approximately 90% of the embedded length. For the 30-mm length, 80% of the maximum stress was dissipated in approximately 70% of the embedded length. In other words, the 15- to 30-mm implants did not reduce the stress in the crestal bone region and was able to constrain the stress within the length of the implant. Therefore, the length of the implant in favorable bone quality (e.g., D1 or D2 bone) and crown height may range from 10 to 15 mm with similar strain conditions. All implant lengths exhibited 80% to 100% of the stress in the crestal 40% of the implant length in this ideal bone simulant.
The results of this analysis point to the fact that the majority of the maximum stress generated by a lateral load can be dissipated as well by implants in the range of 10 to 15 mm in length, compared with implants in the range of 20 to 30 mm in length. In addition, the highest stresses were observed in the crestal bone regions, regardless of the implant length. This biomechanical analysis supports the opinion that longer implants are not necessarily better in good bone volume and density, such as that found in the anterior regions of the mandible. An implant length of 12 mm is usually sufficient under most patient force and bone density conditions. However, poorer bone densities provide a different strain condition.29
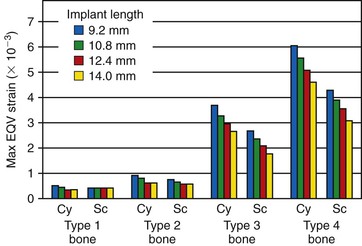
The ideal length of an implant may be affected by the bone density. The occlusal loads are primarily concentrated at the crest of the ridge in good-quality bone (i.e., D1, D2). In softer bone types (D3, D4), the stress contours around the implant body extend more apically. As a result, longer implants are a benefit in softer bone types. For example, in a three-dimensional finite element analysis study by Tada et al., the strain around an implant in D1 bone is similar for all implant length from 9.2 to 14 mm.34 In type 2 bone, the implant length also did not influence the amount of strain at the implant–bone interface. However, the strain around an implant body in D3 bone had two to three times more strain than the harder bone types, and the 9.2-mm length had almost 30% more strain than the 14-mm-long implant. In type 4 bone, the amount of strain around a 9.2-mm implant was four times more than the D1 and D2 bone simulant model, and the 14-mm-long implant was three times more (Figure 13-12). In addition, longer implants become more fixated in soft bone during surgical placement and may resist more movement during initial healing. This aspect decreases the failure rate during healing time for implants in soft bone. Hence, implants up to 15 mm long are suggested in the softest bone types, especially when cantilevers or lateral loads exist on the prosthesis.
Bicortical stabilization in the anterior mandible, a rationale often cited for longer implants, is not needed in D1 bone, which is primarily homogeneous cortical bone.14 Bone overheating is a primary cause of surgical failure in dense bone, and attempting to engage the opposing cortical plate in D2 bone and preparing a longer osteotomy may result in overheating the cortical bone.35 In D3 bone, a threaded implant may not readily engage the denser bone of the apical cortical plate, and the implant threads may strip along the rest of the osteotomy because it is in a fine trabecular bone type. In addition, after the implant–bone interface is formed, excessively long implants do not transfer stress to the apical region because most of the stresses are transmitted within the crestal 7 to 9 mm of bone (except in the softer bone types), and therefore longer than 12-mm implants are often not needed in the anterior mandible.22
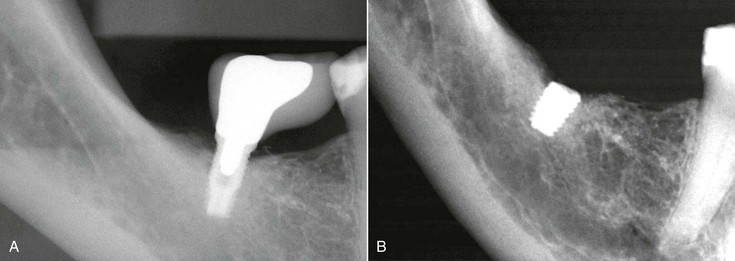
The anterior mandible is also the region that has less bite force and the implants are more long axis loaded. It should be noted that the incisal edge of an anterior mandibular tooth is often more facial than the inferior cortical plate (Figure 13-13). As a result, a longer implant in the anterior mandible with abundant bone often engages the lingual cortical plate, not the inferior border. Because this landmark is more superior, the surgeon may inadvertently perforate the lingual plate and increase the risk of bleeding, swelling of the floor of the mouth, and postoperative complications.
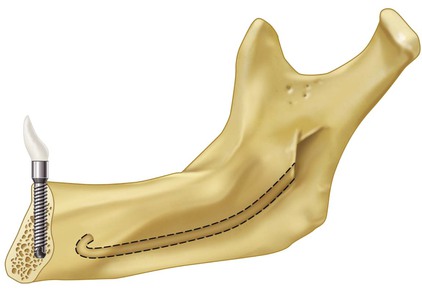
D3 and D4 bone are primarily present in the posterior regions of the jaw, where less available bone height is observed compared with the anterior regions. Mandibular inferior alveolar nerve repositioning has been cited as an acceptable clinical treatment to facilitate placement of longer implants in the posterior mandible (Figure 13-14). However, this advanced surgical procedure represents an increased risk for paresthesia and is often not indicated, especially when other treatment options are available.36

To place the longest implants in the maxillary posterior regions, a sinus graft is often required. Sinus grafts have been shown to grow bone into the graft from the surrounding walls of bone, and bone does not form under the sinus mucosa for several years. Therefore, the apical end of longer implants will not benefit from the sinus bone graft procedure for some time, and the crest of the bone below the graft will remain at greater risk. However, it should be noted that implants in D4 poor-density bone (as often found in the posterior maxilla) benefit when they are at least 12 mm in length. Implants up to 15 mm may be advantageous in conditions of higher force factors; therefore, a sinus graft is often required in this region.
Increasing surface area primarily by length in the posterior regions of the jaws often requires advanced grafting or surgical techniques in either the maxilla or mandible. When incisal guidance eliminates all lateral forces and no cantilevers are present on the prostheses, the implant length requirement may be reduced, especially in good-quality bone. Implant lengths greater than 12 mm offer few benefits under these conditions and often increase the surgical risks of the procedure.
Shorter Implant Lengths
Different risk factors for implant longevity have emerged over the years. A review of the literature related to implant failure and implant length was published by Goodacre et al. in 2003.32 Many implant manufacturers provide implants in 7-, 8.5-, and 10-mm lengths. In the majority of articles addressing implant length, implants smaller than 10 mm have increased failure rates. In the reports summarized, the failure rates of these shorter implants were 15% compared with a 3% failure rate of longer implants. The failure is even more apparent when the literature reviews implants smaller than 10 mm in the posterior regions of partially edentulous patients. Fewer than half of the clinical reports had survival rates higher than 90%, and more than half of the reports had implant failure higher than 19.7%6,28,37–46 (Table 13-1).
TABLE 13-1
Short Implants (Literature Review Below 90%)
| Author (Year) | No. of Implants | Success Rate (%) | Implant System |
| Jemt and Lekholm40 (1995) | 298 | 76 | Brånemark |
| Minsk et al.28 (1996) | 50 | 84 | Brånemark (six systems) |
| Saadoun and Le Gall41 (1996) | 15 | 79 | Steri-Oss |
| De Bruyn et al.47 (1999) | 9 | 87 | Screw-Vent |
| Winkler et al.38 (2000) | 152 | 81 | Screw-Vent (six designs) |
| Naert et al.6 (2002) | 1168 | 67 | Brånemark |
| Weng et al.39 (2003) | 97 | 79 | 3i |
| Total implants: 1889 | |||
| Average success rate: 80.3% | |||
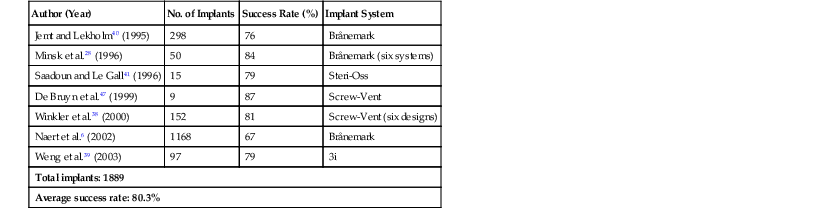
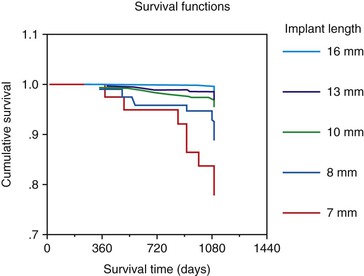
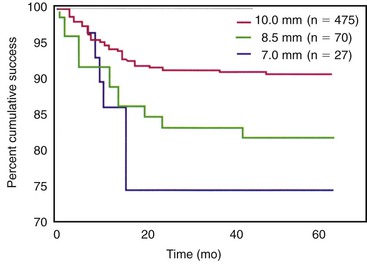
A review of several of the multicenter reports of short implants is noteworthy. Minsk et al. reported the results of a training center in 1996, with 80 different operators using six different systems over a 6-year period.28 Implants 7 to 9 mm in length were reported to have a 16% failure rate. The overall survival rate of all longer lengths was 95%. Winkler et al. published a multicenter report over a 3-year period in 2000.38 The implant survival was directly related to the length of the implant. Whereas the 7-mm-long implants had a 26.4% failure rate, 16-mm implants demonstrated only a 2.8% rate of failure. Whereas implants of 8 mm had a 13% failure rate, 10-mm implants in the report failed at a rate of 10.9%, and the 13-mm implants failed 5.7% of the time (Figure 13-15). A multicenter report by Weng et al. in 2003 found that 60% of all failed implants were 10 mm or less in length.39 The overall failure rate of all implants in the study was 9%, yet the 7-mm implant failed 26% of the time, and the 8.5-mm implant had a 19% failure rate (Figure 13-16). Naert et al. reported in the literature on clinical outcomes of short dental implants.6 Whereas implants shorter than 10 mm had a survival rate average of 81.5%, longer implants had a survival rate higher than 95%.
It should be noted the failure rates in most of these reports are not surgical failures or failures to osseointegrate. The failures associated with short implants most often occurred after prosthetic loading. In other words, the surgical success was not affected by implant length. However, after the prostheses were in function, an increase in early loading failure was observed, especially within the first 6 to 18 months.39
Four reasons linked to biomechanics may explain why the short implant may have a higher failure rate after loading compared with longer implants48:
1. Less surface area to dissipate occlusal loads
2. Higher bite forces in posterior regions
Rationale of Short Implants
The height of existing available bone is often used by the implant dentist to determine the implant length after adequate width and mesiodistal space are confirmed. The height of available bone is measured from the crest of the edent/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses