12 Lasers in Pediatric Dentistry
In 1960, Dr. Theodore Maiman, working on the theory of light amplification proposed by Albert Einstein, created the first laser.1 Eighty years after Einstein’s 1917 paper, the first erbium laser for hard tissue dental use was cleared for marketing by the U.S. Food and Drug Administration (FDA). Since that time, dentistry has undergone dramatic changes in the way both soft tissue and hard tissue disease and abnormalities are treated. In pediatric dentistry, the primary goals are the prevention and the interception of oral diseases and soft tissue abnormalities without making patients reluctant to visit the dentist. If these twin goals of prevention and interception are not attainable, clinicians restore diseased teeth and repair or eliminate soft tissue conditions.
Laser Types
Erbium Family of Lasers
The development of the erbium family of lasers (Er:YAG and Er,Cr:YSGG) has made the treatment of children safer and easier. Laser-assisted dental care has changed the way dentists prepare diseased teeth, ablate bone, and treat soft tissue abnormalities and diseases. An entire new standard of care is becoming a reality. The erbium lasers have helped create a positive treatment atmosphere, with most pediatric patients undergoing dental caries treatment without fear.2,3
The benefits of lasers have become well documented over the past decade. The erbium lasers provide an alternative to conventional drilling and filling, while often allowing a dentist to use the high-speed or slow-speed handpiece to complete procedures (e.g., extensive alloy preparations) without the need for local anesthesia. Erbium lasers have the unique ability to ablate hard tissues (bone, dentin, enamel) as well as perform soft tissue procedures.4–7 With similar capabilities, the erbium family of lasers includes the 2940-nm erbium-doped yttrium-aluminum-garnet (Er:YAG) and the 2780-nm erbium, chromium–doped yttrium-scandium-gallium-garnet (Er,Cr:YSGG).
Soft Tissue Lasers
Complementing the erbium lasers is a second group, the soft tissue lasers. A variety of laser wavelengths are useful for soft tissue procedures. The primary soft tissue lasers currently used include the carbon dioxide (CO2),8,9 neodymium-doped YAG (Nd:YAG),10 and the diode lasers.11,12 These soft tissue lasers have no capability to ablate hard tissue. Although Nd:YAG lasers have FDA clearance for ablating first-degree caries in enamel, the process is extremely slow and tedious and has essentially been replaced by the erbium family of lasers.
Low-Level Lasers
The third group of lasers useful in pediatric care are the photobiostimulating (PBS), or low-level, lasers.13–15 Wavelengths of CO2, diode, erbium, and Nd:YAG lasers are classified by the FDA as Class IV lasers because of their ability to ablate tissue. However, the FDA classifies low-level (PBS) devices as Class III lasers with “no significant risk” (NSR) because they produce less than 500 mW of energy. The photobiostimulatory effects of these lasers are usually labeled low-level laser therapy (LLLT).
Outside of dentistry, the FDA has cleared low-level laser use in medicine for conditions such as carpal tunnel syndrome and for pain management. Dental applications at this time should be considered off-label use (not cleared by FDA). Although these low-level lasers are safe, caution should be used, and contraindications include pregnancy, presence of malignancies, and use near the eye or, in some cases, over the thyroid gland16 (see Chapter 15).
Adjuncts and Benefits
Some degree of visual enhancement for the dentist is highly recommended when using lasers. Lasers enable the practitioner to perform microdentistry because the laser can remove minute areas of diseased hard tissue not readily visualized. When performing soft tissue procedures, it is beneficial to use magnification to view the surgical area.17,18 Loupes are one excellent option for enhanced visualization; however, the limitation of one magnification setting makes adding a dental operating microscope the optimal investment. The author has used a dental operating microscope since 2001 and finds children accept it without difficulty and remain quite still during dental procedures.
Lasers in Pediatric Dental Practice
Lasers have led to a reevaluation of dental cavity preparation and a fundamental change in the practice of restorative dentistry. We now need to reevaluate and often modify G.V. Black’s principle of “extension for prevention” with the concept of minimally invasive microdentistry. The use of erbium lasers for repair of incipient hard tissue disease provides a stress-free means of restoring teeth with minimal invasiveness and usually with no local anesthetic.19,20 Other benefits to the patient over conventional methods include reducing the number of office visits required for restorative procedures, decreasing healing time for soft tissue procedures, eliminating the need for suturing, and reducing the need for postoperative pain medication and antibiotics.
The effectiveness of using hard tissue lasers is safe and well documented in the dental literature. The Nd:YAG laser has limited usefulness in the treatment of dental caries but is cleared for removal of superficial pigmented caries.21 However, the erbium family is the laser of choice and most practical for deep enamel, dentin, and cementum caries removal. The erbium laser can be used for restoring primary and permanent teeth, again with minimal to no local anesthesia. In most cases, children will not require local anesthetic for Class I, II, III, IV, or V restorative procedures using bonded restorative materials.
Using the concept of minimally invasive restorative procedures, the erbium laser allows the operator to remove only diseased tissue, thus preserving much more of the healthy, unaffected tooth structure. Lasers also prevent the small microfractures that occur in enamel when using conventional dental handpieces. In cases where alloy restorations are preferred, the laser’s low-level analgesic effect may allow the dentist to create a restorative preparation using a conventional handpiece without analgesia. The erbium laser creates its ablation effect by being absorbed by water within the hydroxyapatite of the tooth structure. This heats up the water within the mineral, creating microexplosions of the hydroxyapatite out of the tooth. The erbium laser is absorbed by water, and decayed hard tissue has more water content than healthy hard tissue; therefore, erbium lasers are more specific for decay than conventional instruments. Conventional instruments (handpieces, air abrasion, spoon excavators) remove whatever is in their path. Erbium lasers preferentially remove higher-water-content (decayed) tissue, leaving the lower-water-content (healthy) tissue unaffected22 (see Chapter 11).
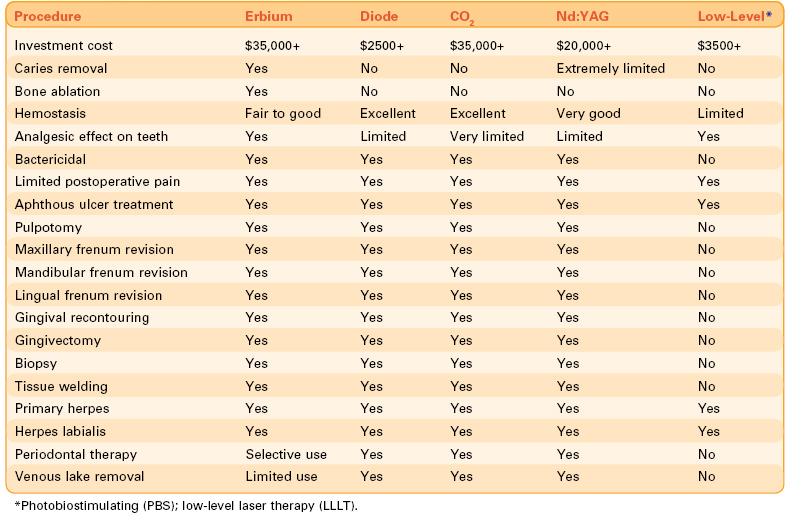
Table 12-1 lists the various uses of lasers in pediatric dentistry.
Hard Tissue Procedures
Analgesia for Sealant Placement and Caries Removal
Both surgical and low-level (PBS) lasers can produce an analgesic effect on teeth. The low-level laser is placed on the occlusal and root areas of the tooth to create this analgesic effect. A similar result may be produced using surgical lasers in the defocused mode for 2 to 3 minutes. Lasers using extremely short pulse durations are very efficient at producing this effect. Placement of sealants, preventive resin restorations, and Class I, Class III, and Class V caries removal may be completed using erbium lasers with minimal to no local anesthesia using this technique. When caries are deep, removing tooth structure with a high-speed or slow-speed dental handpiece with no local anesthetic or patient discomfort may also be performed with this technique. Low-level laser analgesia is technique sensitive (see Chapter 15).
Erbium Laser Caries Removal
Class II preparations are more time-consuming when using lasers; however, use of the correct parameters will allow the procedure to be performed successfully without patient discomfort. In general, preparing the tooth for a stainless steel or other type of crown is possible but not usually practical because this takes so long. Every erbium laser has different pulse durations, Hz/mJ settings, tip diameters (producing different spot sizes) of different materials, and different delivery rates of air and water through the handpiece. Therefore, it is impossible to include suggested settings for each procedure. However, the following generalities apply to all erbium laser operative dentistry procedures, based on how the erbium wavelength is absorbed by the target tissue, the spot size (see Chapter 2), and the erbium laser’s preferential absorption by water:
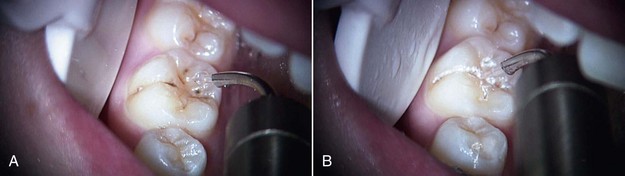
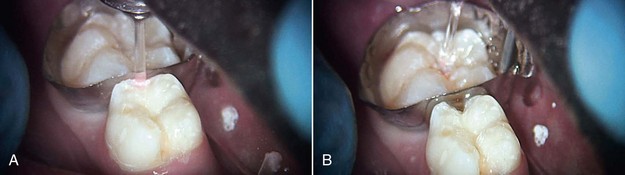
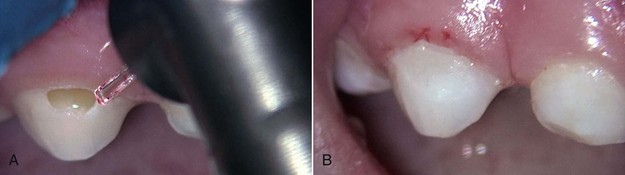
Figures 12-1 to 12-5 (pp. 206-207) show erbium laser removal of Class I to V caries. Figure 12-6 (p. 207) shows the result of conventional instrumentation using local anesthesia in a pediatric patient.
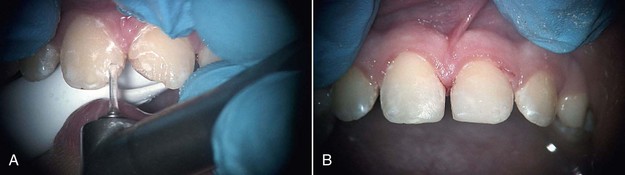
FIGURE 12-5 • A, Class IV erbium laser preparations on maxillary central incisors fractured due to trauma. B, Fractures restored.
Soft Tissue Procedures
A wide array of soft tissue procedures may be performed with lasers in the pediatric dental office.23–29 Erbium lasers may be used to accomplish many soft tissue procedures with little or no bleeding when used at lower energy settings than for hard tissue procedures, and without water spray. In some cases, however, a diode, CO2, or Nd:YAG laser is better suited for the procedure. Patients with bleeding disorders (e.g., von Willebrand disease, hemophilia) or those receiving anticoagulants (e.g., aspirin, warfarin) will benefit from the superior hemostatic ability of these lasers.
Pediatric soft tissue laser procedures include the following:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses