Class II Correction with an Intermaxillary Fixed Noncompliance Device
Twin Force Bite Corrector
Aditya Chhibber, Madhur Upadhyay, Ravindra Nanda
Morphogenesis and the development of the face is one of the most complex processes in human development. The role of nature versus nurture has long been debated. Proponents of genetic theory claim that growth patterns may arise from the activation and repression of genes that regulate the metabolic activity of differentiated cells, while proponents of epigenetic theories believe that growth control factors may lie in sutures,1 cartilage,2 or functional matrices3 surrounding the craniofacial structures. Others believe that it is the confluence of genetics and external environmental factors that ultimately determines the size, shape, and location of craniofacial structures.4
The role of heredity in the development of one’s phenotypical appearance has been examined through observational studies of monozygotic or dizygotic twins, who have greater similarity in appearance than unrelated individuals.5 The question always has been whether and to what degree the external environment can influence the genetically predisposed size, shape, and direction of growth of craniofacial structures. While some studies6 suggest that the presence of malocclusion can be greatly influenced by environmental factors, others believe its cause is multifactorial.5 Even though it is reported that both Class II and Class III malocclusions may have strong familial tendency,7,8 it may be difficult to estimate the influence of environmental factors in modifying craniofacial growth because the heritability studies of occlusion are typically based on twins and siblings who did not receive orthodontic treatment.
Class II malocclusion is one of the most common problems presenting to orthodontists. Skeletally, a prognathic maxilla, a retrognathic mandible, or a combination of the two is a possible etiology for this malocclusion. Studies in the literature9–12 report that Class II malocclusion is more commonly associated with mandibular retrognathism than with maxillary prognathism. Stahl et al.13 reported that features of a skeletal Class II occlusion develop early in the deciduous dentition and do not tend to self-correct with age, implying that some sort of intervention is necessary to achieve correction. Depending on the patient’s growth status, treatment options commonly include use of functional appliances or fixed functional appliances (FFAs) to enhance mandibular growth, headgear to restrict maxillary growth, camouflage by extraction of upper and/or lower premolars, or surgical correction of the underlying skeletal discrepancy in patients in whom facial growth has been completed.14 The goal of either orthodontic intervention or orthognathic surgery is generally to improve the patient’s dental and facial esthetics, dental function, self-image, and quality of life.
The term functional appliance refers to a group of appliances that posture the mandible forward in an attempt to stimulate mandibular growth. Historically, the use of functional appliances began with Kingsley’s vulcanite biteplate but probably was first propagated by Anderson with the use of the Activator appliance.15 Since then, numerous functional appliances have been reported in the literature, with the most popular being the Activator, Bionator, and the Twin Block appliance. However, despite the use of functional appliances for more than a century, there is still considerable debate over the effectiveness of such mandibular anterior repositioning appliances in stimulating skeletal mandibular growth.16 Studies17–19 on experimental animals such as rats, mice, and primates depict a clear increased mandibular growth potential with the use of such appliances. However, similar experiments with these bite-jumping appliances to enhance mandibular skeletal growth in human subjects did not yield comparable results. The results of randomized clinical trials20–22 have shown that with the use of functional appliances there is an initial increase in the mandibular growth response that is greater than that seen in the control sample; however, in the long-term, when patients treated with functional appliances were compared to untreated control subjects, the difference in the overall mandibular length was statistically insignificant.
Typically a functional appliance is advocated for a minimum of 12 hours per day for 6 to 9 months to observe dentoskeletal changes. Thus patient compliance is critical to the success of removable functional appliances.23,24 In general, the factors associated with patient compliance are age, nature of the treatment delivered, and psychosocial characteristics of the individual patient. It has been reported that compliance with treatment is better in adults than in children and that younger children are more compliant with treatment than are adolescents.25 Since most growth modulation procedures are undertaken in the adolescent phase, proficient patient compliance may be difficult to obtain in certain patients. Removable appliances such as headgear and functional appliances are usually rejected by patients due to discomfort, pain, restriction, and constraints on physical activity and movement.26 In a study on patient compliance with functional appliances monitored microelectronically, Sahm et al.27 reported that the patients wore the functional appliances far less than recommended to obtain dentoskeletal changes.
To eliminate patient compliance for Class II correction, the use of non–patient-compliance-based FFAs was first propagated by Emil Herbst in 1905 with the Herbst appliance. The appliance never really gained popularity until Pancherz revived it in the 1970s. Since then there have been numerous modifications of the rigid Herbst appliance28 and various other FFAs29–32 have also been reported in the literature. These FFAs may be broadly classified as rigid, flexible, and semirigid fixed functional appliances. The major difference between functional appliances and FFAs is that the mandible is forcefully postured in an anterior position with FFAs with the help of inter-arch anchorage using the maxillary denture base as the anchor unit.
Using the concept of equilibrium,33 it can be understood that when a rigid FFA is placed in the mouth, the appliance is in static equilibrium. This essentially means that when there is a mesial or forward directed force on the lower arch, there exists an equal and opposite distal or backward directed force on the upper arch. This effect has been proved by cephalometric studies as the “headgear effect”34,35 of FFAs. Apart from the “skeletal” effects on the denture bases, effects on the dentition such as retroclination of maxillary incisors,36 proclination of mandibular incisors,36–38 distalization of upper molars and mesialization of lower molars,37,38 and clockwise rotation of the occlusal plane38 have also been observed with FFAs. Thus Class II correction with FFAs is reported to be due to a combination of skeletal and dental effects.
Diagnosis and Treatment Planning
To accurately diagnose a patient, detailed information is gathered through a chief complaint, medical and dental history, clinical examination, and records that include extraoral and intraoral photographs, models, and radiographic images. An accurate interpretation of the data obtained from all clinical examinations and diagnostic records is made to develop a problem list, on the basis of which treatment objectives are identified and an individualized treatment plan is formulated for each patient.
Cephalometric Analysis
Orthodontists usually judge skeletal and dental relationships through cephalometric analysis, in which the patient’s characteristics are compared to norms that differ among patient populations based on age, sex, and race. Cephalometric analysis can be performed to evaluate the cranial base, the relationship of the maxilla to the cranial base, the mandible’s size and position relative to the cranial base, the relationship between the maxilla and the mandible, the vertical dimension, maxillary and mandibular dentition, and soft tissue. Table 13-1 provides an example of such analysis. Although the absolute numbers obtained in a cephalometric analysis provide basic information regarding an individual patient, there may be limitations to restricting diagnosis of a patient to numbers only.
TABLE 13-1
Cephalometric Facial Analysis of Patient EE
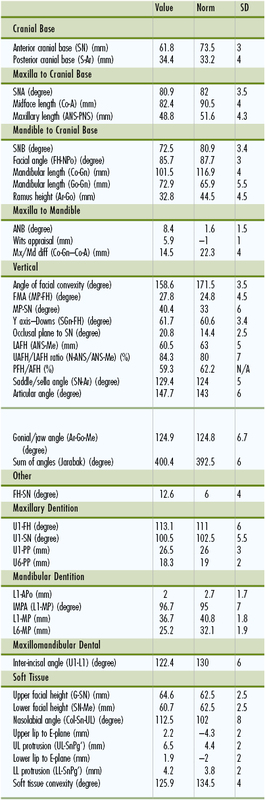
A, A point; AFH, anterior facial height; ANB, A point nasion B point; ANS, anterior nasal spine; APo, A point to pogonion; Ar, articulare; Co, condylion; Col, columella; FH, Frankfurt plane; G, glabella; Gn, gnathion; Go, gonion; IMPA, incisor mandibular plane angle; L1, lower incisor; L6, lower molar; LAFH, lower anterior facial height; LL, lower lip; Me, menton; MP, mandibular plane; N, nasion; PFH, posterior facial height; Pg’, soft tissue pogonion; PNS, posterior nasal spine; PP, palatal plane; SD, standard deviation; Sn, subnasale; SN, sella-nasion; SNA, sella-nasion A point; SNB, sella-nasion B point; U1, upper incisor; U6, upper molar; UAFH, upper anterior facial height; UL, upper lip.
Cephalometric facial analysis analyzing cranial base, maxilla to cranial base, mandible to cranial base, maxilla-mandibular relation, vertical relation, maxillary and mandibular dentition, and soft-tissue analysis.
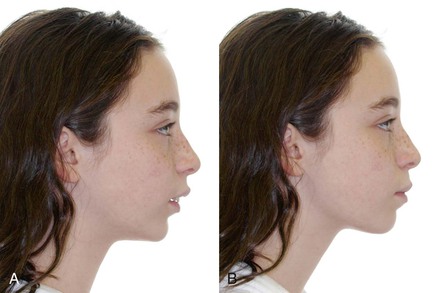
A relatively easy, quick, and reliable way to assess the outcome with a functional appliance or FFA is a visualized treatment objective (VTO). The patient is asked to posture the mandible forward, obtaining anterior incisal contact with the posterior teeth in a Class I or super Class I relationship. If the profile of the patient improves, it indicates that the patient may be a good candidate for functional jaw orthopedics (Fig. 13-1). If on posturing the mandible forward the profile does not show improvement, the patient may not be an ideal candidate for a functional appliance and other methods for Class II could be considered or a prefunctional orthodontic phase may be required (Fig. 13-2). As a general rule, a functional appliance (FFA) is most ideally indicated in growing Class II patients who are essentially mandibular deficient, with an average to flat mandibular plane angle and upright lower anterior teeth over the mandibular basal bone with minimal to moderate crowding.
Twin Force Bite Corrector Appliance
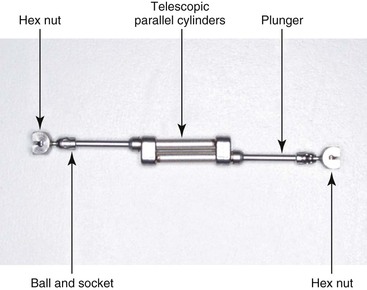
The Twin Force bite corrector (TFBC) appliance39–42 is a hybrid fixed push–type, semirigid FFA clamped to archwires in both the upper and the lower arches bilaterally. Each unit is made up of two 15-mm telescopic parallel cylinders (Fig. 13-3). Within the cylinder is a nickel-titanium (Ni-Ti) coil spring that is activated when the patient occludes. A plunger is incorporated at the end of each cylinder on both ends. At the end of each plunger, hex nuts are present to attach the appliance to the archwires mesial to the upper molars and distal to the lower canine. At full compression a force of approximately 210 g is delivered on each side by compression of the coil spring. This force is synergistic to the indirectly applied force by the muscles of mastication due to the forced anterior repositioning of the mandible.
Looking at the individual force components exerted by the appliance, there is an intrusive and distal component of force on the maxillary posterior segment and a mesial and intrusive force component on the lower anterior segment. Since the point of force application is away from the estimated center of resistance (CRES) of the maxillary and mandibular denture bases,43 a clockwise moment is generated (Fig. 13-4, A). A unique feature of the TFBC appliance is that since the point of force application is closer to the CRES of the maxillary dentition, compared to other traditional FFAs where the point of force application in the maxillary arch is distal to the upper molar (Fig. 13-4, B), a lesser clockwise moment is generated with the appliance on the maxillary arch. Also, since the appliance is clamped to the archwire, the intrusive component of the spring force is probably redistributed along the entire denture base. In addition, since the force is applied buccal to the CRES of the maxillary molar, estimated to be at the center of the trifurcation of the maxillary molar, a buccal expansive force is experienced (Fig. 13-5).
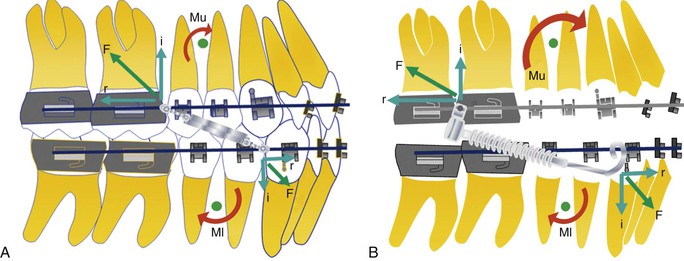
Figure 13-4 Force system with (A) Twin Force bite corrector (TFBC) appliance and (B) conventional fixed functional appliance (FFA). F, Total force; i, vertical (intrusive) component; Ml, moment created on the lower arch; Mu, moment created on the upper arch; r, horizontal component.
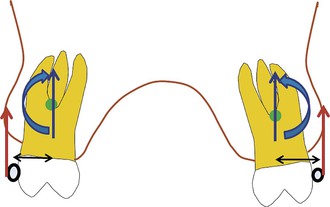
Figure 13-5 Force system with Twin Force bite corrector (TFBC) appliance in transverse dimension. Force applied by the TFBC appliance is depicted in red. Equivalent force system at the center of resistance of the molar is depicted in blue.
Treatment Protocol
Pre-treatment records for a patient are obtained (Fig. 13-6) and after the initial leveling and alignment phase, the archwires are progressively increased to 0.019 × 0.025-inch stainless steel in the upper arch and 0.021 × 0.025-inch stainless steel in the lower arch (Fig. 13-7, A–C). Both archwires are cinched to consolidate the arches into a single unit to avoid any spaces developing or flaring of the incisors. Additionally, to minimize lower incisor flaring, MBT bracket prescription with –6-degree torque lower anterior brackets is advised. A 0.032-inch × 0.032-inch transpalatal arch is placed to counteract the buccal forces exerted by the TFBC appliance. The standard TFBC version is attached by the hex nuts to the archwires mesial to the maxillary molars and distal to the lower canines, posturing the mandible forward in an anterior edge-to-edge relationship (Fig. 13-7, D–F).

Figure 13-6 Pre-treatment records of Class II patient treated with the Twin Force bite corrector (TFBC) appliance. A–C, Facial views. D–H, Intraoral views.

Figure 13-7 A–C, Clinical setup before placement of an appliance. D–F, Placement of the Twin Force bite corrector (TFBC) appliance. G-I, Removal of the appliance with overcorrection achieved.
After 3 to 4 months of appliance placement, the patient usually has an overcorrected Class I molar and canine relationship. This helps to overcompensate for any relapse that may occur after appliance removal (Fig. 13-7, G–I). Appropriate finishing and detailing is performed and the patient is subsequently debonded (Fig. 13-8). The retention protocol involves a fixed lingual retainer for the lower arch and a removable wrap-around retainer for the upper arch.
Effects of the TFBC Appliance
In an unpublished study44 conducted at the University of Connecticut Health Center to analyze the effects of the TFBC appliance, a comparison was done between 20 subjects who received the TFBC appliance and an untreated Class II sample derived from the Denver growth study. The patients were matched for age, sex, and maturation status. The skeletal and dental results (Figs. 13-9 and 13-10, respectively) showed that during the 3-month period of using the TFBC appliance, A point in the maxilla moved 0.5-mm posteriorly under the distal force of the appliance and 1.7-mm inferiorly by the clockwise moment acting on the upper arch (compared to 0.1-mm anterior and 0.4-mm inferior movement in the control sample). The absolute length of the maxilla (anterior nasal spine [ANS]–posterior nasal spine [PNS]) was similar in both groups. The palatal plane rotated clockwise 0.5 degree in the TFBC sample compared to 0.1 degree in the control sample. The mandibular length (Ar-Pog) increased significantly—2.1-mm in the TFBC sample compared to 0.7-mm in the control sample—which could be attributed to a combination of growth and forward posturing of the mandible under the influence of the TFBC appliance. Dentally, the upper incisors showed distal crown tipping of –7.0 degrees in the TFBC sample compared to 0.1 degree mesial tipping in the control sample. The upper molar distalized –0.7-mm and intruded –1.1-mm in the TFBC group; in the control group the upper molar mesialized 0.3-mm and extruded 0.2-mm. The lower incisors flared 7.3 degrees and mesialized 2.6-mm in the TFBC group compared to no movement in the control group. The lower molar mesialized 1.8-mm in the TFBC group whereas in the control group the molar mesialized only 0.2-mm. Therefore the Class II correction was due to a combination of skeletal and dental effects.
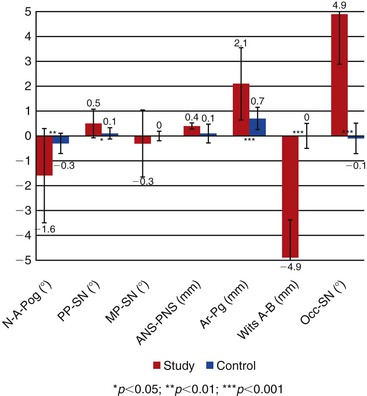
Figure 13-9 Skeletal observations of a study sample treated with the Twin Force bite corrector (TFBC) appliance compared to an untreated Class II control sample matched for age, sex, and cervical vertebral maturation stage (CVMS). ANS-PNS (mm), Anterior nasal spine to posterior nasal spine; Ar-Pg (mm), articulare to pogonion; MP-SN (˚), mandibular plane (gonion–gnathion) to sella-nasion; N-A-Pog (˚), nasion – A point – pogonion; Occ-SN (˚), occlusal plane to sella-nasion; PP-SN (˚), palatal plane to mandibular plane (gonion-gnathion); Wits A-B (mm), Wits occlusal plane changes.
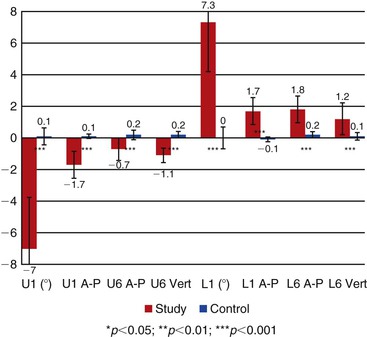
Figure 13-10 Regional superimposition observations of the dental effects of the Twin Force bite corrector (TFBC) appliance compared to the untreated Class II control sample. L1 (˚), Angular change in lower incisor inclination; L1 A-P, linear changes in lower incisor position; L6 A-P, linear changes in lower molar position; L6 Vert, vertical changes in lower molar position; U1 (˚), angular change in upper incisor />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses