Melolabial Flaps
Introduction
Because of the proximity of the melolabial fold to the nose and lips, melolabial flaps have long been used to repair these structures.1,2 During the 19th and 20th centuries, many varieties of melolabial flaps were described.3 In the past, such flaps have been called nasolabial flaps, but the term melolabial is more accurate in description as the prefix melo- refers to the cheek and the suffix -labial refers to the lips. Thus, it is more accurate to use the term melolabial crease rather than nasolabial crease because the crease separates the lips from the cheek, not the nose from the lip. This chapter discusses only cutaneous flaps harvested from the mound of skin immediately lateral to the melolabial crease and known as the melolabial fold.
Local cutaneous flap classification and terminology are discussed in detail in Chapter 6, but a brief summary here is helpful in understanding the mechanisms of movement of flaps harvested from the melolabial fold. Classification of flaps by method of transfer, which is to say by tissue movement, is usually the most convenient way of discussing flaps relative to their use in repair of facial cutaneous defects.4–6 It also contributes to the understanding of where standing cutaneous deformities develop and where the maximum wound closure tension occurs during wound repair. By use of this classification, melolabial flaps may be categorized as pivotal, advancement, and hinge. Melolabial hinge flaps are rarely used and are not discussed in this chapter. Advancement in the majority of situations depends on stretching the flap skin in the direction of flap movement. Such flaps are subjected to an increase in wound closure tension. In contrast, pivotal flaps rotate about a point at their base and in their purest form are not stretched. Thus, they are not subjected to wound closure tension greater than the natural tension of the remaining facial skin, although the repair of the donor site of the flap is subjected to increased tension. There are three types of pivotal flaps: rotation, transposition, and interpolated. Transposition and interpolated flaps may be transferred on a cutaneous pedicle or subcutaneous tissue pedicle. In the latter case, the flap is referred to as an island flap because it has no cutaneous connection to the donor site. Island transposition pivotal flaps are occasionally harvested from the melolabial fold but are uncommonly used and are not discussed. Rotation flaps are pivotal flaps with a curvilinear configuration. They must be designed immediately adjacent to the defect and are best used to close triangular defects. In the author’s practice, local flaps in the form of rotation are rarely designed in the area of the melolabial fold because their curvilinear incision frequently creates a scar that crosses the melolabial crease perpendicular to relaxed skin tension lines (RSTLs). For this reason, rotation flaps are not discussed.
Melolabial Transposition Flaps
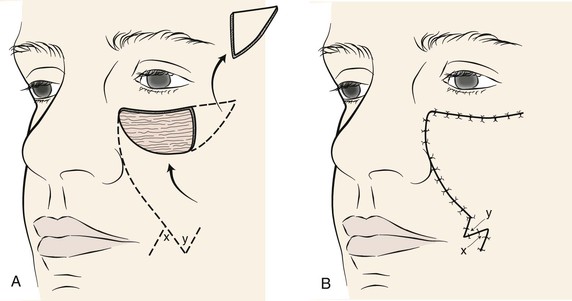
The majority of melolabial transposition flaps are designed as a rectangle, parabola, or rhombus. The axes of these flaps are usually oriented along or are parallel to the axis of the melolabial fold (Fig. 12-1). Closure of the flap donor site is within or parallel to the melolabial crease. The flap may be lengthy relative to its width, which facilitates closure of the donor defect without excessive wound closure tension. Melolabial transposition flaps used to repair small (2 cm or less) cutaneous defects of the medial cheek may be based superiorly or inferiorly. However, transposition flaps used to repair medial cheek defects larger than 3 cm should be based superiorly because there is more redundancy of facial skin in the inferior cheek, in the region of the jowl. In older patients, this redundancy can provide a source for a large flap and still enable primary closure of the donor site. Flaps should be designed so that whenever possible, closure of the donor site is in the melolabial and labial mandibular creases. When superiorly based melolabial transposition flaps are used, the standing cutaneous deformity is removed just medial or lateral to the superior border of the defect, depending on whether the flap is pivoted medially or laterally.
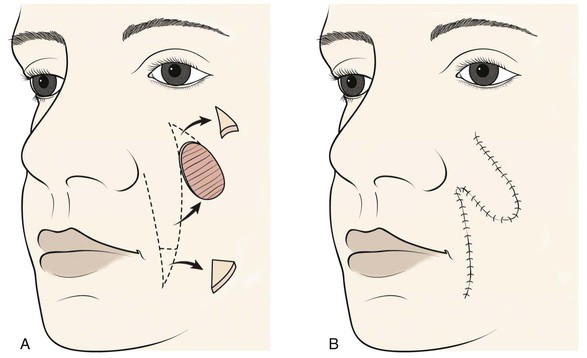
FIGURE 12-1 A, Skin defects of medial cheek can be repaired with melolabial transposition flaps. Broken line outlines incision for flap. B, Standing cutaneous deformities removed from base of flap and cheek donor site on flap transfer and closure of donor site.
Transposition flaps are pivotal flaps, and the greater the arc of pivotal movement, the greater will be the size of the standing cutaneous deformity and the less will be the effective length of the flap (see discussion in Chapter 8). The reduction in effective length must be accounted for in designing melolabial transposition flaps so that greater pivoting requires a longer design of the flap. To limit this restricting factor, whenever possible, melolabial transposition flaps should be designed to pivot no more than 90°.
Melolabial Advancement Flaps
Melolabial Unipedicle Advancement Flaps
Unipedicle advancement flaps are created by parallel incisions that allow a sliding movement of skin in a single vector toward the defect. This movement is in one direction, and the flap advances directly over the defect. As a consequence, the flap must be developed adjacent to the defect, and one border of the defect becomes the leading border of the flap. Melolabial advancement flaps are not frequently designed with two parallel incisions. When they are used to repair skin defects of the superomedial cheek, melolabial advancement flaps are usually designed by making only one long incision in the melolabial crease and undermining the skin of the fold lateral to the incision (Fig. 12-2). Skin is then advanced upward in a vector parallel to the melolabial crease with some additional slight pivotal movement. The pivotal movement, although limited, eliminates the need to make the second incision parallel to the first incision to create and to move the flap. A standing cutaneous deformity is excised lateral to the skin defect parallel to the inferior bony orbital rim.
Melolabial Island Advancement Flaps
The melolabial V-Y subcutaneous tissue pedicle island advancement flap is an option for repair of medial cheek skin defects at or below the level of the nasal alae.7 The flap is particularly well suited for skin defects located immediately adjacent to the alae (Fig. 12-3). A triangle-shaped skin island is designed with the base of the triangle formed by the inferior margin of the defect. Optimally, the vector of flap advancement is designed parallel to the melolabial crease. The width of the skin island should equal the width of the defect at its widest point. The height of the skin island should generally be twice the height of the defect. The trailing half of the skin island tapers to a point to facilitate donor site closure in a V-Y fashion after flap advancement. The flap is therefore sometimes referred to as a V-Y island advancement flap. The skin island may extend as far as the inferior border of the mandible if necessary. Positioning the inferior tip of the skin island directly in the melolabial crease optimally conceals the donor site scar. Insofar as possible, incisions should be designed so that their scars are parallel to or in borders of aesthetic regions.
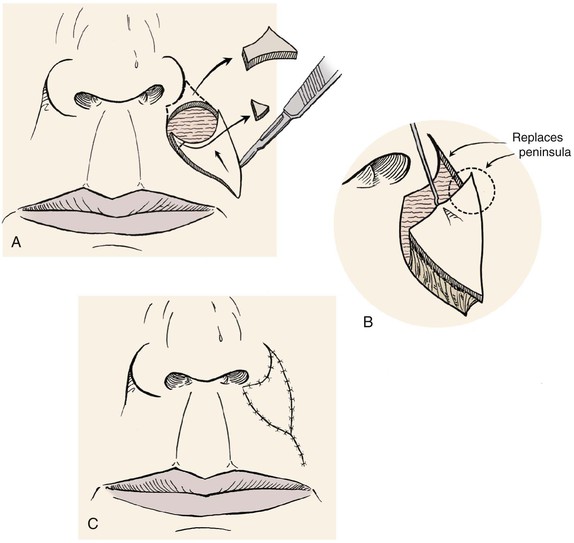
FIGURE 12-3 Melolabial subcutaneous tissue pedicle island advancement flaps are particularly suited for repair of skin defects adjacent to alar base. A, Defect enlarged to remove peninsula of skin between ala and melolabial fold. Island flap designed to replace skin peninsula. B, Flap is based on subcutaneous fat of melolabial fold. C, Superior and lateral portions of wound closure suture lines are in aesthetic boundaries.
The perimeter of the skin island is incised to the level of the superficial subcutaneous fat. Undermining of the adjacent facial skin for a distance of 2 cm is performed at this level. Blunt and sharp dissection is then carried through the subcutaneous tissue surrounding the skin island, beveling slightly away from the skin island down to the level of the fascia overlying the facial muscles. This frees the elastic subcutaneous tissue pedicle from its medial and lateral fibrous attachments to the surrounding cheek fat while preserving its vascular supply, which is derived from its deep attachments. The skin island is then advanced toward the defect by placing a skin hook at its leading border. At this point, the pedicle can be narrowed to facilitate the advancement of the flap. This is accomplished by back cutting the peripheral borders of the flap in the subcutaneous tissue plane, leaving at least one-third of the total flap surface area attached to the underlying subcutaneous tissue. Further thinning of the subcutaneous tissue of the undermined leading border of the flap may be performed to create an appropriate thickness match between the border of the flap and the recipient site. A central pedicle attached to at least one-third of the total skin island surface area will adequately perfuse the flap. Further subcutaneous undermining of the skin adjacent to the flap is required if puckering of the peripheral facial skin occurs with flap mobilization (see Fig. 12-3). Subcutaneous undermining is also performed at the recipient site. In addition, the recipient site’s depth and shape may be modified by removing skin and subcutaneous tissue so that scars will be positioned along aesthetic boundary lines and the defect will more appropriately accommodate the thickness of the advancement flap. The leading border of the skin island is fixed in place, and the wound surrounding the remaining perimeter of the flap is subsequently closed such that wound closure tension is equally distributed over the entire length of the flap. The flap donor site is closed in a V-Y fashion, with care taken to compensate for any differences in the length of the opposing margins of the donor site by suturing on a bias (see Chapter 6).
For sizeable (2-3 cm) lip skin defects adjacent to the inferior border of the ala, it may be beneficial to excise the small peninsula of skin between the ala and melolabial fold in the process of enlarging the defect so that it extends to an aesthetic boundary.8 The peninsula is then reconstructed by appropriately designing the island flap so that the superior portion of the flap replaces the peninsula (see Fig. 12-3). This technique provides the best scar camouflage because the superior border of the flap is positioned within the aesthetic boundaries of the alar-facial sulcus and melolabial crease. When this peninsula is not replaced, the flap must cross the base of the peninsula and may mar an otherwise excellent result.
Melolabial Interpolated Subcutaneous Tissue Pedicle Flaps
Melolabial transposition flaps have frequently been used for reconstruction of the ala and nasal sidewall. They have the advantage of maintaining a lymphatic drainage route through the pedicle of the flap, which remains in continuity with cheek skin. They also avoid a circumferential scar, which in part accounts for trap-door deformity. Why not use a transposition flap instead of an interpolated flap for ala repair? Both flaps have the advantage of using skin with color, texture, sebaceous glandularity, and thickness similar to those of the natural skin of the ala. Both flaps leave an acceptable donor scar in the depth of the melolabial crease. The main reason for not using a melolabial transposition flap is that it deforms the alar-facial sulcus and lateral portion of the alar groove. A portion of the flap by necessity must pass through the superior aspect of the alar-facial sulcus, which represents an important topographic junction between the facial aesthetic regions of the nose, cheek, and upper lip. Whenever possible, local flaps should be designed so that they do not cross borders that separate aesthetic regions. This is especially true if the border has a concave topography, like that of the alar-facial sulcus.9 Too often, this sulcus has been violated by transposition flaps harvested from the cheek to reconstruct lower lateral nasal defects. The flap passes through the sulcus, obliterating the valley between the ala and cheek. When this happens, it is extremely difficult to restore the valley to a completely natural contour. For this reason, an interpolated melolabial flap is recommended for reconstruction of the ala. The pedicle of the flap does not extend through the alar-facial sulcus, it crosses over the sulcus. The pedicle may consist of skin and subcutaneous fat or subcutaneous fat only and is detached from the cheek 3 weeks after the initial transfer to the nose. Although 3 weeks is a lengthy period for the patient to endure the deformity caused by the attachment of the flap’s pedicle to the cheek, this interval enables the surgeon to thin and sculpt the subcutaneous tissues of the distal flap at the time of flap transfer and the proximal portion of the flap at the time of pedicle detachment and flap inset. On inset of the flap, the patient is left with a completely natural alar-facial sulcus because no incision or dissection has been performed in this region. Because of this advantage, I recommend the choice of an interpolated design when a pivotal cheek flap is planned for reconstruction of a defect of the ala and the defect does not extend laterally to the alar-facial sulcus (Fig. 12-4).10
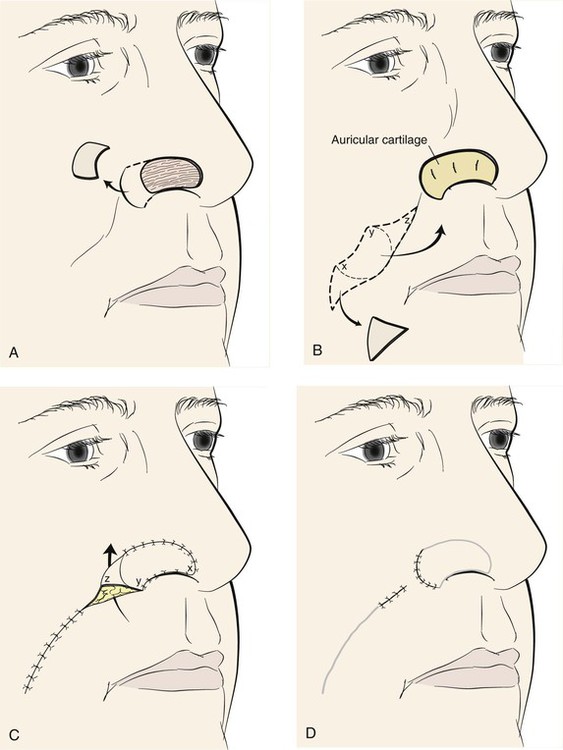
FIGURE 12-4 A, Skin defect of ala. Remaining skin of aesthetic unit removed. B, Auricular cartilage graft used for structural support of ala. Interpolated melolabial flap designed for covering of cartilage graft. Flap pivots toward midline. C, Subcutaneous tissue pedicle of flap crosses over alar-facial sulcus, necessitating subsequent division of pedicle. D, Second stage consists of division of pedicle and flap inset.
The nasal-alar unit is highly contoured, has a free margin, and functions as the external nasal valve. In reconstructing the ala, consistent results require a cartilage subsurface framework to resist the forces of scar contraction, to provide a stable external valve, and to serve as a scaffold for contour. The framework in the form of a cartilage graft must be used at the time of the initial reconstructive procedure and requires vascularized tissue superficial and deep to the graft, totally enveloping the cartilage. Adequate function of the nose requires a thin internal layer most appropriately supplied by vascularized mucosa.11 The external covering flap is provided by an interpolated cheek or forehead flap. Lining flaps and structural grafts for defects of the nose are discussed in detail in Chapter 18.
The porous and sebaceous nature of medial cheek skin closely resembles that of the caudal third of the nose, so an interpolated melolabial flap is generally the preferred covering flap for alar reconstruction. The flap is based superiorly on the rich vascular supply in the region of the alar-facial sulcus described by Herbert.12 At this location, perforating branches from the angular artery penetrate the levator labii muscle. Other perforating vessels on both borders of the midportion of the zygomatic major muscle assist in supplying the cheek skin adjacent to the ala. The flap may be designed as a peninsular flap based superiorly on a cutaneous pedicle or as an island based on a subcutaneous tissue pedicle. In most circumstances, I prefer to design the flap as a crescent-shaped island of skin based on a subcutaneous tissue pedicle. The superior extent of the island remains 5 mm below the alar-facial sulcus, preserving this important aesthetic area.9
An exact template of the alar unit is made from the contralateral normal side with a malleable material such as foil or a thin sheet of foam rubber. The template is reversed to design the interpolated cheek flap. When the defect extends beyond the confines of the ala into another nasal aesthetic unit, the template is designed slightly smaller than the defect to accommodate the phenomenon of distraction of wound margins, which creates an open wound that is larger than the surface area of the skin removed. If excision of additional skin is indicated to resurface an adjacent nasal aesthetic unit, the template is fashioned before the remaining skin is removed because of this same phenomenon. Alternatively, the contralateral intact nasal aesthetic unit can be used to design the template.
When the ala is reconstructed with a melolabial flap, the entire ala is resurfaced with the cheek flap, except for 1 mm of alar skin just anterior to the alar-facial sulcus (see Fig. 12-4). This small skin tag preserves the alar-facial sulcus and often provides a better scar than when the flap extends to the sulcus. This approach is similar to the method recommended by Sheen and Sheen13 for performing a type II Weir excision to reduce the size of the nasal base. Maintaining the excision outside of the alar-facial sulcus lessens the risk for development of a depressed scar. This approach also avoids the technically challenging requirements of integrating the flap into the nasal sill at the time of flap inset. When using cheek flaps for repair, I often delay excision of the extreme lateral portions of the residual alar skin until the time of pedicle detachment and flap inset. This delay reduces the wound tension on the flap at the time of initial transfer.
The fashioned template is placed on the melolabial fold so that the center of the flap is positioned 1 cm above the horizontal plane of the oral commissure. The template is positioned so that the medial border of the designed flap lies in the melolabial crease. This arrangement ensures that the flap is harvested from the cheek, not the lip, and that the donor site wound closure will lie within the melolabial crease, providing maximum scar camouflage. The flap is designed to pivot 90° toward the midline in a clockwise direction when it is harvested from the left cheek and counterclockwise when it is harvested from the right cheek. Thus, the template is positioned to design the flap with a specific orientation. As the flap is pivoted and transferred to the recipient site, the medial border of the in situ flap is sutured to the cephalic border of the nasal defect. This in turn causes the inferior border of the in situ flap to join the anterior border of the defect. The lateral border of the in situ flap becomes the inferior border of the reconstructed ala (see Fig. 12-4).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses