General Considerations in the Treatment of Temporomandibular Disorders
“TMD IS A COMPLEX AND MULTIFACTORIAL CONDITION; SO ALSO ARE OUR PATIENTS.”
—JPO
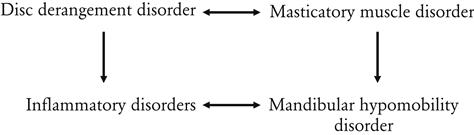
Interrelationships of Various Temporomandibular Disorders
The accurate diagnosis and treatment of TM disorders (TMDs) can be difficult and confusing. This is often true primarily because the patient’s symptoms do not always fit into one classification. In many instances several classifications seem to be appropriate because in reality the patient is suffering from more than one disorder. In fact, in many patients, not only do several conditions coexist, one disorder may actually contribute to another. It is appropriate, therefore, when more than one disorder appears to be present, to attempt to distinguish the primary from the secondary disorder. For example, a patient may complain of right temporomandibular joint (TMJ) pain 2 weeks after a fall that traumatized the joint. The pain has been present for 12 days, but during the past week it has been aggravated by a decrease in mouth opening associated with muscle discomfort. The primary diagnosis is a traumatic injury to this joint, whereas the secondary diagnosis is protective co-contraction or local muscle soreness associated with the response of the muscles to restricted movement of the painful joint. During treatment both diagnoses must be considered and appropriately managed.
The interrelationship of the various TMDs must always be considered in the evaluation and treatment of patients. Sometimes it is nearly impossible to identify which disorder preceded which. Often the evidence to determine such an order can be obtained only from a thorough history. The following examples demonstrate the complex interrelationships between several TMDs:
A patient suffering from a masticatory muscle disorder such as local muscle soreness or myofascial pain will commonly report a chief complaint of myalgia. These muscle conditions are likely to increase the tonicity of the elevator muscles, creating an increase in interarticular pressure of the joint. The condition may be further aggravated by hyperactivity of the superior lateral pterygoid muscle (bruxism), which can accentuate a subclinical disc derangement disorder (increased clicking).

Another patient complains of an early disc derangement disorder. If pain is associated with it, secondary muscle co-contraction can result in an attempt to prevent painful movements. If the muscle co-contraction becomes protracted, local muscle soreness can result. In this instance, a disc derangement disorder has created a masticatory muscle disorder.

When some disc derangement disorders progress, the bony articular surfaces of the joint may undergo changes. In other words, disc derangement disorders can lead to inflammatory disorders of the joint.
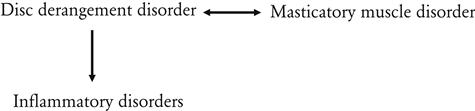
When masticatory muscle disorders persist, limited mandibular movement can become protracted and lead to chronic mandibular hypomobility disorders. Likewise, inflammatory disorders can also induce chronic mandibular hypomobility disorders.
Trauma is another condition that affects all these disorders. Trauma to any structure of the masticatory system can either cause or contribute to most of the other TMDs.
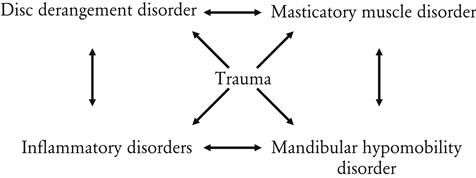
This diagram begins to depict the complicated interrelationships that may exist among the various TMDs. It demonstrates why many patients have symptoms that are associated with more than one disorder and how these relationships can make diagnosis and treatment decisions very difficult.
Treatment of Temporomandibular Disorders
The treatments that have been suggested for TMDs vary enormously over a great spectrum of modalities. In order for the clinician to confidently select an appropriate treatment he or she should demand adequate scientific evidence to support its use. This support should be found in evidence-based literature documenting the successes and failures of a described treatment. Unfortunately this is not always the case. There are numerous published articles suggesting success of a variety of treatment options that may not be soundly substantiated with scientific evidence. In an attempt to demonstrate this confusion, the present author went to the dental literature and developed a list of treatment options that have received at least some scientific support. When the list grew to 49, the search was ended. No wonder the profession is so confused regarding the management of TMDs.
It is also worth noting that the popularity of certain treatment methods can be found to be geographically regionalized. It is highly unlikely that this is appropriate, since epidemiologic studies do not report regionalization of any particular TMD. It can also be noted that treatment selection correlates strongly with the specialty of the doctor whom the patient has consulted. If the patient comes to an orthodontist, orthodontic treatment is likely to be administered; if to an oral surgeon, a surgical procedure is likely; if to a prosthodontist, occlusal therapy is likely to follow. There is no reason why patients with similar problems should receive different treatments in different regions. Nor is there any reason why patients with similar problems should be treated differently by different specialties.
Another interesting observation is that some treatments presented as new and revolutionary were actually presented to the profession years earlier and found to have little or no value. It seems that once a generation has passed, someone rediscovers the treatment, introduces it as new, and clinicians accept the idea and begin using this treatment for their patients. This is certainly unfortunate since, as a result, our patients must suffer and endure additional expense and sometimes irreversible dental procedures that are doomed to fail.
The question that must be asked is how can so many different types of therapies have publications that suggest they are helpful in managing TMD? There are no simple answers to this question. There are, however, certain considerations that may help to explain this controversy. Here are a few:
1. There is a lack of adequate scientific evidence for soundly relating therapy to treatment effects. Although many published studies have investigated TMDs, most are methodologically flawed. Only recently has the dental profession begun to demand sound, evidence-based research methodology. The controlled double-blinded clinical trial is the standard for clinical research, and studies of this kind are rare in the field of TMD. The profession must encourage more of these studies to advance the body of knowledge in the field.1
2. Significant research efforts can begin only with agreement regarding the specific diagnostic categories of TMD. As has been stressed in this text, the most important task of the clinician is to establish the proper diagnosis. Different disorders respond differently to different treatments. Therefore it is only with proper diagnosis that proper therapy can be selected. This fact makes diagnosis extremely important. In the past, many studies described their treatment group as “TMJ patients.” This broad description does not increase the body of knowledge, since the therapy investigated may affect one subcategory and not another. In order to evaluate the effects of a particular treatment, these therapies must be tested in patient groups with very specific common diagnoses. When the clinician is evaluating current research, he or she must be critical of the patient groups tested in the study.1
In 1992 the first attempt to group temporomandibular disorders into common research diagnostic categories was presented (The Research Diagnostic Criteria, or RDCs).2 These categories were developed and significant attempts were made to validate each.3 This was exactly what we needed to enhance the study of TMDs. Although these diagnostic criteria could separate most TMDs from non-TMDs, categorizing specific TMDs was not effective. The reason for this lies in the many groups of musculoskeletal disorders that make up TMDs. In this author’s opinion, the RDCs were not helpful in specifically differentiating the subcategories of TMD and therefore have contributed little to the management of TMDs. The RDCs continue to be revised in an attempt to improve their usefulness.4–6
5. The pain intensity of many musculoskeletal disorders can vary greatly over time. In other words, there may be great pain on some days and little or none on others. This variation may occur for months. Because the symptoms vary, the patient’s perceived need for treatment can change. The patient will most commonly seek treatment for the condition when the symptoms are most intense. At this time the dentist offers treatment and the symptoms begin to resolve. The question that must be asked is “Did the patient’s symptoms resolve because of the therapeutic effect of the treatment or did they resolve merely because they returned back to a lower level associated with the natural fluctuation of the symptoms?” This is a very important concept and is referred to as “regression to the mean.”7 Once one appreciates this concept, it can be clearly seen that many treatments can appear to be successful when actually they have no real therapeutic value. In order to study the true therapeutic value of a treatment, it must be compared over time with no treatment at all. This is why random controlled clinical trials are needed. Unfortunately these types of studies are rare in the field of TMD. The concept of regression to the mean is discussed in more detail in Chapter 15.
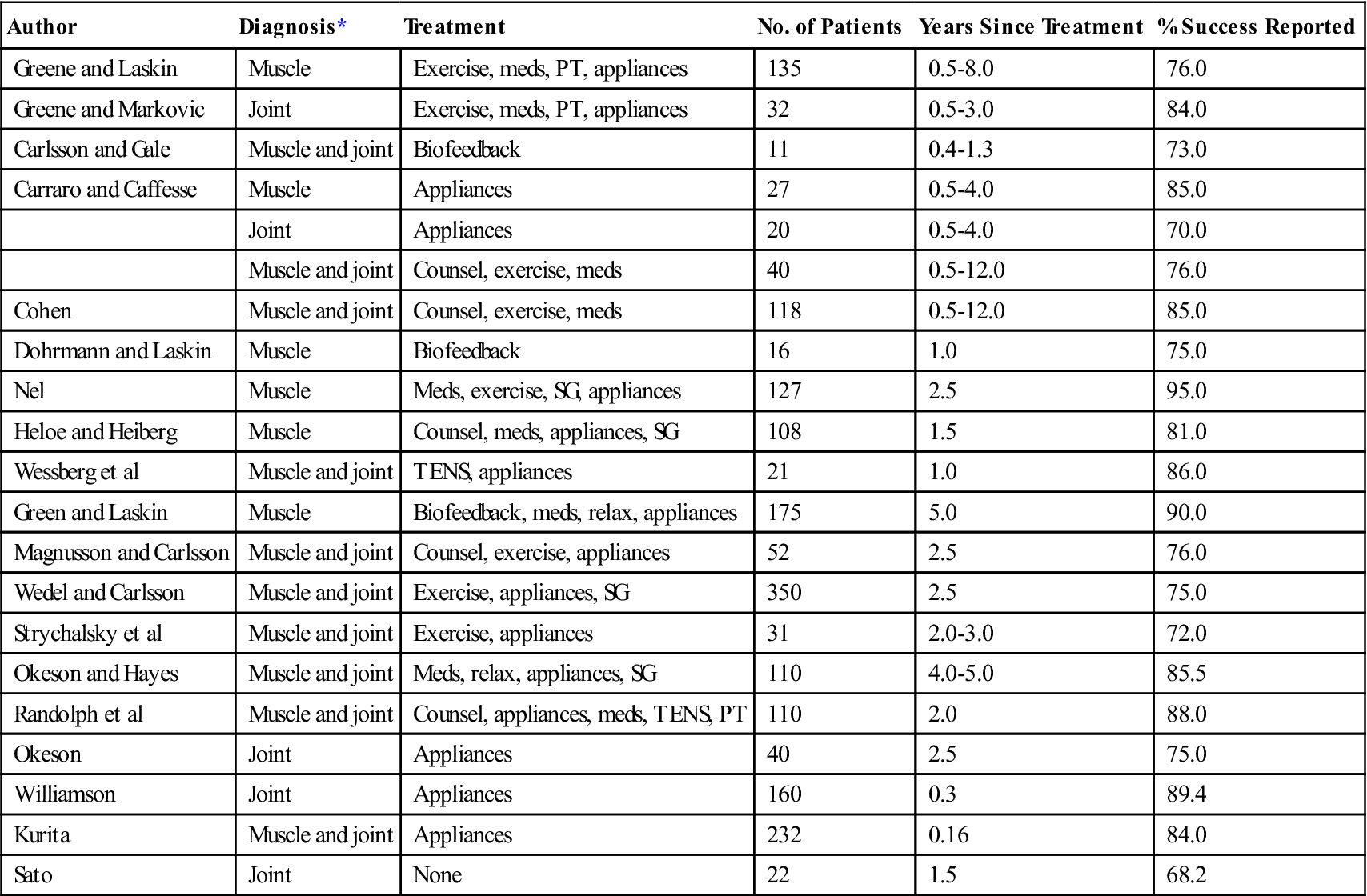
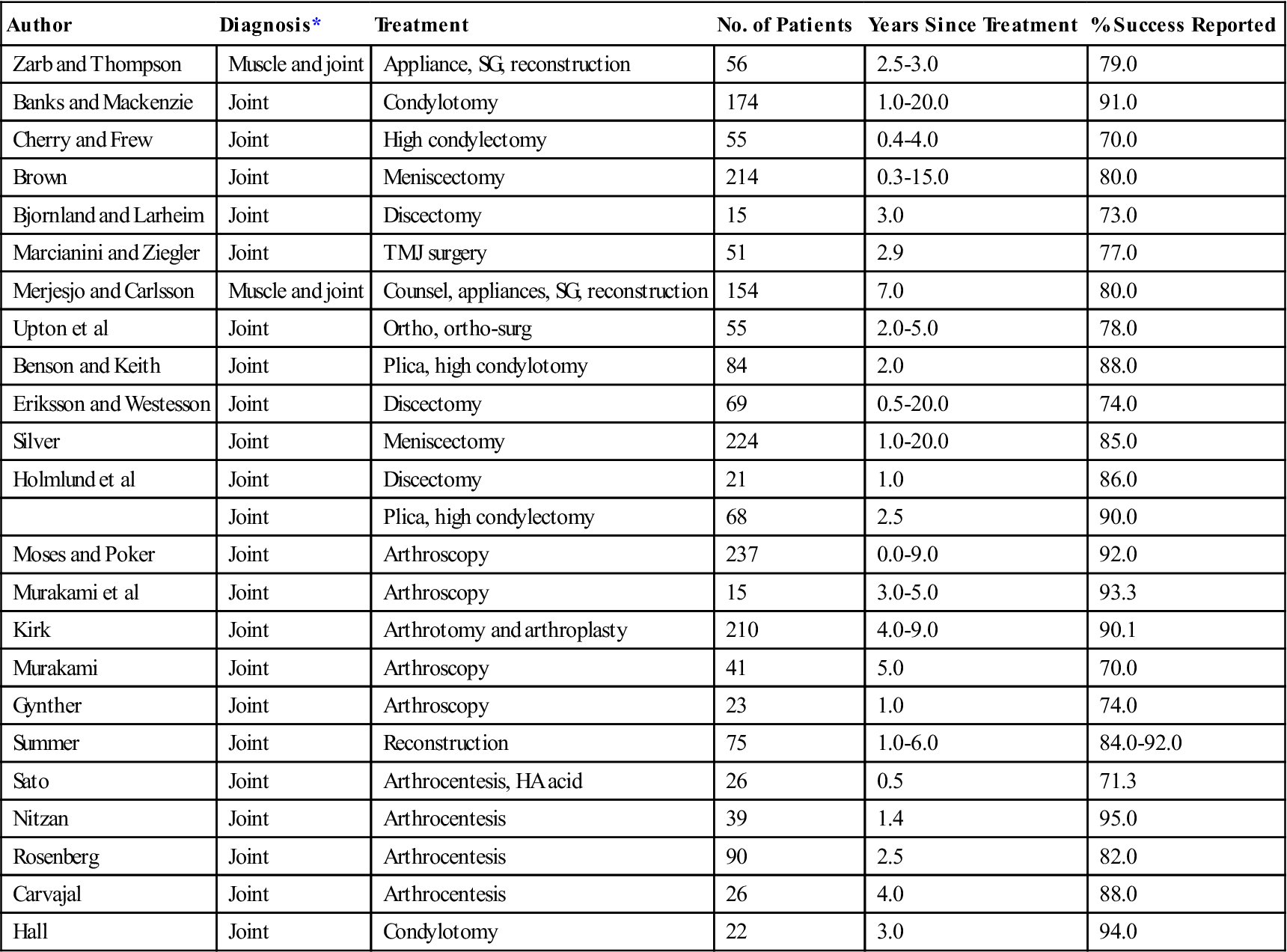
Tables 11-1 and 11-2 show the results of a group of long-term studies8–48 on the treatment of various TMDs. Long-term treatment studies should give the most accurate information regarding the effectiveness of treatment. The studies have been placed in one of two categories: those that provided basically conservative, reversible therapy and those that provided rather nonconservative, irreversible therapy.
TABLE 11-1
Long-Term Studies of Conservative (Reversible) Therapy
| Author | Diagnosis* | Treatment | No. of Patients | Years Since Treatment | % Success Reported |
| Greene and Laskin | Muscle | Exercise, meds, PT, appliances | 135 | 0.5-8.0 | 76.0 |
| Greene and Markovic | Joint | Exercise, meds, PT, appliances | 32 | 0.5-3.0 | 84.0 |
| Carlsson and Gale | Muscle and joint | Biofeedback | 11 | 0.4-1.3 | 73.0 |
| Carraro and Caffesse | Muscle | Appliances | 27 | 0.5-4.0 | 85.0 |
| Joint | Appliances | 20 | 0.5-4.0 | 70.0 | |
| Muscle and joint | Counsel, exercise, meds | 40 | 0.5-12.0 | 76.0 | |
| Cohen | Muscle and joint | Counsel, exercise, meds | 118 | 0.5-12.0 | 85.0 |
| Dohrmann and Laskin | Muscle | Biofeedback | 16 | 1.0 | 75.0 |
| Nel | Muscle | Meds, exercise, SG, appliances | 127 | 2.5 | 95.0 |
| Heloe and Heiberg | Muscle | Counsel, meds, appliances, SG | 108 | 1.5 | 81.0 |
| Wessberg et al | Muscle and joint | TENS, appliances | 21 | 1.0 | 86.0 |
| Green and Laskin | Muscle | Biofeedback, meds, relax, appliances | 175 | 5.0 | 90.0 |
| Magnusson and Carlsson | Muscle and joint | Counsel, exercise, appliances | 52 | 2.5 | 76.0 |
| Wedel and Carlsson | Muscle and joint | Exercise, appliances, SG | 350 | 2.5 | 75.0 |
| Strychalsky et al | Muscle and joint | Exercise, appliances | 31 | 2.0-3.0 | 72.0 |
| Okeson and Hayes | Muscle and joint | Meds, relax, appliances, SG | 110 | 4.0-5.0 | 85.5 |
| Randolph et al | Muscle and joint | Counsel, appliances, meds, TENS, PT | 110 | 2.0 | 88.0 |
| Okeson | Joint | Appliances | 40 | 2.5 | 75.0 |
| Williamson | Joint | Appliances | 160 | 0.3 | 89.4 |
| Kurita | Muscle and joint | Appliances | 232 | 0.16 | 84.0 |
| Sato | Joint | None | 22 | 1.5 | 68.2 |
*The diagnosis established for each patient population is designated “muscle” for extracapsular muscle disorders or “joint” for intracapsular disorders.
TABLE 11-2
Long-Term Studies of Nonconservative (Irreversible) Therapy
| Author | Diagnosis* | Treatment | No. of Patients | Years Since Treatment | % Success Reported |
| Zarb and Thompson | Muscle and joint | Appliance, SG, reconstruction | 56 | 2.5-3.0 | 79.0 |
| Banks and Mackenzie | Joint | Condylotomy | 174 | 1.0-20.0 | 91.0 |
| Cherry and Frew | Joint | High condylectomy | 55 | 0.4-4.0 | 70.0 |
| Brown | Joint | Meniscectomy | 214 | 0.3-15.0 | 80.0 |
| Bjornland and Larheim | Joint | Discectomy | 15 | 3.0 | 73.0 |
| Marcianini and Ziegler | Joint | TMJ surgery | 51 | 2.9 | 77.0 |
| Merjesjo and Carlsson | Muscle and joint | Counsel, appliances, SG, reconstruction | 154 | 7.0 | 80.0 |
| Upton et al | Joint | Ortho, ortho-surg | 55 | 2.0-5.0 | 78.0 |
| Benson and Keith | Joint | Plica, high condylotomy | 84 | 2.0 | 88.0 |
| Eriksson and Westesson | Joint | Discectomy | 69 | 0.5-20.0 | 74.0 |
| Silver | Joint | Meniscectomy | 224 | 1.0-20.0 | 85.0 |
| Holmlund et al | Joint | Discectomy | 21 | 1.0 | 86.0 |
| Joint | Plica, high condylectomy | 68 | 2.5 | 90.0 | |
| Moses and Poker | Joint | Arthroscopy | 237 | 0.0-9.0 | 92.0 |
| Murakami et al | Joint | Arthroscopy | 15 | 3.0-5.0 | 93.3 |
| Kirk | Joint | Arthrotomy and arthroplasty | 210 | 4.0-9.0 | 90.1 |
| Murakami | Joint | Arthroscopy | 41 | 5.0 | 70.0 |
| Gynther | Joint | Arthroscopy | 23 | 1.0 | 74.0 |
| Summer | Joint | Reconstruction | 75 | 1.0-6.0 | 84.0-92.0 |
| Sato | Joint | Arthrocentesis, HA acid | 26 | 0.5 | 71.3 |
| Nitzan | Joint | Arthrocentesis | 39 | 1.4 | 95.0 |
| Rosenberg | Joint | Arthrocentesis | 90 | 2.5 | 82.0 |
| Carvajal | Joint | Arthrocentesis | 26 | 4.0 | 88.0 |
| Hall | Joint | Condylotomy | 22 | 3.0 | 94.0 |
*The diagnosis established for each patient population is designated “muscle” for extracapsular muscle disorders or “joint” for intracapsular disorders.
In reviewing these data, one must remember that the types of patients and the criteria for diagnosis and success vary; it is therefore difficult to compare studies. A very interesting general observation, however, is that conservative and nonconservative therapies seem to report similar success rates on a long-term basis (70%-85%). Although it is likely that the patient population between these groups was quite different, both conservative and nonconservative treatments have been comparably successful on a long-term basis. It would appear, therefore, that a logical approach to patient management is to attempt conservative (reversible) therapy first and to consider nonconservative (irreversible) therapy only when the reversible treatment has failed to resolve the disorder adequately.49,50 This philosophy is the basis for managing TMDs as well as any other type of disorder.
All the treatment methods being used for TMDs can be categorized generally into one of two types: definitive treatment or supportive therapy. Definitive treatment refers to those methods that are directed toward controlling or eliminating the etiologic factors that have created the disorder. Supportive therapy refers to treatment methods that are directed toward altering symptoms but that often do not affect the etiology.
Definitive Treatment
Definitive therapy is aimed directly at eliminating or altering the etiologic factors responsible for the disorder. For example, definitive treatment for an anterior dislocation of the articular disc will reestablish the proper condyle-disc relationship. Since the treatment is directed toward the etiology, an accurate diagnosis is essential. An improper diagnosis will lead to improper treatment selection. The specific definitive treatment for each TMD is discussed in future chapters. In this chapter the common etiologic and/or contributing factors are considered.
As stated is Chapter 7, TMDs result when the normal activity of the masticatory system is interrupted by an event. The event, therefore, is the etiology. Definitive therapy would attempt to eliminate the event or its consequence. Common events may include local trauma to tissues or increased emotional stress. An event may also be anything that acutely alters sensory input to the masticatory structures (e.g., acute changes in the occlusion). As discussed in Chapter 7, this represents one mechanism whereby occlusion may lead to certain TMDs (e.g., muscle disorders).
The second influencing effect of occlusion is through orthopedic instability. As previously discussed, orthopedic instability alone does not necessarily lead to TMDs. Problems arise when orthopedic instability is combined with forces associated with loading. Therefore orthopedic instability may contribute to certain TMDs (e.g., intracapsular disorders). Occlusion, therefore, can influence TMDs in two ways. The history and examination are extremely important in understanding the role of the occlusal condition in the TMD. One should always remember that the mere presence of occlusal interferences is not indicative of etiology. Almost all individuals have occlusal interferences. The occlusion condition is certainly not the etiology of all TMDs. The occlusal condition must have been acutely changed or represent significant orthopedic instability. When the occlusion does represent an etiologic factor, occlusal treatments become definitive therapies.
Another common etiology of TMDs is increased emotional stress. When this condition is suspected, therapies used to reduce stress are considered to be definitive.
Although trauma can also cause TMDs, often trauma represents a single event, and the etiology is no longer present when the patient seeks treatment. Treatment to the tissues that have been affected by the trauma can only be supportive. On the other hand, if the trauma is the result of repeated microtrauma—for example, functional activity in the presence of a disc displacement—then definitive treatment would be any therapy that would set up a more favorable environment for loading.
As discussed in Chapter 7, any source of deep pain may also be responsible for the TMD. Deep pain input can refer pain to the face as well as cause protective muscle co-contraction. When a source of deep pain input is present, it must be eliminated so that the secondary pain and muscle response can be resolved. Elimination of this pain is considered definitive therapy.
The last etiology discussed in Chapter 7 was parafunctional activity. Whether this is diurnal or nocturnal bruxing or clenching, this type of muscle activity can be responsible for TMD symptoms. When this is present, definitive therapy is aimed at eliminating this muscle activity.
In this section, each of the five types of etiologic considerations is discussed and definitive treatments for each will be listed. It is often difficult to ascertain the most important etiologic factor causing the TMD, especially on an initial visit. Therefore it is wise to move cautiously with treatment and avoid being too aggressive at first. It is with this rationale that the statement is made: All initial treatment should be conservative, reversible, and noninvasive.
Definitive therapy considerations for occlusal factors
Occlusal therapy is any treatment that is directed toward altering the mandibular position and/or occlusal contact pattern of the teeth. It can be one of two types: reversible or irreversible.
Reversible occlusal therapy
Reversible occlusal therapy alters the patient’s occlusal condition only temporarily and is best accomplished with an occlusal appliance. This is an acrylic device worn over the teeth of one arch; its opposing surface creates and alters the mandibular position and contact pattern of the teeth (Figure 11-1).
The exact mandibular position and occlusion will depend on the etiology of the disorder. When parafunctional activity is to be treated, the appliance provides a mandibular position and occlusion that fit the criteria for optimal occlusal relationships (Chapter 5). Thus when the appliance is being worn, an occlusal contact pattern is established that is in harmony with the optimal condyle-disc-fossa relationship for the patient. The appliance therefore provides orthopedic stability. This type of appliance has been used to decrease symptoms associated with various TMDs11,51–53 as well as parafunctional activity.54–68 Of course the orthopedic stability is maintained only while the appliance is being worn; therefore this is considered to be a reversible treatment. When the appliance is removed, the preexisting condition returns. An occlusal appliance that utilizes the musculoskeletally stable (in centric relation, or CR) position of the condyles is referred to as a stabilization appliance.
Irreversible occlusal therapy
Irreversible occlusal therapy is any treatment that permanently alters the occlusal condition and/or mandibular position. Examples are selective grinding of teeth and restorative procedures that modify the occlusal condition (Figure 11-2). Other examples are orthodontic treatment and surgical procedures aimed at altering the occlusion and/or mandibular position. Appliances designed to alter growth or permanently reposition the mandible are also considered irreversible occlusal therapies. These treatments are discussed in the last section of this text.

In treating a patient, one should always be mindful of the complexity of many TMDs. Often, especially in dealing with muscle hyperactivity, it is impossible to be certain of the major etiologic factor. Therefore reversible therapy is always indicated as the initial treatment for patients with TMDs. The success or failure of such treatment may be helpful in determining the need for later irreversible occlusal therapy. When a patient responds successfully to reversible occlusal therapy (such as a stabilization appliance), there may be indications that irreversible occlusal therapy might also be helpful. This correlation is sometimes but certainly not always true. Occlusal appliances can affect masticatory function in a variety of ways. These are discussed in Chapter 15.
Definitive therapeutic considerations for emotional stress
Some TMDs are etiologically related to certain emotional states.69–72 Emotional stress is certainly one of several psychological factors that must be considered. Increased levels of emotional stress can affect muscle function by increasing the resting activity73–74 (protective co-contraction), increasing bruxism, or both. Increased levels of emotional stress also activate the sympathetic nervous system, which may in itself be a source of muscle pain.75,76 Activation of the autonomic nervous system may also be associated with other psychophysiologic disorders commonly associated with TMD, such as irritable bowel syndrome, premenstrual syndrome, and interstitial cystitis.77,78 It is extremely important that the clinician recognize this relationship and alter treatments appropriately. Unfortunately, the dental practitioner is not often trained well in this area of medicine and therefore can easily feel inept or uncertain. Nevertheless, dentists who treat TMDs must have an appreciation for these problems so that, if indicated, proper referrals can be made.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



