12
Paediatric dentistry
- Dental development and dental anomalies
- Dental caries – pathogenesis and prevention
- Tooth wear
- Treatment of caries in the primary dentition
- Soft tissue problems in children
- Anxiety and pain control
- Trauma in children
Introduction
Paediatric dentistry involves the oral and dental care of children from birth onwards and is concerned with all aspects of oral and dental development and problems that may arise. This chapter includes some of the important features and considerations that are presented to the clinician together with treatment modalities. It is, in effect, a multidisciplinary subject with the common theme being the care of children. Therefore it is not surprising that many aspects which are applicable to paediatric dentistry also appear elsewhere in this textbook (e.g. preventive dentistry, tooth notation, materials, etc.).
Dental development
The earliest evidence of dental development in the fetus occurs as early as 7 weeks in utero when there is a proliferation of the oral epithelium to form the dental lamina, which then goes on to form the enamel organs. The latter are ten discrete cellular condensations in the lower jaw and ten in the upper jaw and these are the beginnings of the tooth germs, which are destined to become the primary (deciduous, baby) teeth. At a much later stage there is an outbudding from each primary tooth germ and these form the tooth germs of the permanent teeth which will replace the primary predecessors. At the distal part of each, the dental lamina continues to grow backward and produces tooth germs for the permanent first, second, and third molar teeth.
Tooth notation
Tooth notation systems have been developed in order to provide a quick, accurate and standardised way of referring to particular teeth. Of over 32 different systems that exist, the two most commonly used in the UK are described below.
The Zsigmondy–Palmer system
This system, sometimes called the Palmer system, was first developed by Zsigmondy, an Austrian dentist, as early as 1861. The mouth is divided into four quadrants and each primary tooth is assigned a letter of the alphabet from A to E, starting at the midline with the central incisors (the permanent teeth are assigned the numbers 1 to 8). The letters are placed inside an L-shaped symbol used to identify the quadrant. Because of the problems of recording this information electronically and in printed text, a modification of this notation can be used which replaces the L quadrant indicator with the letters UL, UR, LR and LL, e.g. URE for upper right second primary molar, LLA lower left central incisor, etc.
The FDI notation
This was adopted by the Federation Dentaire Internationale (FDI) in 1971 and is used more internationally than the Zsigmondy–Palmer system. It is a two-digit code and again the mouth is divided into quadrants. The first of the two digits indicates the quadrant and the second the tooth position. The quadrants are numbered 1 to 4 in the permanent dentition and 5 to 8 in the primary dentition, such that the upper right quadrant is 1 or 5, upper left is 2 or 6, lower left is 3 or 7 and lower right is 4 or 8, depending on the dentition. For example, the lower left primary first molar is 74; however, it is not spoken as ‘seventy-four’, but rather ‘seven four’. All the primary teeth in the mouth would therefore be:
55 54 53 52 51 61 62 63 64 65
85 84 83 82 81 71 72 73 74 75
Tooth eruption
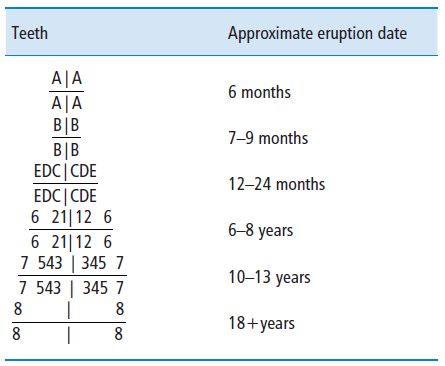
The first tooth to erupt is the primary mandibular central incisor at 6 months of age (Table 12.1). This is soon followed by the maxillary central incisors and then all the lateral incisors. Thus all the incisors have erupted by about 9 months of age. There is then a quiescent period of 3–5 months until the next eruption phase when the primary first molars emerge at about 12–14 months of age. The second quiescent period of 3–5 months occurs after which is seen the eruption of the primary canines at 16–18 months. The third and longer rest period of 5–10 months then follows after which the last teeth, the second molars, complete the primary dentition at 24–30 months of age. There is then a long interval of about 4 years before the permanent molars start to appear at 6–8 years of age when the first permanent molars erupt together with the incisors. The next quiescent period of 2–3 years precedes the next phase of eruption of the premolars, second molars and canines at 10–13 years. The last teeth to erupt, if present, are the third molar or ‘wisdom’ teeth and this occurs at any time from about 18 years onwards.
Table 12.1 Approximate eruption dates.
The timing of eruption will vary greatly and it may not be unusual for teeth to erupt soon after birth or as late as 12 months and still be considered within the limits of normality. The important feature is the sequence of eruption of teeth. For instance, the normal eruption sequence of the maxillary permanent anterior teeth is central incisors first followed by the laterals. If, however, the lateral incisor appears before the central, then almost certainly it is an untoward situation and may indicate some pathology, such as a supernumerary tooth, retained primary tooth, damaged permanent central incisor, trauma, etc.
Morphological differences between primary and permanent teeth
There are numerous differences between the primary and permanent dentition, many of which give rise to considerations in relation to operative treatment, as discussed later in this chapter. Essentially, primary teeth have:
- A shorter crown.
- A lighter colour.
- Narrower occlusal surfaces.
- Broader and flatter interproximal contact areas.
- Thinner enamel and dentine.
- Longer pulp horns, particularly the mesial buccal.
- Relatively larger pulps.
- Enamel prisms which run slightly occlusally at the cervical margin.
- Curved roots (to accommodate the developing permanent successor).
- Roots which have open apices.
- More tortuous and irregular pulp canals.
- An abundance of accessory pulp canals at the furcation areas.
Disruption in the number of teeth
Hypodontia
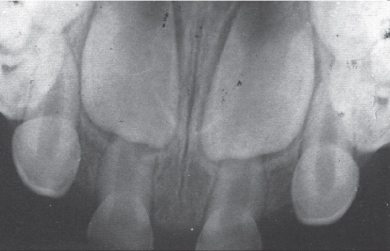
If there is a failure of the dental lamina to form tooth germs, then the number of teeth that develop will be affected. A reduction in the number of teeth is known as hypodontia. In extreme cases, where no tooth germs at all develop, there will be a complete absence of primary and secondary teeth, a condition known as total hypodontia or anodontia. In these rare cases it is invariably an inherited disorder and is always associated with other problems which fall under the generic name of ectodermal dysplasia. Patients so affected, as well as having no or at least substantially fewer teeth than normal, may have a decrease in sweat glands and hair follicles, defects in finger nails, etc. Absence of a smaller number of teeth is relatively common and in the permanent dentition the third molar teeth are commonly absent. Less frequent is the congenital absence of maxillary lateral incisors (Figure 12.1) and second premolars.
Figure 12.1 Occlusal radiograph of a three year old child showing bilateral congenital absence of the primary and permanent lateral incisors.
The presence of teeth affords proper development and growth of the mandible and maxilla and, therefore, in cases of total hypodontia or anodontia, management is difficult owing to smaller jaws and a lack of alveolar bone growth, making the provision of dentures and subsequent use of intraosseous implants problematical. The management of one or two congenitally absent teeth is usually much easier. Often a primary tooth that has no permanent successor will remain in place as a functional tooth for many decades. Where the primary tooth with no permanent successor is lost then the resultant space may close either naturally with the adjacent teeth moving into the space or with orthodontic appliance therapy. Should this not be the case and the space needs to be managed, then a partial denture, bridge or, subsequently, an intraosseous implant will be required.
Hyperdontia
Should extra tooth germs of either the primary or secondary dentition occur, then extra teeth will appear, a condition known as hyperdontia. This may have arisen as a result of extra proliferations of the dental lamina or one of the normal tooth germs, at an early stage, actually splitting to form two tooth germs. These extra teeth are also called supernumerary teeth and can occur in any part of the mouth and may be related to a particular tooth group. Hence they can be incisoform, caniniform and molariform. However, they tend to be rare in the primary dentition but common in the permanent dentition. They are ten times more frequent in the maxilla than in the mandible and tend to be in the anterior region. Their form can vary from a normal-looking tooth to conical or tuberculated shaped teeth. The former is often the result of a permanent tooth germ splitting at an early stage and causing two identical teeth to form. Where the extra tooth is identical to the tooth of the normal series, then it is termed a supplemental tooth.
Occasionally an extra tooth causes no problems and is accommodated into the dental arch without disruption to the occlusion. More often than not it leads to localised crowding and this is remedied by the extraction of the tooth that is in the least favourable position.
Supernumerary teeth may cause no problems and may erupt in ectopic sites such as the palate and may be simply extracted. At other times supernumerary teeth may impede the eruption of permanent teeth or cause them to be deflected from their normal path of eruption. If this occurs, then a surgical extraction of the supernumerary tooth is required. Once a clear path of eruption has been established, the unerupted permanent tooth is likely to erupt uneventfully. Where it may be deemed that this tooth has impaired eruptive potential, then often the unerupted tooth is surgically uncovered and an orthodontic bracket and gold chain is attached. The tooth is recovered and the mucosa is sutured back in place. Subsequent gentle pressure via an orthodontic appliance will pull the errant tooth into a normal position. Occasionally, supernumerary teeth that have not led to problems may be left in order to avoid a surgical extraction. Where this occurs, as with any unerupted tooth left in situ, it will need to be monitored by having a radiograph taken at least every 2 years to ensure no pathological changes have occurred, such as resorption of adjacent teeth or cyst formation of the dental follicle.
Disruption of tooth form
The shape and size of a tooth are usually under genetic control and development of elements within the enamel organ is responsible for the resultant tooth form. In the enamel organ there are two layers of cells. The first layer is the ameloblast layer and this induces the second layer of cells, the odontoblasts, to form. The former cells are responsible for the formation of enamel whilst the odontoblasts lay down dentine. As these hard tissues form, the two layers of cells recede as the enamel and dentine layers become thicker. It is a continuous process and it has been shown that enamel is deposited at the rate of 4 μm per day. It therefore can be considered that the original position of the layer of ameloblasts and odontoblasts maps out what is the future junction between the enamel and dentine and once hard tissue is deposited this then establishes the future shape of the tooth. Therefore, it follows that if there is some sort of disturbance in this layer of cells prior to enamel and dentine formation, then the tooth form will change. Conversely, once the hard tissue is formed then the tooth form is ‘fixed’ and no changes can occur.
Figure 12.2 Geminated mandibular permanent left lateral incisors.
Double teeth
These can occur in both the primary and secondary dentitions and usually affect the anterior teeth. It may have arisen by two adjacent tooth germs that are in close proximity coalescing and forming a single but expanded tooth and this is termed fusion. When this occurs, since there are two tooth germs involved, there is one large tooth in place of two teeth, unless fusion has taken place between a tooth of the normal series and a supernumerary tooth. The other way in which double teeth arise is where there has been an expansion of a normal tooth germ before enamel and dentine has been formed. Presumably, if this was allowed to continue, the end result would be the formation of two tooth germs and subsequently two teeth as described above. However, before separation takes place, hard tissue is laid down and the resultant tooth, when it erupts, is very much wider than normal. This process is called gemination (Figure 12.2) and unlike fusion, the number of teeth present is normal.
Double teeth of either variety are generally characterised by a vertical labial groove which often becomes carious, and hence fissure sealing at an early stage would be beneficial. Where these teeth have separate roots and a substantial crown, the tooth can be split and allowed to continue as separate teeth. However, more often than not, there is a single but somewhat expanded root, which makes separation impossible and, in view of the aesthetic and local crowding implications of having a much wider tooth in the dental arch, an extraction and management of the resultant space would be the usual treatment.
Dens in dente (dens invaginatus)
This literally means a ‘tooth within a tooth’ and is commonly seen in permanent maxillary lateral incisors. It arises due to prolific growth of the layers of ameloblasts and odontoblasts which are mapping out the palatal surface of the tooth. In order to accommodate the exuberant growth, there is a fold in the sheet of cells which causes an inward (towards the pulp) growth. Enamel and dentine are deposited in this new shape and essentially form a blind channel with an opening on the cingulum pit. Clinically this may be recognised as a deep pit or fissure in this area of the tooth. As with pits and fissures elsewhere in the mouth, this area is susceptible to caries. On other occasions, where the enamel and dentine in the depth of the channel have failed to form properly, the pit provides a direct opening into the pulp. When this happens and no preventive or remedial action has been taken, the patient will have problems owing to direct infection of the pulpal tissues from the oral cavity. It would therefore be important that this is diagnosed at an early stage, preferably as soon as the tooth erupts, and that the cingulum pit or fissure is fissure sealed. If there are signs of early caries then this must be treated accordingly.
Dilaceration
A dilacerated tooth is one in which the crown is bent at an angle to the roots. It occurs most commonly in the upper central incisors as a result of trauma from primary incisors.
Enamel pearls
These are small nodules of enamel which form typically on the buccal root surface.
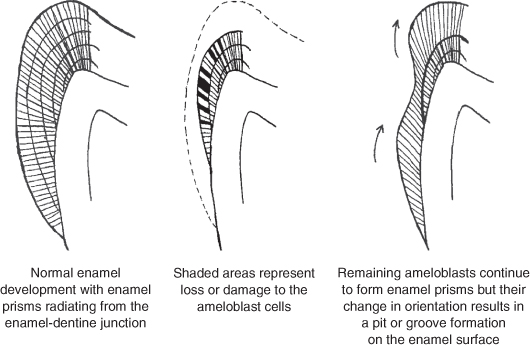
Abnormalities of tooth structure
Enamel and dentine, as previously mentioned, are formed by ameloblasts and odontoblasts respectively. Although this is a continuous process, there are two distinct stages. The first is the formation of an organic matrix which acts like a framework for the second stage; the second stage is the mineralisation phase, whereby the hydroxyapatite crystals are deposited to form the hard tissue. Disturbance of matrix formation will lead to deficiencies in the enamel bulk and may result in hypoplastic pits or thin enamel (Figure 12.3).
Figure 12.3 Development of hypoplastic pits in enamel.
Problems with mineralisation will affect the amount of enamel deposited in the matrix and, therefore, although there may be normal enamel thickness, there will be discoloured areas of hypomineralisation. These disturbances may be localised and affect only one or two teeth, or they may be generalised and affect most if not all the teeth. Inherited or acquired disturbances of tooth structure including amelogenesis imperfecta and dentinogenesis imperfecta are fully described in Chapter 3, p. 68–69.
Where a child suffers from an inherited condition, such as amelogenesis imperfecta, considerable restorative treatment is required to maintain function and appearance. In the young child interim measures, such as simple restorations, stainless steel crowns or composite veneers, may be required; these may progress to full-coverage crowns and porcelain veneers later.
Dental caries
Dental caries, despite being the commonest disease in humans, is a complex multifactorial phenomenon with three main factors which contribute to its pathogenesis (see Chapter 4).
Dental plaque is essentially a mucopolysaccharide film with elements derived from the saliva and microorganisms which reside in the oral cavity. The plaque microflora, despite being derived from the oral flora, is a selection of different bacteria in type and quantity. Dental plaque contains bacteria that are acid producing, with Streptoccocus mutans being the most important member in terms of caries production. Lactobacilli are also implicated in the process and rapidly increase in number as the carious process becomes established.
Diet is the single most important factor in the whole process as a substrate is produced from fermentable carbohydrates. Diet is particularly significant in children since they have more taste buds than adults (the average adult has <10 000), and frequently demonstrate a particular craving for sweet things, although this diminishes with adolescence. Sugars such as sucrose are readily implicated, but other products such as starch can be broken down by plaque bacteria to form sugars, which in turn produce various acids, the chief one of which is lactic acid. The acids so produced dissolve the hydroxyapatite crystals that form the enamel structure. All fermentable carbohydrates can be converted to acids in plaque, but sugars such as sucrose are rapidly changed, whereas starch products involve an additional step in the conversion and therefore take longer.
Host factors play an important part in caries initiation and prevention as they alter the resistance of the individual to caries attack. The quality of enamel, dentine and cementum may differ from person to person which results in differing caries susceptibilities. The quality and flow of saliva are extremely important. Saliva contains biochemical complexes, which help to buffer plaque acids, thus reducing or eliminating demineralisation of the enamel. Saliva may also be rich in calcium and phosphate ions which help to remineralise areas almost immediately and therefore reverse the caries process. Also a good flow of saliva aids the removal of not only substrates from the mouth, but also any plaque acid that has been formed.
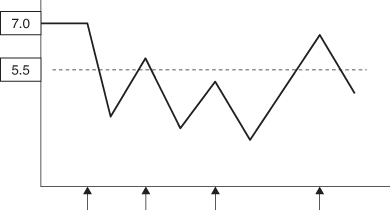
The interplay of these three factors leads to either demineralisation or remineralisation. Any fermentable carbohydrate challenge in the form of a snack, sucrose drink, etc. will lead to plaque acid production, resulting in demineralisation initially at microscopic level. The calcium and phosphate ions that are released are held in the plaque and saliva and, should the acid environment in the plaque disappear within a short space of time, then the calcium and phosphate ions reform the crystalline structure of the enamel. Thus this system of damage and repair or, more strictly, demineralisation and mineralisation normally maintains a balance. Where the balance is disturbed with more demineralisation than remineralisation, then the resultant destruction produces the typical carious lesion and cavitation. The Stephan curve (Figure 12.4) illustrates the increase in plaque acidity (or fall in pH) following a single fermentable carbohydrate intake. After its consumption, there is an elimination of the acid and a return to normal plaque pH at which time any destruction of the microscopic enamel structure is repaired. If, however, fermentable carbohydrate intake is frequent throughout the day, then the acidic or low pH of the plaque is maintained for longer periods with considerable demineralisation occurring and this amount of destruction cannot be remineralised as before (Figure 12.5).
Figure 12.4 Stephan curve showing fall in plaque pH from a resting state of 7.0 to below the critical level of 5.5 (indicated by dotted line) following a single intake of fermentable carbohydrate as indicated by the arrow. The portion below the dotted line represents the amount of demineralisation that occurs.
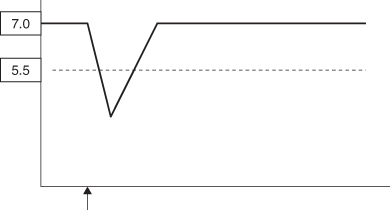
Figure 12.5 Stephan curve after multiple fermentable carbohydrate intakes. It can be seen that the plaque pH stays below the critical level of 5.5 for a long period and this amount of demineralisation is not reversible.
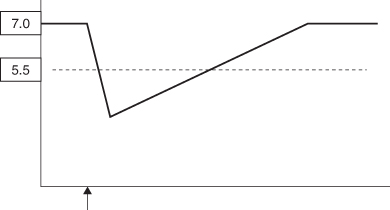
It should also be remembered that remineralisation and repair will only take place when the plaque pH rises to above 5.5 and the longer the period of acidic conditions, the more likelihood of caries developing. Where foods have a particular adherence, for instance sticky toffee, etc., or where there is a poor salivary flow as a result of medication (e.g. antihistamines) or treatment (radiotherapy), or a reduced salivary flow (during sleep), a single fermentable carbohydrate intake can tip the balance towards demineralisation (Figure 12.6).
Figure 12.6 Stephan curve showing fall in plaque pH from a single fermentable carbohydrate but where it is retained in the mouth for a longer period than normal. The slower elimination of plaque acid leads to an increase in demineralisation.
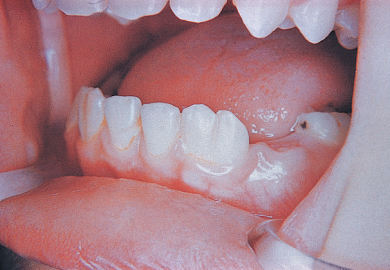
Where the process is rapid it is often referred to as ‘rampant caries’. This condition usually occurs in very young children where the sugar intake is both high and frequent. The causative agent is often fruit juices or similar containing sucrose, given in a feeding bottle. The drink is given over long periods on demand and often the child falls asleep with the feeding bottle in his/her mouth. Thus the upper anterior teeth are constantly bathed in the sucrose condition and, with the child falling asleep, there is even less opportunity for elimination of the drink or the plaque acid from the mouth. Because this usually occurs in very young children who are still using a feeding bottle, the condition has also been referred to as ‘nursing caries’ (Figure 12.7).
Prevention of dental caries
Prevention is important for all patients, but there are certain factors which render individuals, especially children, very much more at risk, and it is perhaps prudent to target these individuals or groups. These may be general or local factors. General factors include:
- Low socioeconomic groups.
- Medically and physically compromised patients.
- Special needs children.
Local factors include:
- Existing caries experience.
- Excessive periods of sugar intake per day.
- Poor oral hygiene.
- Conditions where there is a poor salivary flow.
- Orthodontic appliance therapy.
Figure 12.7 ‘Nursing caries’ affecting maxillary upper primary teeth.

Diet modification
By far the most important factor in caries initiation and propagation is the effect of diet, as described above. It is therefore not surprising that dietary analysis and modification form the mainstay of any caries preventative programme. Parents often fail to recognise the relationship of their child’s diet and their caries experience and frequently dispute the fermentable carbohydrate intake. This may be because they assume that it is the consumption of sweets which is entirely responsible and are unaware that other foods, including snacks such as crisps, etc., are also implicated. In addition, most processed foods contain hidden sugars. The term ‘hidden’ is somewhat unfair in that the food manufacturers will argue that the amount of sugar is listed on the labelling. However, usually these are foods which parents do not readily consider as causing tooth decay. Another reason why parents underestimate the dietary effect relates to the importance of frequency of consumption rather than the total consumed. Thus a quantity of sweets consumed over a short period is less detrimental than a smaller amount spread over a longer time.
In order to be able to provide advice regarding the diet it is necessary to examine what is being consumed. This is achieved by the completion of a diet diary which records all food, drinks and snacks consumed over usually a period of 3 days. One of the days should be a weekend day as the eating pattern may be different from a weekday or a school day. It is essential that the diet diary is filled in at the time that the food or drink is consumed. To complete the diary retrospectively at the end of the day or at the end of the 3-day period is likely to lead to omissions of between-meal snacks and drinks which may have become a subconscious routine but, of course, are very important in the analysis. Figure 12.8 illustrates an example of a diet diary.
There are many ways in which a dietary diary may be analysed. The simplest is to identify to the parent and child the good and bad aspects of the record, pointing out the decay-producing foodstuffs and the frequency. A more effective way is a more detailed analysis which differentiates mealtime and between-meal snacking, using a scoring system for acid attacks on the teeth as follows:
| Score | |
| Main meal | 2 |
| Main meal + brushing | 1 |
| Between meal snacks | |
| Food or drink consumed within a 5-minute period (e.g. biscuits, sweets, fruit cordial, etc.) | 1 |
| Food consumed over longer than a 5-minute period | 2 |
Table 12.2 illustrates the analysis of a typical caries-prone child for a single day using the above scoring system. It can be seen that there have been 12 acid attack episodes, which can realistically be reduced to the recommended maximum of five. This is a very simple way of analysing the data which produces targets which are easily understood and can be achieved. It is important that the whole process is conducted in an informative way and that neither the parent nor child are made to feel intimidated.
Fluorides
The use of topical and systemic fluoride is fully described in Chapter 11, p. 225–229.
Fissure sealants
Fissure sealing became popular from the early 1970s and the technique was made viable by the introduction of the acid-etch technique, which enabled materials, such as dental resins, to be attached to the enamel surface without the need for mechanical preparation of the tooth. The principle of fissure sealing is based on the concept that the occlusal fissure pattern of, particularly, first permanent molar teeth and, to a lesser extent, the premolars and second molars is very susceptible to becoming carious. Indeed, epidemiological studies have demonstrated the high caries prevalence of these clinical sites. By taking a sound tooth and covering the fissure system with a resin, this very vulnerable area of the tooth remains protected as it becomes much easier to keep plaque-free than before. Although fissure sealing has been regularly used for over 35 years, the idea of protecting a sound tooth is not new. Almost 50 years before the first fissure sealant had been developed, an American, Thadeus Hyatt, advocated a technique which he called prophylactic odontotomy. This essentially involved taking a sound tooth and preparing shallow occlusal cavities, predominantly in enamel, which eliminated the fissure system. The tooth was then filled with amalgam. Whilst prophylactic odontotomy had is proponents, it was not an idea that received much support, and in some ways it was rather illogical to place an amalgam filling in a tooth to prevent caries which, if it had occurred, would need an amalgam filling.
Figure 12.8 Typical diet diary.
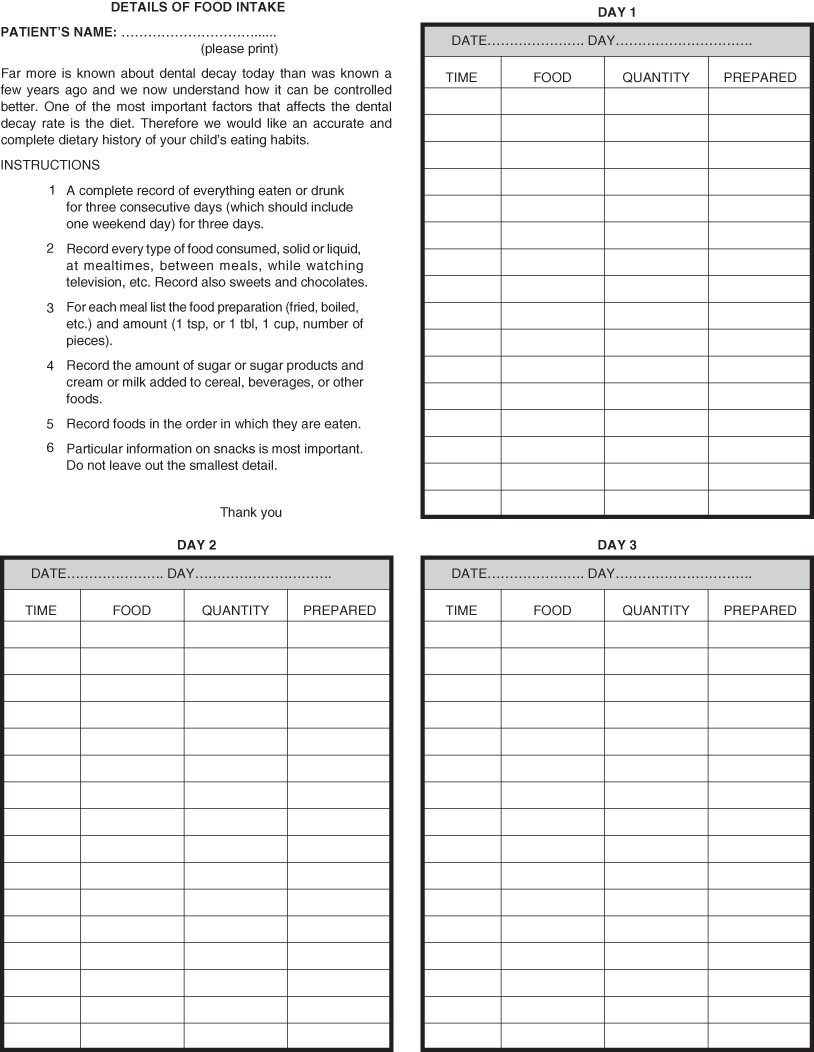
Table 12.2 Acid exposures of teeth.
| From diet diary | Recommended | |
| Breakfast | 1 | 1 |
| Between meals | 2 | 0 |
| Lunch | 2 | 2 |
| Between meals | 3 | 0 |
| Dinner | 2 | 2 |
| Bedtime snacks | 2 | 0 |
| TOTAL | 12 | 5 |
Not all children will develop fissure caries and therefore it would not be cost effective to carry out the procedure on all paediatric patients. The British Society of Paediatric Dentistry (2000) published guidelines regarding the use of fissure sealants. These are summarised below.
Patient selection indications include:
- Children with impairments, especially where the condition gives rise to problems as a result of developing dental disease or in providing treatment.
- Children who have caries experience, as judged by the existence of two or more cavities in the primary dentition. Susceptible sites on the permanent teeth should be sealed.
Tooth selection indications include:
- Deep fissures.
- Where caries exists in one or more of the permanent teeth. The other susceptible sites on the remaining permanent teeth should be sealed.
- A stained fissure that is not deemed to be carious by clinical and radiographic examination.
Modern fissure sealants may be Bis-GMA resins similar to composite resins, or they may be glass ionomer or a mixture of glass ionomer and composite resin. All these materials utilise the acid-etch technique, which creates microscopic pores in the enamel surface and into which the resin flows and provides the micromechanical retention that holds the sealant in place. The added benefit of sealants containing glass ionomer is that there is some fluoride in this material which in turn can cause further protection to the dental tissues. The long-term success for glass ionomers used as fissure sealants is, however, questionable.
The technique of fissure sealant application is fully described in Chapter 11, p. 230–231.
Regular review of the fissure sealant is important to ensure that:
- It remains intact. Where it is lost it will need to be replaced and where there is partial loss then it will need to be replenished.
- Caries has not been inadvertently sealed under the fissure sealant as demonstrated by colour changes observed through clear fissure sealants or by the use of bitewing radiographs.
Plaque control
Whilst diet modification remains the most important aspect in caries prevention, it has to be remembered that it is the microbiological activity in plaque that results in the conversion of sugars to acids. Therefore any removal of plaque will not only maintain good gingival health, but also have an effect in reducing caries. An example of the latter is the decalcification that occurs around orthodontic brackets when plaque removal has not been as thorough as it should have been.
Tooth brushing remains the main method of plaque control in children and, with the use of toothpaste as previously described, provides a very convenient vehicle for fluoride. However, it requires both a reasonable degree of manual dexterity and also motivation, two factors that young children below the age of 6 years probably do not possess. It is therefore important that parents carry out this routine for their children and, in so doing, not only effect efficient plaque removal but also instil the habit of good oral health for the future. Older children may have developed the skills but perhaps the motivation may be lacking and parental supervision is advisable.
Monitoring of the efficacy of tooth brushing is aided by the use of plaque-disclosing tablets or solutions which essentially are harmless vegetable dyes. Plaque will be stained usually red and give a clear indication to the child and parent of areas in which more concentration is required. The use of plaque indices as a method of quantifying the amount of plaque on the teeth can be quite helpful. The score is usually given as a percentage and whilst it lacks scientific validation, it nevertheless provides a target for the child and parents by which future improvement in tooth brushing may be measured. Other methods of plaque removal such as the use of floss are inadvisable in a young child, as injudicious use can lead to gingival damage.
Tooth wear in children
Gradual loss of the tooth surface has, in the past, been associated with an ageing process and therefore was considered to be related to advancing years. However, in recent years, this has become a recognised problem in children and was first included in the Children’s Dental Health in th/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


