Treatment of Masticatory Muscle Disorders
“MASTICATORY MUSCLE PAIN IS THE MOST COMMON SYMPTOM OF TMD. SO WHY DO SO MANY CLINICIANS CALL THIS ‘TMJ’ WHEN THE JOINTS ARE NOT THE SOURCE OF THE PROBLEM?”
—JPO
THIS IS THE FIRST OF THREE chapters addressing the treatment of the various temporomandibular disorders (TMDs). One chapter is devoted to each of the major disorders. In each chapter the individual subclasses are briefly outlined according to etiology, history, and clinical findings. (A more detailed description may be found in Chapters 8 and 10.) Following this review, appropriate definitive and supportive therapy is discussed and a clinical algorithm is presented to assist the clinician. Finally, at the end of each chapter, several clinical case reports are presented.
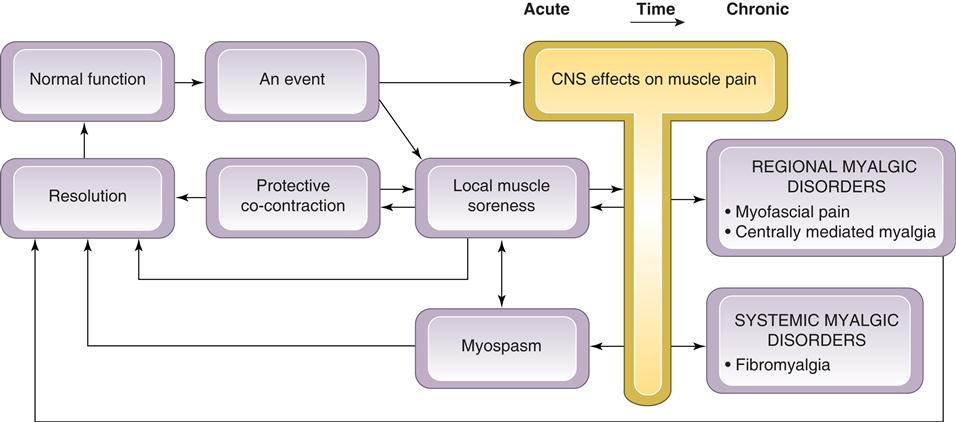
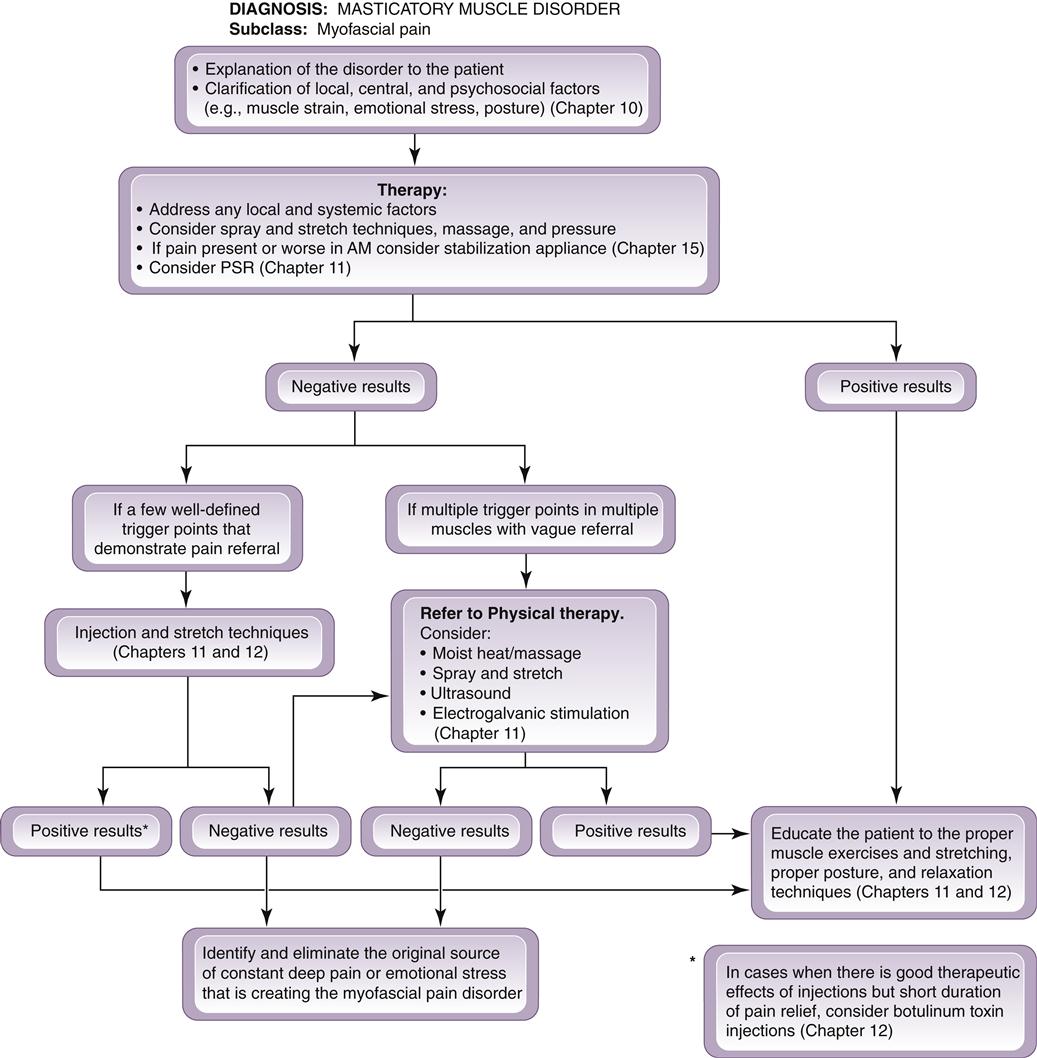
The predominant complaint of patients with masticatory muscle disorders is myalgia. This is often reported as having a sudden onset and being recurrent. The pain originates in the muscles; therefore any restriction of mandibular movement is due to the extracapsular muscular pain. All masticatory muscle disorders are not the same clinically. As discussed in Chapter 8, there are at least five different types. Being able to distinguish among them is important because the treatment of each is different (Figure 12-1). The five types are protective co-contraction (muscle splinting), local muscle soreness, myofascial (trigger-point) pain, myospasm, and chronic centrally mediated myalgia. Two other types are also discussed in this chapter. They are centrally mediated motor disorders and fibromyalgia. The first three conditions (protective co-contraction, local muscle soreness, and myofascial pain) are commonly seen in the dental office. The other three are less frequently seen but must be recognized so that they are not treated inappropriately.
Some muscle disorders occur and resolve in a relatively short period of time (co-contraction and local muscle soreness). When these conditions are not resolved, more chronic pain disorders may result. Chronic masticatory muscle disorders become more complicated and treatment is generally oriented differently than for acute problems. With time, the central nervous system (CNS) can play an important role in maintaining the muscle disorder (myofascial pain, myospasm, chronic centrally mediated myalgia, and centrally mediated motor disorders). It therefore becomes important that the clinician be able to distinguish acute muscle disorders from chronic disorders so that proper therapy can be applied. Fibromyalgia is a chronic myalgic disorder that presents as a systemic musculoskeletal pain problem; it must be recognized by the dentist and best managed by referral to appropriate medical personnel.
Protective Co-contraction (Muscle Splinting)
Protective co-contraction is the initial response of a muscle to altered sensory or proprioceptive input or injury (or threat of injury). This response has also been called protective muscle splinting1 or coactivation.2 It has been demonstrated by several researchers.3–7 Co-contraction is a common phenomenon and can be observed during many normal functional activities, such as bracing the arm in attempting a task with the fingers.2 In the presence of altered sensory input or pain, antagonistic muscle groups seem to fire during movement in an attempt to protect the injured part. Therefore pain felt in the masticatory system can produce protective co-contraction of masticatory muscles.3 Clinically this results in increased activity of the jaw-opening muscles during closure of the mouth as well as an increase in closing muscle activity during mouth opening. One should remember that protective co-contraction is not a pathologic condition but a normal physiologic response of the musculoskeletal system.7
Etiology
The following events are responsible for protective co-contraction:
History
The key to identifying protective co-contraction is that it immediately follows an event; therefore the history is very important. Protective co-contraction remains for only a few days. If it is not resolved, local muscle soreness is likely to follow. The history will reveal one of the following:
Clinical Characteristics
The following clinical characteristics are present with protective co-contraction:
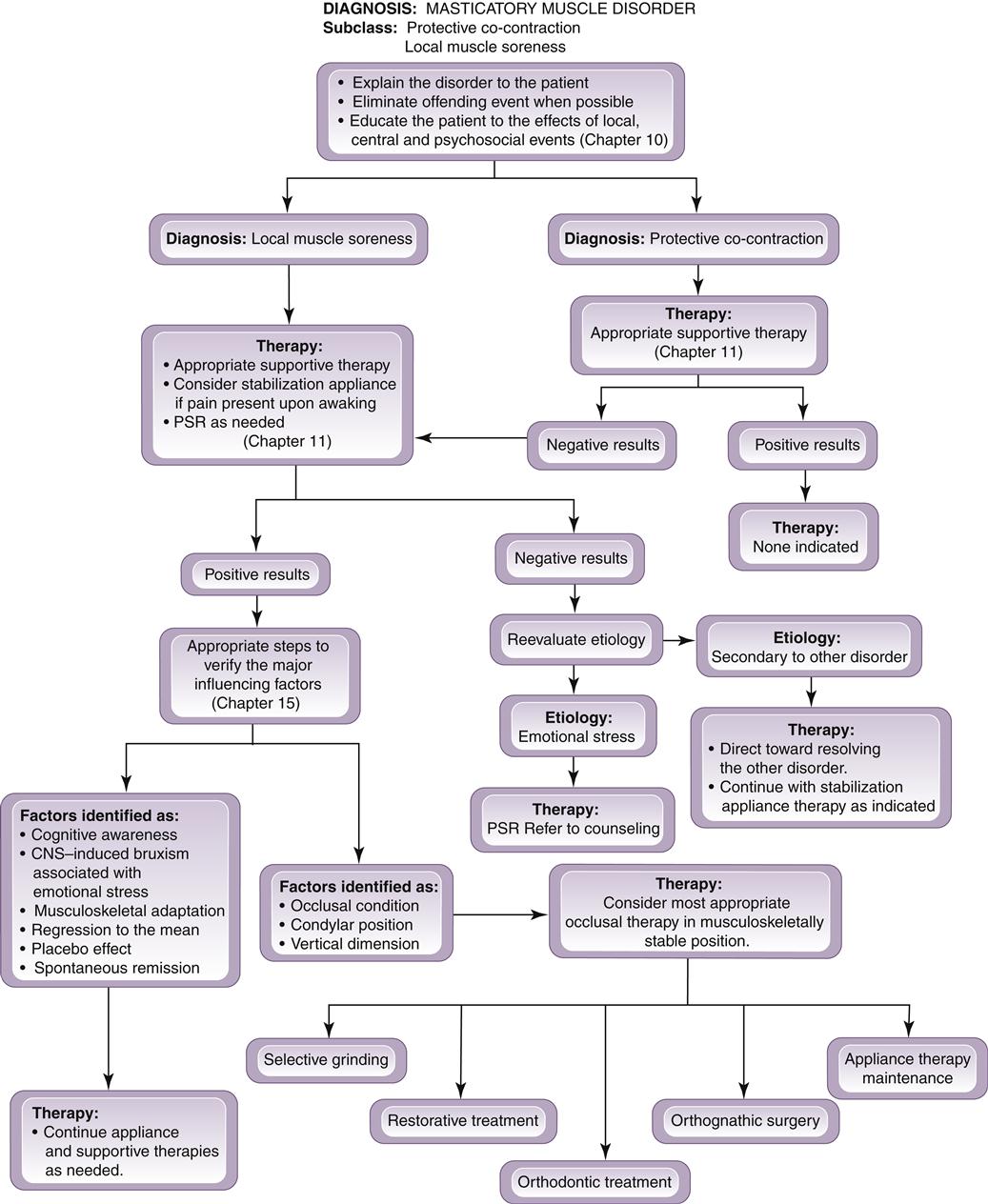
Definitive Treatment
It is important for the clinician to remember that protective co-contraction is a normal CNS response and that therefore there is no indication to treat the muscle condition itself. Treatment should instead be directed toward the reason for the co-contraction. When co-contraction results from trauma, definitive treatment is not indicated, since the etiologic factor is no longer present (Figure 12-2).
When co-contraction results from the introduction of a poorly fitting restoration, definitive treatment consists of altering the restoration to harmonize with the existing occlusion. Altering the occlusal condition to eliminate co-contraction is directed only at the offending restoration and not the entire dentition. Once the offending restoration has been eliminated, the occlusal condition is returned to its preexisting state, which resolves the symptoms (Figure 12-3).
If the co-contraction is the result of a source of deep pain, then the pain must be appropriately addressed (Figure 12-4). If an increase in emotional stress is the etiology then appropriate stress management, such as physical self-regulation (PSR) techniques, should be instituted.
Supportive Therapy
When the etiology of protective co-contraction is tissue injury, supportive therapy is often the only type of treatment rendered. It begins with instructing the patient to restrict use of the mandible to within painless limits. A soft diet may be recommended until the pain subsides. Short-term pain medication (nonsteroidal anti-inflammatory drugs, or NSAIDs) may be indicated. Simple physical self-regulation techniques (Chapter 11) can also be initiated. Generally, however, muscle exercises and other physical therapies are not indicated. Co-contraction is usually of short duration; if the etiologic factors are controlled, the symptoms will resolve over several days.
Patient information sheets are provided in Chapter 16. They can be given to patients when they leave the clinic to enhance their understanding of their problems. These sheets also offer information that can help patients help themselves.
Local Muscle Soreness (Noninflammatory Myalgia)
Local muscle soreness is a primary noninflammatory myogenous pain disorder. It is often the first response of the muscle tissue to continued protective co-contraction and therefore the most common acute muscle pain disorder in dental practice. Although co-contraction represents a CNS-induced muscle response, local muscle soreness represents a change in the local environment of the muscle tissues. It represents the initial response to overuse, which we think of as fatigue.
Etiology
History
The history reported by a patient with local muscle soreness will include one of the following:
Clinical Characteristics
Local muscle soreness presents with the following clinical characteristics:
Definitive Treatment
Since local muscle soreness produces deep pain, which often creates secondary protective co-contraction, cyclic muscle pain will commonly develop over time. Therefore the primary goal in treating local muscle soreness is to decrease sensory input (such as pain) to the CNS (Figure 12-5). Such a decrease in sensory input is achieved by the following steps:
1. Eliminate any ongoing altered sensory or proprioceptive input.
2. Eliminate any ongoing source of deep pain input (whether dental or other).
3. Provide patient education and information on self-management (physical self-regulation). The following four areas should be emphasized:
b. The patient should be encouraged to use the jaw within the painless limits so that the proprioceptors and mechanoceptors in the musculoskeletal system are stimulated. This activity seems to encourage return to normal muscle function.9 Therefore careful and deliberate use of the muscle can promote resolution of local muscle soreness. The patient should be encouraged to use the muscles, but only within painless limits. Complete lack of muscle use is not appropriate for patients experiencing local muscle soreness.
c. The patient should be encouraged to reduce any nonfunctional tooth contacts. This begins by asking the patient to become more aware of those subconscious times when the teeth are in contact and then developing techniques to eliminate these contacts (cognitive awareness).10,11 The patient is instructed to keep the lips together and the teeth apart. Most patients can develop the skills necessary to achieve voluntary disengagement of the teeth during the waking hours.
d. The patient should be made aware of the relationship between increased levels of emotional stress and the muscle pain condition. When emotional stress appears to be a significant contributor to the local muscle soreness, techniques that reduce stress and promote relaxation should be encouraged.12
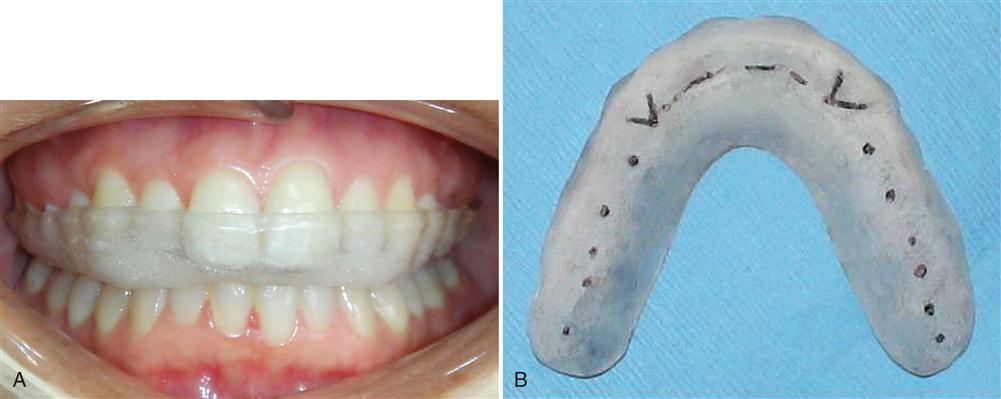
4. Although patients can often control daytime tooth contacts, most have very little control of nocturnal tooth contacts.13 When nighttime clenching or bruxing is suspected (early-morning pain), it is appropriate to fabricate an occlusal appliance for nighttime use.14–19 An occlusal appliance is an acrylic device that fits over the teeth of one arch and provides precise occlusal contact with the opposing arch (Figure 12-6). A stabilization (CR) appliance will provide even occlusal contacts when the condyles are in their anterosuperior position resting on the articular discs against the posterior slopes of the articular eminences (providing musculoskeletal stability). Eccentric guidance is developed on the canines only. The patient is instructed to wear the appliance at night during sleep and only occasionally during the day if it helps to reduce the pain. The part-time use of this type of appliance for local muscle soreness has been demonstrated to be more effective in reducing muscle pain than full-time use.20 Its fabrication is discussed in Chapter 15.
The occlusal appliance has been advocated by the dental profession for years, and there are data suggesting that it can be helpful in reducing masticatory muscle pain disorders.19–24 However, as the profession demands more evidence-based studies, we learn that the occlusal appliance may not be as helpful as one might first have thought.25,26 We must encourage more controlled clinical trials to better understand the effects of appliances on TMD symptoms. However, since a well-fabricated stabilization appliance is a reversible therapy with few negative effects, it can be considered in the management of local muscle soreness.
Supportive Therapy
Supportive therapy for local muscle soreness is directed toward reducing pain and restoring normal muscle function. In most cases, pain can be easily controlled by the definitive treatments discussed above.
For many years muscle relaxants were used for this muscle pain.27 We have found, however, that muscle relaxants do not seem to have a great effect on this muscle pain.28,29 They can centrally relax and sedate the patient, which may have some benefit, but they are not always very useful. These medications are not helpful because the muscles are not really being contracted with local muscle soreness (no increased reading on the electromyogram [EMG]; see Chapter 8). Therefore these medications should be used sparingly and, when used, the patient should be warned of potential drowsiness (no automobile driving).
Manual physical therapy techniques such as passive muscle stretching and gentle massage may also be helpful. Relaxation therapy may also be helpful if increased emotional stress is suspected.
Local muscle soreness should respond to therapy in 1 to 3 weeks. When this therapy is not effective, the clinician should consider the possibility of a misdiagnosis. If a reevaluation of the pain condition reinforces a masticatory muscle disorder, one of the more complicated myalgic disorders should be considered.
Patient information sheets are provided in Chapter 16. These sheets can be given to patients when they leave the clinic to enhance their understanding of their problems. These sheets also offer information that can help patients help themselves.
Myospasms (Tonic Contraction Myalgia)
Myospasm is an involuntary CNS-induced tonic muscle contraction often associated with local metabolic conditions within the muscle tissues. Although this condition can certainly affect the muscles of mastication, it is not as common as was once thought.
Etiology
History
The patient reports a sudden onset of restricted jaw movement usually accompanied by muscle rigidity.
Clinical Characteristics
The following clinical characteristics are associated with myospasms:
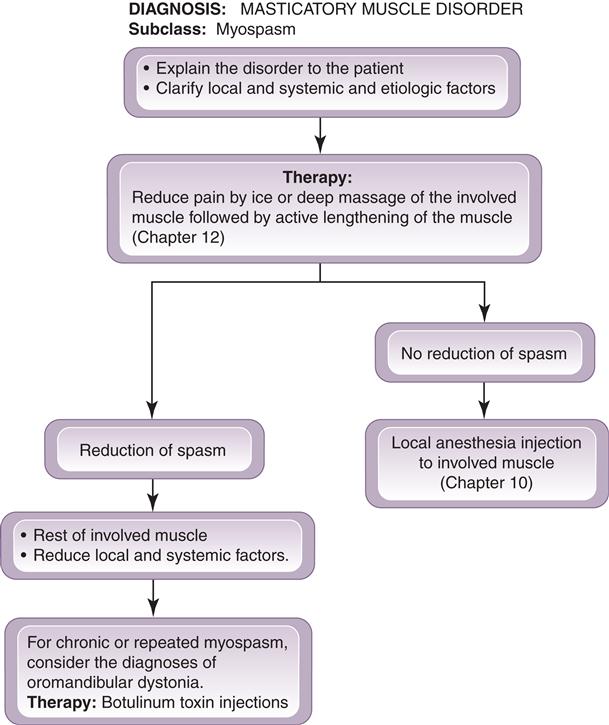
Definitive Treatment
Two treatments are suggested for acute myospasms. The first is directed immediately toward reducing the spasm itself while the other addresses the etiology (Figure 12-7).
1. Myospasms are best treated by reducing the pain and then passively lengthening or stretching the involved muscle. Reduction of the pain can be achieved by manual massage (Figure 12-8), vapocoolant spray, ice, or even an injection of local anesthetic into the muscle in spasm. Once the pain is reduced, the muscle is passively stretched to full length. If an injection is used (and often it is the most effective manner to stop a persistent spasm), 2% lidocaine without a vasoconstrictor is recommended.
On occasion myospasms can occur repeatedly with no identifiable etiologic factors. When this occurs in the same muscle, the condition may actually represent an oromandibular dystonia. Dystonias are repeated uncontrolled spastic contractions of muscles; these conditions are often thought to have central etiologies. Dystonias are managed differently than acute and occasional myospasms; they are discussed in a separate section at the end of this chapter, under Oromandibular Dystonias.
Supportive Therapy
Often physical therapy techniques are the key to managing myospasms. Soft tissue mobilization such as deep massage and passive stretching are the two most important immediate treatments. Once the myospasm is reduced, other physical therapies, such as muscle conditioning exercises and relaxation techniques, can be helpful in addressing local and systemic factors. Pharmacologic therapy is not usually indicated because of the acuteness of the condition.
Myofascial Pain (Trigger-Point Myalgia)
Myofascial pain is a regional myogenous pain condition characterized by local areas of firm, hypersensitive bands of muscle tissue known as trigger points.32 This condition is also called myofascial trigger-point pain. The presence of central excitatory effects is common with this myalgic disorder. The most common effect is referred pain, often described by the patient as a tension-type headache.
Etiology
Although we lack a complete understanding of this disorder, the following etiologic factors have been related to myofascial pain:
History
The patient’s chief complaint is often focused on the heterotopic pain and not the actual source of pain (the trigger points). Therefore the patient will direct the clinician to the headache (tension-type) or to protective co-contraction. If the clinician is not careful, he or she will likely direct treatment to the secondary pains, which, of course, will fail. The clinician must have the knowledge and diagnostic skills necessary to identify the primary source of pain so that proper treatment can be selected.
Clinical Characteristics
An individual suffering with myofascial pain will commonly reveal the following clinical characteristics:
Definitive Treatment
The treatment of myofascial pain is directed toward the elimination or reduction of etiologic factors (Figure 12-9). The clinician can accomplish this with the following treatment protocol:
1. Eliminate any source of ongoing deep pain input in an appropriate manner according to the etiology.
2. Reduce the local and systemic factors that contribute to myofascial pain. This treatment is individualized to the patient’s needs. For example, if emotional stress is an important part of the disorder, stress management techniques are indicated. When posture or work position contributes to myofascial pain, attempts should be made to improve these conditions. Physical self-regulation techniques (Chapter 11) are very useful in managing myofascial pain.
3. If a sleep disorder is suspected, proper evaluation and referral should be made. Often low dosages of a tricyclic antidepressant, such as 10 to 20 mg of amitriptyline before bedtime, can be helpful (Chapter 11).
Spray and Stretch
One of the most common and conservative methods of eliminating trigger points is with a spray-and-stretch technique.41–43 This technique consists of spraying a vapocoolant spray (e.g., fluoromethane) on the tissue overlying the muscle with a trigger point and then actively stretching the muscle. The vapocoolant spray provides a burst of cutaneous nerve stimulation that temporarily reduces pain perception in the area (Chapter 2). Once the tissue has been sprayed, the muscle is stretched to its full length painlessly (Figure 12-10). The vapocoolant spray is applied from a distance of approximately 18 in. in the direction of the referred symptoms. The passive stretching of the muscle must be performed without producing pain. If pain is elicited, the muscle will likely protectively cocontract, resulting in more muscle activity (cyclic muscle pain). The precise technique for each muscle has been described by Simons and Travell.44 Their text should be an essential part of the armamentarium of any clinician treating myofascial pain.
Pressure and Massage
In some instances massage or manipulation of a trigger point can cause it to be eliminated. Care must be taken, however, not to produce pain. It has been demonstrated41,45,46 that increased pressure applied to a trigger point can also be an effective technique. The pressure is increased to approximately 20 lb and is maintained for 30 to 60 s. If this technique produces pain, it must be stopped, since the pain can reinforce cyclic muscle pain.
Ultrasound and Electrogalvanic Stimulation
Physical therapy modalities such as ultrasound and electrogalvanic stimulation (EGS) can sometimes be useful in managing trigger points.47 Ultrasound produces deep heat to the area of the trigger point, causing local muscle relaxation.48 Low-voltage EGS can be used to rhythmically stimulate or pulse the muscles. This therapy leads to reduced muscle activity and encourages muscle relaxation.49,50 Although there is little research to verify the efficacy of these techniques, they are generally very conservative and may be useful.
Injection and Stretch
Another effective method of eliminating a trigger point is by using injection techniques (Figure 12-11). Most commonly, local anesthetic is injected, and then the muscle can be stretched painlessly.51–53 Although the anesthetic is useful in reducing pain,54 it is apparently not the most critical factor in eliminating the trigger point.55,56 Rather, the mechanical disruption of the trigger point by the needle seems to provide the therapeutic effect.
Local anesthetic is used for two reasons: First, it eliminates the immediate pain, allowing full painless stretching of the muscle. Second, it is diagnostic; in other words, once a trigger point is anesthetized, not only is the local pain reduced but the referred pain is also eliminated. Thus the clinician can gain valuable information regarding the source of referred pain. For example, the anesthetic injection of a trigger point in the sternocleidomastoid will immediately eliminate a referred temporal headache and enable the true source of the headache pain to be identified. The immediate shutdown of pain relates to the interruption of the central excitatory effects produced by the deep pain (the trigger point). This suppression of pain may be in part related to the endorphin system.57
When local anesthetic injections are indicated, 1% procaine appears to be the least myotoxic. However, this medication is no longer packaged for use in dental syringes; thus when a dental syringe is to be used, 2% lidocaine will be appropriate. A vasoconstrictor should not be used for muscle injections. A long-acting anesthetic such as bupivacaine (Marcaine) is not indicated for muscle injections because of the associated risk of increase myotoxicity, especially when such an agent is used with steroids.58 Only a small amount of lidocaine is needed to treat a trigger point. One dental carpule is adequate for two or even three trigger-point injections, depending on the size of the muscle being injected. A half carpule is indicated for a trapezius trigger point; less than a third is adequate for a temporalis trigger point.
Trigger point injections may be an appropriate treatment for myofascial pain when it is found that the injections provide the patient with prolonged relief even after the anesthetic effect has resolved. Repeated injections may be indicated if the period of pain relief grows longer between each injection. If trigger-point injections fail to provide any prolonged pain relief, there is no reason to repeat the procedure.
As with any injection, the four rules described in Chapter 10 should always be followed. The anatomic considerations and injection technique for each muscle are described by Simons and Travell51; their text should be consulted by clinicians interested in treating myofascial pain with trigger-point injections.
Supportive Therapy
As already discussed, various physical therapy modalities and manual techniques are used to treat myofascial pain. These techniques are listed under definitive treatments because they address the actual elimination of trigger points. The most important are soft tissue mobilization and muscle conditioning techniques.
Pharmacologic therapy such as treatment with a muscle relaxant can be helpful, but it will not usually eliminate the trigger points. A medication such as cyclobenzaprine (Flexeril), 10 mg before sleep, can often reduce pain, but the trigger points must still be treated as discussed above. Muscle relaxants help to convert an active trigger point into a latent or dormant trigger point but may not necessarily eliminate it. Analgesics may also be helpful in interrupting the cyclic effect of pain.
Posture is another possible contributor to myofascial pain.32 Muscles that are maintained at shortened length tend to develop trigger points more than others. Daily stretching to full length can be beneficial in keeping them pain-free. This is especially true in the neck and shoulder region. Regular exercise should always be encouraged.33,59,60
Patient information sheets are provided in Chapter 16. These sheets can be given to patients when they leave the clinic to enhance their understanding of their problems. These sheets also offer information that can help patients help themselves.
Centrally Mediated Myalgia (Chronic Myositis)
Centrally mediated myalgia is a chronic, continuous muscle pain disorder originating predominantly from CNS effects that are felt peripherally in the muscle tissues. This disorder presents clinically with symptoms similar to those of an inflammatory condition of the muscle tissue; therefore it is sometimes referred to as myositis.
Etiology
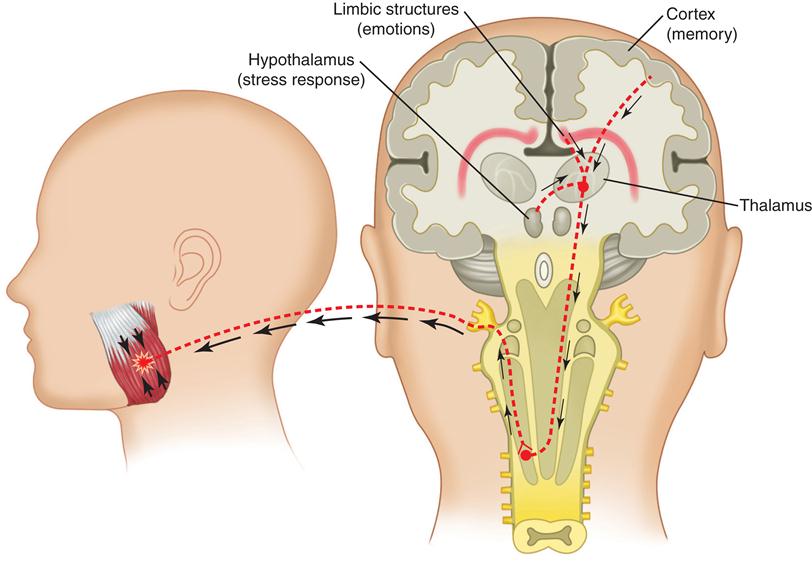
The etiology of centrally mediated myalgia is, as the name suggests, the CNS and not the more commonly associated structures of the masticatory system. As the CNS becomes exposed to prolonged nociceptive input, brainstem pathways can functionally change. This can result in an antidromic effect on afferent peripheral neurons. In other words, neurons that normally carry information only from the periphery into the CNS can now be reversed to carry information from the CNS out to the peripheral tissues. This is likely to occur through the axonal transport system.61 When this occurs, the afferent neurons in the periphery can release nociceptive neurotransmitters such as substance P and bradykinin, which in turn cause nociception and pain in the peripheral tissues. This process is called neurogenic inflammation.62–66
The important concept to remember is that the muscle pain reported by the patient with chronic centrally mediated myalgia cannot be treated by managing the painful muscle tissue itself. Management must be directed to the central mechanisms, an idea that can be very foreign to dentists.
Chronic centrally mediated myalgia may be caused by the prolonged input of muscle pain associated with local muscle soreness or myofascial pain. In other words, the longer the patient complains of myogenous pain, the greater the likelihood of chronic centrally mediated myalgia. However, is it also possible that other central mechanisms may play a significant role in the etiology of centrally mediated myalgia, such as chronic upregulation of the autonomic nervous system, chronic exposure to emotional stress, or other sources of deep pain input (Figure 12-12).
History
The patient reports a constant primary myogenous pain condition usually associated with a prolonged history of muscle complaints (for months and even years).
Clinical Characteristics
The following six clinical characteristics are common to centrally mediated myalgia:
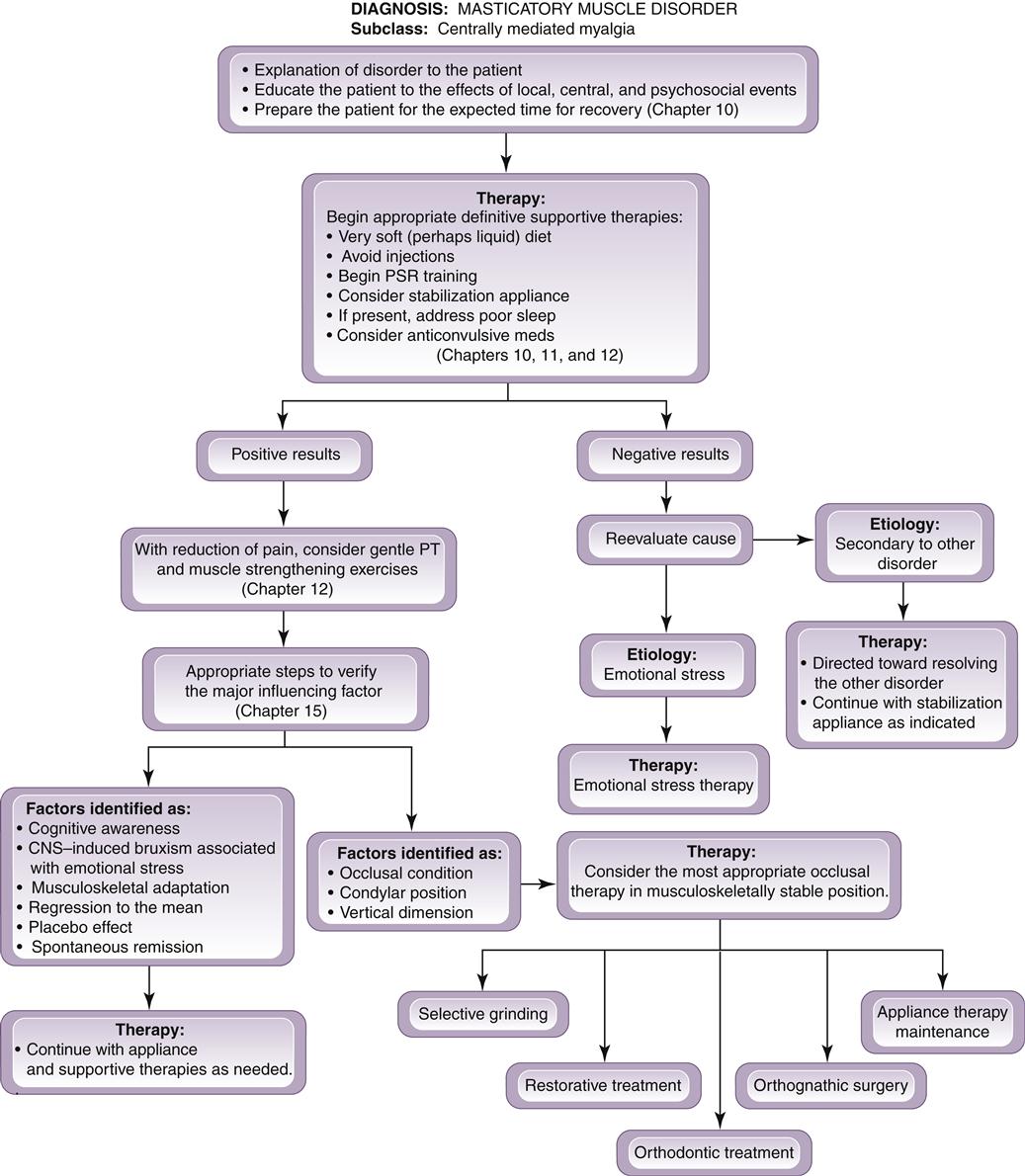
Definitive Treatment
The clinician must initially recognize the condition of chronic centrally mediated myalgia, since the outcome of therapy will not be as immediate as with treating local muscle soreness. Neurogenic inflammation of muscle tissue and the chronic central sensitization that produced it often take time to resolve. When the diagnosis of chronic centrally mediated myalgia is established, the clinician should discuss with the patient the expected results and the length of time needed for recovery. The patient should be informed that reduction of symptoms is initially slow and not dramatic. Patients must be aware of this so as to minimize disappointment in treatment results. As etiologic factors are controlled, neurogenic inflammation will resolve and symptoms will slowly decrease.
As is true with local muscle soreness, four general treatment strategies are followed in the patient with chronic centrally mediated myalgia. However, although somewhat similar, they are not identical. In fact, therapy for local muscle soreness will often aggravate chronic centrally mediated myalgia (Figure 12-13). Therefore if the clinician is treating local muscle soreness and the symptoms become greater, it is likely that the condition is actually chronic centrally mediated myalgia. The following regimen should then be used:
3. Disengage the teeth. As with local muscle soreness, the management of chronic centrally mediated myalgia is assisted by disengaging the teeth both voluntarily and involuntarily. Voluntary disengagement is accomplished by the physical self-regulation techniques discussed in Chapter 11. Involuntary disengagement of the teeth (nocturnal bruxism) is achieved by a stabilization appliance in the same manner as with local muscle soreness (Chapter 15).
4. Begin using an anti-inflammatory medication. Since local muscle tissue is inflamed, it is quite appropriate to prescribe an anti-inflammatory. An NSAID, such as ibuprofen, is a good choice and should be given on a regular basis (600 mg four times a day) for 2 weeks so that blood levels are sufficiently elevated to achieve a clinical effect. Irregular “as needed” doses will not achieve the desired effect. Ibuprofen is also analgesic; it can thus help to reduce cyclic muscle pain, which can propagate chronic centrally mediated myalgia. As previously discussed, the patient should be questioned for any history of stomach complaints and monitored for any gastric symptoms during the course of therapy. If these symptoms are present, a COX2 inhibitor should be considered (Chapter 11).
5. Consider management of sleep. As with other centrally mediated pain conditions, the quality of the patient’s sleep can be affected negatively. When this occurs, low dosages of a tricyclic antidepressant such as 10 mg of amitriptyline at bedtime can be helpful in reducing symptoms67–69 (Chapter 11). The mechanism is thought to be related to either an improvement in the quality of sleep67,68,70 or a positive effect on the descending inhibitory system. Cyclobenzaprine (Flexeril), 10 mg at bedtime, may also be helpful to facilitate sleep and reduce pain.71–73
6. Since the CNS is a major player in this type of pain condition, it is likely that the central neurons will have become sensitized. Therefore treatment oriented toward reducing this central sensitization can be helpful. The clinician may consider some of the anticonvulsant medications, such as gabapentin (Neurontin) or pregabalin (Lyrica) (Chapter 11). These medications may also assist in sleep, since one of their common side effects is drowsiness.
Supportive Therapy
Early in the treatment of chronic centrally mediated myalgia physical therapy modalities should be used cautiously since any manipulation can increase the pain. Sometimes moist heat can be helpful (Figure 12-14). For other patients, ice seems to be more helpful. The patients will clearly relate which is best for them. As the symptoms begin to resolve, ultrasound therapy and gentle stretching can begin. If pain is increased by the therapy, the intensity should be decreased.
Since the treatment of chronic centrally mediated myalgia often takes time, two distinct conditions can develop: hypotrophic changes to the muscle (atrophy) and myostatic contracture. These occur as a result of the lack of use of the elevator muscles (temporalis, masseter, medial pterygoid). Once the acute symptoms have resolved, activity of the muscles should slowly begin. Some gentle isometric jaw exercise will be effective for increasing the strength and use of the muscles (Figure 12-15). Passive stretching is also helpful in regaining the original length of the elevators (Chapter 11). The treatment of chronic centrally mediated myalgia is a slow process and cannot be rushed. If physical therapy is introduced too quickly, the condition can worsen.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses