12 Skin Resurfacing
Patient Selection
As with any cosmetic procedure, proper patient selection is the key to obtaining ideal results. Lighter skin types have the potential for more predictable skin resurfacing and fewer problems with hyper- and hypopigmentation. Although many skin classification systems exist, the Fitzpatrick system (Table 12-1) is the most widely used. This system is derived from skin response to sunlight.
| Skin Type | Skin Color and Characteristics |
|---|---|
| 1. Ivory white | Always burns, never tans |
| 2. White | Usually burns, tans minimally |
| 3. White | Burns moderately, tans moderately |
| 4. Beige/light brown | Burns minimally, tans easily |
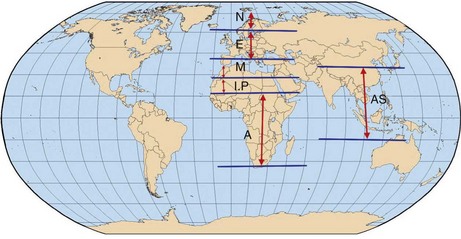
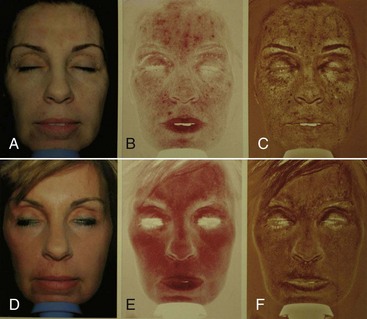
Whereas the Fitzpatrick system is relatively straightforward, looking at the larger picture of who we are and where we came from intensifies our understanding of skin types. The Fanous classification of skin type is based on racial origins (Figure 12-1) and puts a logical understanding behind numbers.
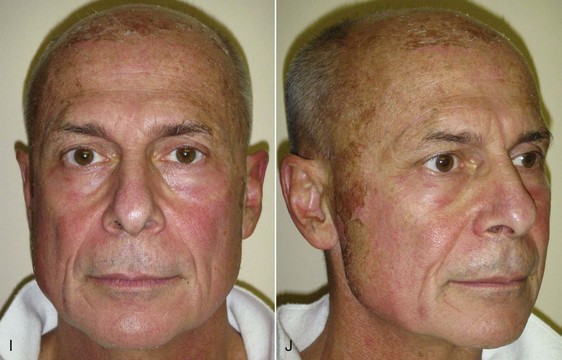
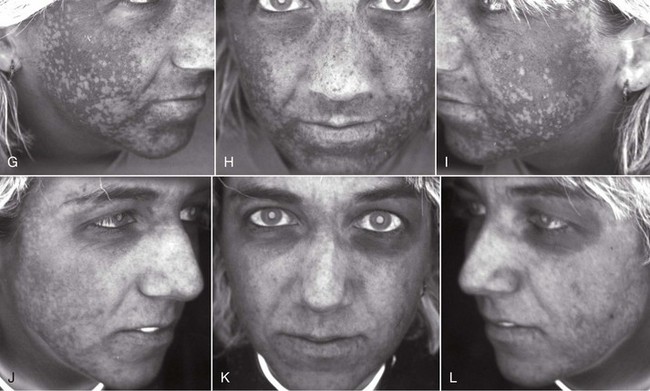
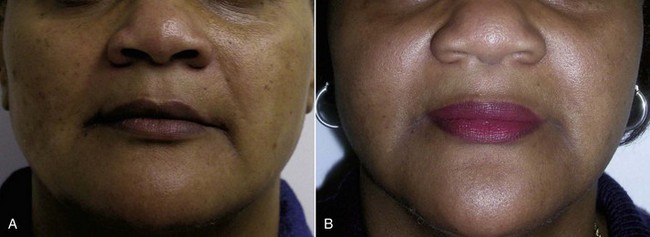
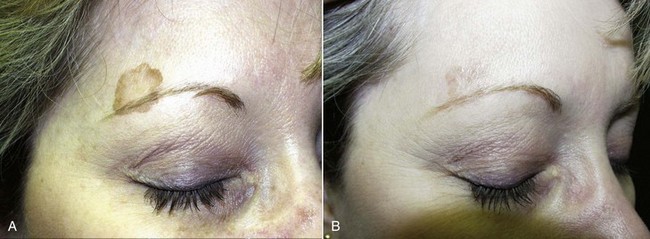
In treating various skin types, novice surgeons should keep in mind that the darker a patient’s skin is, the more potential problems can exist with peel or laser, especially hyper- or hypopigmentation (Figure 12-2). The very light skin types and the darkest skin types are the most stable; the mixed browns are the most problematic. Referred to as global skin, this type should always be approached with caution when using peels and lasers. The best patients for the novice resurfacing surgeon are Fitzpatrick 1 and 2 skin types. Type 3 and above should be reserved for more experienced surgeons.
Resurfacing Contraindications
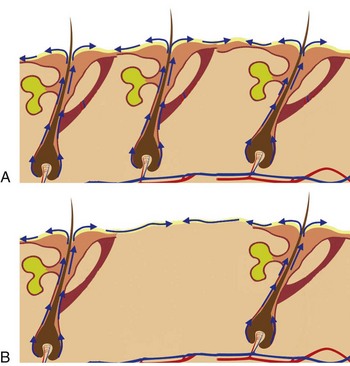
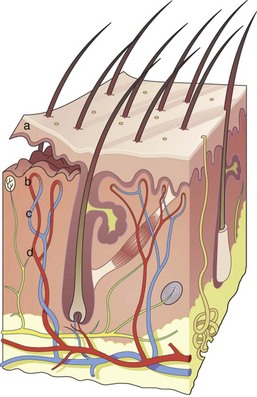
After the epithelium is destroyed by chemical agents or light sources, it must regenerate, or a full-thickness burn scar can result. Reepithelialization occurs from the base of the pilosebaceous units, and the presence of the hair/sebaceous gland unit is directly related to how much and how quickly the new epithelium regenerates. In a process known as epiboly, the pilosebaceous units serve as the progenitors of new epithelium. New epidermal cells migrate from the base of the pilosebaceous unit, progress up the hair shaft, then spread laterally on the injured skin surface (Figure 12-3). It stands to reason that areas of the body that are heavily populated with pilosebaceous units have a better chance of more rapid epithelialization. The face has 30 times the pilosebaceous units as the neck or chest and 40 times the number on the dorsal arms and hands. For this reason, deeper peeling and laser treatment can be performed on the face, whereas the same treatment on the neck or extremities can lead to disastrous scarring (Figure 12-4). In low hair-bearing areas, the epithelial cells simply have too far to go, but areas heavily populated with hair follicles heal faster.
Knowing the importance of pilosebaceous units and healing, any procedure or medication that reduces or suppresses the pilosebaceous units could affect the result and cause scarring. Systemic retinoids such as isotretinoin (Accutane) work by suppressing the pilosebaceous units, which would obviously affect reepithelialization after skin resurfacing by peel or laser. Most authorities recommend waiting at least 1 year after Accutane therapy before resurfacing. Obagi1 has shown that a 6-month waiting period after Accutane therapy before chemical peel is safe. Radiation therapy can also destroy pilosebaceous units, and patients who have received therapeutic radiation can be problematic healers.
Preresurfacing Skin Conditioning
Chemical peeling is not a procedure that someone just shows up and does. It has been shown that prepeel skin conditioning speeds healing, reduces postpeel pigmentation problems, and improves treatment results.2 A solid prepeel skin conditioning program also makes the patient take ownership of their care and outcome. A motivated patient will be very compliant with prepeel conditioning, and poorly motivated patients will be weeded out. Patients who cannot tolerate the chapping, peeling, and redness from Retin-A will not likely do well with a chemical peel. Most important, however, is that prepeel conditioning or “priming” will improve their experience and outcome. In reality, all the patients in a cosmetic practice should be on “eternal skin care” as it will make them younger, there is science behind that.
Aging skin has decreased collagen in the dermis, increased keratinocyte atypia, roughness, and dyspigmentation. The goal of prepeel priming is to restore the skin to as normal as possible before wounding it.3 Epidermal actions of Retin-A (tretinoin) 0.05% to 0.1% reverse many of these aging changes by normalizing keratinization, creating a thin and compact stratum corneum, and improving epidermal dyspigmentation.3 In the dermis, Retin-A will also increase collagen production (fibroblasts), increase glycosaminoglycans, and reduce solar elastosis. Retin-A has better results when used at a higher percentage on a nightly basis but is not a user-friendly drug. The inflammatory stage of redness, burning, and chapping begins quickly and peaks at 2 to 3 weeks, then slowly subsides. Patients typically will begin a regimen then quit when the inflammation begins. They must understand that this is not only normal and expected, it means positive things are occurring. When patients complain of Retin-A dermatitis, I congratulate them and tell them it is working. Many patients will start and stop and never get through the inflammatory stage. It only works if you use it. The epidermal and dermal changes from Retin-A allow the chemical peel agent to penetrate deeper and more homogenously.
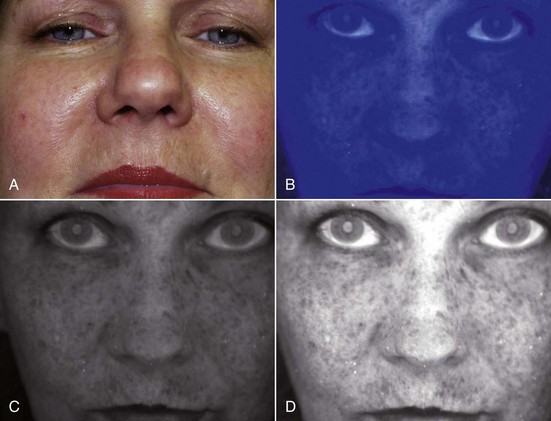
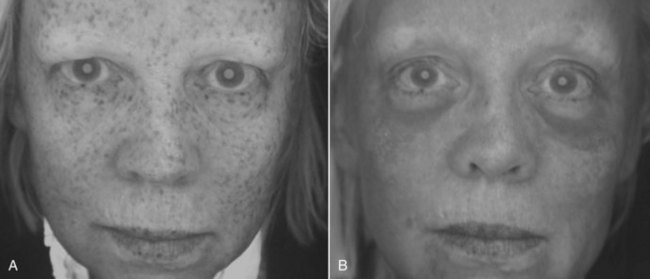
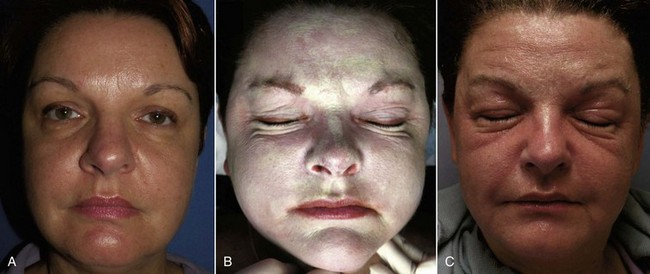
In my experience, a medium-depth chemical peel will improve fine lines, wrinkles, and minor scars, tighten the skin, smooth the skin texture, and improve epidermal and superficial dermal dyschromias. The degree of skin tightening is minor to moderate and does not rival that of deep peels (complicated and more unpredictable procedures) or aggressive laser skin resurfacing. Patients who expect facelift or laser-quality skin tightening or wrinkle and scar reduction will be disappointed with a medium-depth chemical peel. Having said this, peels can be repeated in 90 days, and the cumulative improvement can be significant. All patients are good medium-depth TCA peel candidates. The rapid wounding and turnover of skin reduces the buildup of aged skin and pigment, but the depth of the pigment and the peel are directly related to the outcome. Superficial epidermal pigment is likely to significantly improve with medium-depth TCA peels, whereas deeper dermal pigment is more resistant or sometimes impossible to eradicate. A simple and very effective means of determining the estimated depth of pigment is the use of ultraviolet light.4 Whether using a common Wood’s lamp, ultraviolet lamps available at party stores, or a dedicated skin scanner, the surgeon and patient can visualize the degree and depth of facial skin pigmentation. Ultraviolet light enhances epidermal melanin. If a patient has visible dyschromias (lentigines), commonly called age spots, sun spots, or liver spots, and these enhance under ultraviolet light, they are usually in the epidermis and will respond well to medium-depth or even superficial-depth chemical peels. If there are visible spots that do not enhance under ultraviolet light, they reside in the deeper dermis and are less likely to improve with a single medium-depth peel.
Commercially available ultraviolet skin scanners are available from most dermatologic suppliers. These devices have multiple ultraviolet bulbs and a mirror for the patient to view the pigmentation (Figure 12-5). The other end of the device has a viewing port for the observer (Figure 12-6). I have described a means of using a common digital camera and imaging software to reproduce the ultraviolet view for printout and viewing by the patient4 (Figure 12-7). This not only serves as motivation for the patient to begin skin care or have a peel, it also gives the surgeon an idea about the depth of the pigment and the response of the proposed peel. By making pretreatment and postpeel images, the surgeon and patient can evaluate the efficacy of the procedure. Images might also be used (with permission) for procedure marketing (Figure 12-8).
Newer technology has simplified this process. The Reveal Imager system (Canfield Imaging Systems, Scientific, Fairfield, NJ) is a convenient and portable system that gives an immediate computer image of the patient in normal light and has filters that enhance vascular and pigment abnormalities (Figure 12-9). These devices are well worth the investment. Patients are always surprised at the amount of skin damage they have and are motivated to begin skin care and have a skin peel procedure. Images can also be used to show the effect of the procedure (Figure 12-10).
Medium-Depth Chemical Peel Procedure
To clarify and quantify types of peels, a consideration of tissue damage and healing time is the most accurate means of classification. A very superficial chemical peel wounds all or part of the stratum corneum and heals in 2 to 3 days. A superficial peel wounds all or part of the epidermis to a depth of approximately 0.06 mm and heals in 4 to 6 days; Retin-A is an example of this type of peel. A medium-depth chemical peel destroys all or part of the papillary dermis to an approximate depth of 0.45 mm and heals in 7 to 8 days; TCA and glycolic acid are examples of medium-depth peel agents. Deep peels destroy the epidermis, the papillary dermis, and extend into the reticular dermis to an approximate depth of 0.6 mm; 10 to 12 days are required for reepithelialization. Phenol or high concentrations of TCA are examples of deep peel agents. Boxes 12-1 and 12-2 summarize chemical peels.
Box 12-1 Summary of Peeling-Depth Classifications
Box 12-2 Healing Time of Various Peels
(Image from Waugh A, Grant A: Ross and Wilson Anatomy and physiology in health and illness, ed 10, Edinburgh, 2006, Churchill Livingstone.)
Figure 12-11 shows two patients 7 days after aggressive laser and medium-depth chemical peel, illustrating the differences in wounding and healing.
Peeling Agents
Numerous chemical agents exist for performing chemical face peels and are used by themselves or in combination with other agents. Simple creams such as Retin-A or fluorouracil (5-FU) can be used for at-home superficial peels and can be started and stopped as necessary by the patient. The more traditional “procedural” peels are most often performed with liquid acid solutions (Box 12-3) and are applied at various concentrations with or without supplemental anesthesia. Some peeling agents such as alpha hydroxy acid (AHA) can be halted during the procedure with a neutralizing agent, but other agents such as TCA or phenol cannot be slowed down, stopped, or reversed. Once they are applied, the damage is done.
Mechanism of Action
Peeling agents are commonly classified by their mechanism of action on tissue. Keratolytic agents include glycolic acid, lactic acid, citric acid, malic acid, tartaric acid, and salicylic acid.4 These lighter-peel agents interrupt the adhesion of keratinocytes and are used for exfoliation but do not have a significant effect on deeper wrinkles or scars. They are mainly used for improvement of skin roughness, very fine lines, acne control, and mild pigmentation disorders. They are typically performed without anesthesia and are repeated numerous times to obtain a result.
Chemical Peel Procedure
A chemical peel performed at a beauty shop or spa is quite different from one performed by a cosmetic surgeon using a more concentrated acid and IV sedation. Many variables can affect the depth and related result of a chemical peel.5 These include:
Ultralight Tca Peel
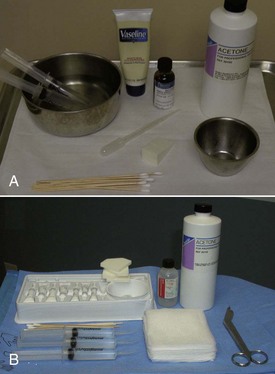
For the novice peeler, performing simple single-coat, low-concentration (e.g., 15%) peels on awake patients is a good beginning. To make a 15% concentration of TCA, use 2 mL of 30% TCA diluted with 2 mL of water, and apply a single coat after acetone or alcohol degreasing (Figure 12-12). The entire face can be treated, but some surgeons do not treat eyelids with these conservative peels. The patient will have a tolerable burning sensation and probably not manifest any significant skin frosting. Over the next week, there may be very slight flaking. A peel of this nature can be repeated every 2 weeks for cumulative improvement.
Once comfortable performing ultralight peel, the surgeon can treat the next patient with two coats of the same concentration, still easily tolerated by the average person. A handheld fan can ease the burning sensation (Figure 12-13). The skin may very slightly frost in some areas, and the skin will flake or possibly peel to a small extent over the next 3 to 4 days.
Multiple-Coat, Medium-Depth TCA Peels
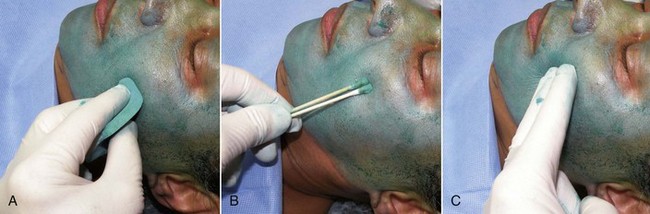
The face is degreased with acetone or alcohol by rubbing vigorously with gauze pads (Figure 12-14). Adequately degreased skin will appear dry and without shine. The inferior border of the mandible is marked with a surgical marker unless the neck or décolletage is to be treated. Any specific scars or areas of deeper pigmentation are also marked. Instrumentation is minimal for chemical peel and is shown in Figure 12-15.
At this point, the patient is sedated and the procedure begun. The head is elevated slightly so that any dripping will not flow toward the eyes. A small amount (2 to 4 mL) of 30% TCA is placed in a small basin then applied evenly to the entire face with a sponge applicator, cotton-tipped applicators, or gloved fingers. A folded gauze pad is also effective because the acid can be rubbed into the skin. It is of utmost importance to protect the patient from spilled or misapplied acid. The basin is never passed over the patient’s face but rather is held by the assistant to the patient’s side (Figure 12-16).
Generally the 2 to 4 mL of 30% TCA will cover the entire face for a single coat. I generally also treat the earlobes and upper and lower eyelids. The first coat of TCA is applied evenly to the entire face in a systematic fashion (Figure 12-17, A). To treat the entire face equally and not inadvertently “double treat” regions, it makes sense to use the same application pattern in all cases, beginning with one area and moving to another, working around the entire face or area to be treated. Some surgeons use a clock-face pattern and begin in the right forehead, progress to the right temple and cheek, then to the right lower cheek, then cross the midline and proceed up the left side of the face.
The second (and possibly final coat) of TCA is applied after several minutes. Again, several minutes are allowed to elapse to evaluate signs of peel depth (see Figure 12-17, B). Skin frosting is indicative of epidermal and dermal skin protein coagulation and begins almost immediately. Areas of thinner skin will frost upon contact, whereas the more sebaceous and thicker skin will require several coats to frost. When applying the acid to areas of wrinkled skin such as the lower lids, corners of the mouth, or lateral canthal regions, the skin is stretched to allow the acid to penetrate the wrinkles. Using the sharp end of a broken cotton-tipped applicator stick or tongue blade to “grind” the acid into acne scars is effective6 (Figure 12-18).
The goal of a medium-depth 30% TCA peel is to produce a homogenous frost commensurate with the desired depth of penetration (Box 12-4; Figure 12-19). A sparse, irregular patchy frost signifies epidermal penetration, and the nature of the frost changes as the acid progresses deeper. As the acid progresses to the papillary dermis, a light white frost with a pink background is seen; blood vessels of the papillary dermis are still patent. Progression of the acid deeper into the papillary dermis but not into the reticular dermis results in vasospasm in the capillary loops of the papillary dermis. This reaction causes blood flow in this area to cease and the pink background to disappear. The frost appears as a solid white sheet. A peel that reaches this level implies that the whole papillary dermis is involved, and the upper reticular dermis has been reached but not penetrated, which is the endpoint of a medium-depth chemical peel.3 This is also referred to as the intermediate reticular dermis (IRD) by some authors.3 Lighter peels end at the IRD, and deeper peels extend below the IRD. A grey frost can indicate overtreatment and impending burn. Judging the endpoint and related frosting requires significant experience, so the novice peeler should work their way from light to medium to deeper peels. This should be done over a significant period of time, with close observation of each patient during and after the peel. Photographic documentation of successive cases serves as an excellent learning aid.
Although the presence and absence of pink skin is helpful in endpoint judgment, it is more difficult to visualize in darker skin types. Another means of evaluating when the papillary dermis has been reached is epidermal sliding (Figure 12-20). This is exaggerated wrinkling of the skin when pinched. Prior to complete precipitation and coagulation of papillary dermal proteins, papillary dermal edema and disruption of anchoring fibrils allows the epidermis to move more freely, resulting in exaggerated wrinkling when the skin is pushed or pinched.1 Put simply, when epidermal sliding begins, the acid is entering the papillary dermis. When it disappears, the acid is in the papillary dermis. This transient sign disappears as the peel progresses and may not be apparent in thicker-skinned individuals.3
The acid is rubbed into the hairline so no visible demarcation line exists (Figure 12-21). TCA will not harm the hair. The eyelids are treated last. One or two coats of 30% TCA can be very effective in treating lower-lid dermatochalasis (Figure 12-22). This is very thin skin and frosts quickly (Figure 12-23), so to prevent overtreatment, adequate time should elapse before the second pass. Novice peelers should be very conservative in this area. A cotton-tipped applicator provides precision application near the eye. A water source should be readily available in the case of acid entering the eye. The upper eyelid can also be treated but does not require aggressive treatment. TCA is NOT toxic to the cornea, but if it enters the eye and is flushed immediately, healing is usually uneventful, although the patient will feel irritation for several days. Significant eye contact would warrant an ophthalmology consult.

FIGURE 12-21 To lessen demarcation lines and transition zones, the acid is rubbed well into the hairline.
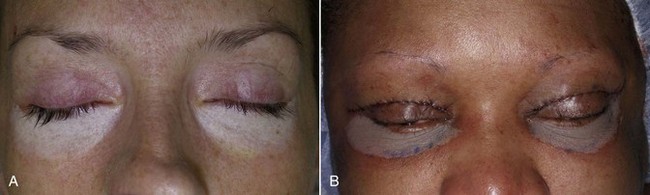
FIGURE 12-23 Frosting of the lower eyelids after application of two coats of 30% trichloroacetic acid (TCA).
If the neck or décolletage is to be treated, the entire process must be reconsidered in light of the decreased number of pilosebaceous units in the nonbearded neck. Severe scarring and disfigurement can and has occurred with chemical peels and lasers. I never use 30% TCA on the neck, but I will use up to three coats of 15% or two coats of 20% (Figure 12-24). To concoct 15% TCA, 2 mL of 30% of TCA are mixed with 2 mL of water. To make a 20% mixture, 4 mL of 30% TCA are mixed with 2 mL of water. The novice peeler should treat the neck to half the level they think necessary. It is important to keep in mind that multiple peels can be performed at 90-day intervals, and it is better to treat safely over several peels than create scarring from an overly aggressive peel.
I do not treat to a solid white frost on the neck, but rather a much lighter frost with a pink background (Figure 12-25). Patients must understand that they will have much less result on their neck than their face with both peel and laser. The décolletage (upper chest) can also be treated with the same conservative tenets as the neck. Patients often want lower and lower treatment, but they must realize there will always be a demarcation line, so the face and neck are generally my desired treatment regions.
Postpeel Care
Immediately after the peel, the entire treated area is covered with petroleum jelly or Aquaphor (Belersdorf Inc., Wilton, CT), and if the patient is uncomfortable, cold compresses are placed on the treated areas (Figure 12-26). Transient burning is common but quickly dissipates. Immediate swelling may be evident (Figure 12-27). Wound care throughout the healing process is very simple. Patients wash the treated area with a hypoallergenic cleanser and keep petroleum jelly or Aquaphor on the areas continually for 1 week. Most patients do not need analgesics. In the rare event of severe swelling, oral steroids can be used. Antibiotics and antivirals are continued through the fifth to seventh day or until epithelialization is complete. Some surgeons no longer advocate antibiotics with chemical peeling,6 but the standard of care in the local community should dictate this.
Patients should understand that for the first 48 hours, not much change will be apparent other than skin tightness. As described earlier, over the next several days, the skin will become thickened and brown and begin to peel first in areas of increased movement (perioral and periorbital regions) between day 3 and 5. It is human nature to want to pick at the peeling skin, but this can leave scarring, so patients should be encouraged to let the skin peel naturally. Some patients will actually have sheets of skin peel off; others will notice the dead skin emulsify and exfoliate when washing the face. For medium-depth peels, most of the peeling is complete by day 7, and most female patients are back in makeup by day 7 to 8 (Figure 12-28). Figure 12-29 shows the author before and throughout the week after medium-depth TCA peel. Sequelae and complications will be discussed later in this chapter.
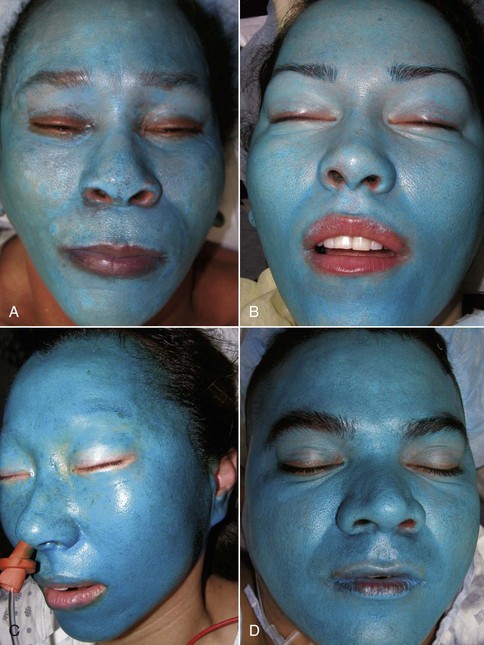
Obagi Blue Peel
Over the years, numerous proprietary chemical peels have come and gone, but the Obagi Blue Peel (OBP) has maintained a niche for reliable and safe chemical peeling. Although some doctors feel there is no advantage to using the OBP over conventional TCA, I almost always use it when peeling pigmented (global) skin (Figure 12-30). I have done over 100 of these peels on Fitzpatrick 4 to 6 skin types, and they proved safe and effective. My experience is purely anecdotal, but sometimes in clinical practice, whatever works, works! I can also verify after teaching hundreds of doctors chemical peeling techniques that the OBP is a great way to learn the art and a safe and effective means of treating darker skin types. I believe the ingredients of the OBP make the peel process slower so the novice surgeon can better observe the impending depth signs, making the process safer.
Although one could use the OBP on any skin type, I choose to treat Fitzpatrick 1 to 3 skin types with pure 30% TCA and treat the darker skin types with one to three coats of 20% TCA in the OBP. The contents of the OBP include glycerin, saponins, and a nonionic blue color base. A reduction of the surface tension of the TCA, water, and glycerin occurs, which results in a homogenous TCA-oil-water solution that slows the penetration and release of TCA in the skin. This results in a more even coating, allows the skin proteins to neutralize the penetrating acid between applications, and produces slower frost formation as compared to straight TCA peels. This gives the surgeon extra time to evaluate the evolving depth (frost) signs and stop at the desired depth for a wider margin of safety.3 Finally, the color prevents inadvertent double treatment on an area (common with clear TCA), because the blue dye shows what areas have been covered.
The OBP procedure is much the same as the previously described TCA peels. The same patient selection criteria and skin conditioning regimens are used. The face is degreased with acetone or alcohol and the blue peel component mixed with the TCA (Figure 12-31). The OBP component is contained in 2-mL tubes. If one tube is mixed with 2 mL of 30% TCA, a 15% solution of TCA will result. For a more aggressive peel, 1 tube of blue base (2 mL) is mixed with 4 mL of 30% TCA (final concentration 20%). The 15% TCA/blue base is used for novice peelers and superficial treatment. A single coat of 15% TCA will exfoliate the stratum corneum. Three to four coats of 15% TCA (on normal skin) will peel to the level of the papillary dermis. The 15% mixture is also better tolerated on awake patients. The 20% mixture is more aggressive and should not be used by inexperienced peelers. In normal skin, a single coat of 20% will penetrate the stratum corneum but above the basal layer. A second coat of 20% will reach the papillary dermis. Patients with thicker skin may take more coats of either concentration, and those with thin skin may take less. Experience has a lot to do with the judgment of peel depth and healing. Again, begin with conservative peels and progress to more advanced techniques over time. In chemical peeling, the art is as important as the science.
Once the TCA and blue base is mixed, the entire contents are applied to the face using the preferred method of application (Figure 12-32). Dilutions are designed to require the entire mixture to treat the face or similar 5% of body surface area. The first coat is applied evenly around the entire face with care not to overlap passes. I prefer to leave the eyelids last to concentrate on safety without distraction. After the entire 4 or 6 mL (depending upon the concentration) is applied, at least 2 minutes are allowed to elapse before applying the next coat. For medium-depth chemical peels, most patients can tolerate three to four coats of 15% or two to three coats of 20%. In both instances, the skin will generally heal in 7 to 8 days.
Light frosting will be noticeable with the first coat of blue peel but will be sparse and patchy. The second coat will accelerate the frosting (and the discomfort). After the second coat, at least 2 minutes must again be allowed to elapse before the next coat. White frost with a pink background will generally appear after the third or fourth coat of 15% or the second or third coat of 20%. This indicates the papillary dermal level, which is adequate for noticeable results in most patients (Figure 12-33). The experienced peeler can proceed with additional application to a dense white frost without pink background, indicating the IRD has been reached. When in doubt, use less!
At the end of the peel, the frost will generally persist 10 to 15 minutes then dissipate. Patients must understand that their skin will have a bluish tint for several days. Much of the blue base can be removed with the included cleanser that accompanies the OBP kit (Figure 12-34).

FIGURE 12-34 A significant amount of the blue base can be removed by washing with the included cleanser.
Postpeel care is the same for the previously described straight TCA peel. Patients apply a light coat of petroleum jelly or Aquaphor until the peeling is complete and wash the face twice a day with a hypoallergenic wash. Most patients will begin to peel by day 3 or 4 and finish by day 6 or 7 (Figure 12-35).
Chemical peeling can also be used as an adjunct to laser skin resurfacing, especially to blend in hairlines and treat the neck. Figure 12-36 shows combination cases.
Case Presentations
Figures 12-37 to 12-45 show before-and-after chemical peel patients treated by the author.

FIGURE 12-43 African American female shown before (A) and after (B) an Obagi Blue Peel for perioral and generalized pigmentation.
Chemical Peel Complications
As I have said many times, successful chemical peeling is as much art as science and requires significant experience to obtain predictable results. Precise attention to creating a homogenous frost and hence peel depth is critical to the end result (Figure 12-46). It is equally important to make sure that all regions are symmetrically treated and blended into the hairline, or the transition is noticeable (Figure 12-47).
Overcoverage or extending natural transition zones is just as problematic as undercoverage. Not all chemical face peel patients undergo simultaneous neck peeling. If the neck is not peeled, the transition must stop at the mandibular border so as not to be noticeable (Figure 12-48). Landmarks can shift with a supine patient, so the mandibular border should be marked in the upright position before the case (Figure 12-49).
This chapter has mentioned the sensitivity of the neck skin compared to facial skin. Delayed healing and severe scarring can occur with overtreatment (Figure 12-50). It is very tempting to aggressively treat the neck because it is a major area of concern for many patients. Although some practitioners espouse predictable expertise with aggressive neck peeling, I would again caution all peelers to reject the temptation of instant neck rejuvenation, owing to inherent risks. As far as cosmetic surgery has advanced, when it comes to facelift, lasers and peels, the neck stands out against a rejuvenated face and a predictable and safe treatment option will someday be a welcomed advance in the art.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses