12
Dental Fear and Anxiety Associated with Oral Health Care: Conceptual and Clinical Issues
- Dental care-related fear and anxiety are related but distinct states that exist on continua and influence how and when a patient utilizes dental treatment.
- Fears and anxieties about dental treatment can develop via a number of mechanisms and manifest in diverse ways; they are highly individualized, complex phenomena which in extreme forms can meet criteria for Specific Phobia.
- Dental care-related fear and anxiety are prevalent global public health concerns that impact oral health, systemic health, psychological/emotional health, and quality of life.
- Appropriate and comprehensive assessment of dental care-related fear and anxiety is critical for understanding an individual patient’s experience, and necessary for successful reduction of the aversive states.
- A number of intervention strategies are available, including behaviorally, cognitively, educationally, and pharmacologically oriented methods, which can be used singly, or in combination, for effectively working with highly fearful and anxious patients.
Introduction
Fear, anxiety, worry, nervousness, and even disgust associated with the dental environment and oral healthcare professionals are global and ubiquitous phenomena that impact a diverse range of patients across the life span, with impact on family, friends, coworkers, and oral health professionals. This chapter focuses on dental anxiety and fear in adults and adolescents; these phenomena in children are of critical importance, given their developmental course and natural history from childhood leading into adulthood. Chapter 14 in this volume provides information about disruptive behavior in children in the dental operatory and its relation to fear and anxiety. So commonplace are the experiences of dental anxiety and fear, in fact, that they frequently are the topics of advertisements, newspaper cartoons, stand-up comedy routines, and everyday conversations (e.g., Sonis, 1997). While it may be a common experience, and even the focus of countless jokes, dental fear and anxiety are distressing, if not debilitating, over decades, for many patients, and are of significant clinical relevance for the dental professional. Dental fear and anxiety about dental care can be daunting barriers to the utilization of treatment.
Recognized as somewhat separate states that exist along continua in the general population, dental fear and anxiety may be so extreme that the patient can be diagnosed with a Specific Phobia, or a related behavioral health problem. While highly dental-anxious/fearful patients can be placed into general categories, there are innumerable unique manifestations. In spite of advancing dental treatment technologies, dental fear and anxiety appear to be at static levels from a population-wide perspective. Across the globe, dental fear and anxiety are associated with avoidance of oral health care, and so may best be conceptualized as dental care-related fear and anxiety. The avoidance behavior is linked to greater oral disease and poorer oral health-related quality of life, with implications for systemic health and quality of life in general, and is therefore a major public health problem worldwide. Understanding dental care-related fear and anxiety from both conceptual and clinical standpoints is critical for the oral healthcare professional. Appreciation of conceptual issues will inform assessment, management, and treatment of patients with high levels of dental care-related fear and anxiety.
Conceptual Considerations
Dental treatment is a potentially stressful experience for many, even most patients. Physical (e.g., potential for pain, being closed-in) and environmental/psychological factors (e.g., lack of predictability, loss of control) make the dental situation unique and often invoke stress (Eli, 1992). Undoubtedly, some procedures are especially stressful for a great majority of patients. For example, in patients generally (i.e., not necessarily those who are highly fearful/anxious), root canal therapy and the associated pain and stress results in transitionary changes in natural killer cell cytotoxicity and the subsequent development of infectious disease episodes within the following month (Logan et al., 2001).
Patients experience fear or anxiety not only during invasive procedures; in fact, patients also report experiencing fear and/or anxiety in the context of routine preventative procedures, including dental hygiene treatment (Gadbury-Amyot et al., 1996; Sullivan & Neish, 1998). Many aspects of dental treatment are perceived as uncomfortable, threatening, or disgusting by patients, including the sights, sounds, and smells associated with the dental clinic, injections, dental instruments, perceived lack of control and predictability, and dental/orofacial pain (McNeil & Berryman, 1989; de Jongh et al., 1994; Johnsen et al., 2003). Moreover, patients often feel embarrassment in regard to their anxious and fearful responses anticipating, or while receiving, dental care.
The terms “oral health care” and “dental treatment” are quite broad, and so elucidating what aspects of the general construct are emotionally evocative is important in defining the “universe” of what constitutes dental fear, anxiety, and phobia. Indeed, dental fear can be quite specific, as in the case of an otherwise generally comfortable patient who becomes in need of root canal therapy, or it can be generalized to almost all aspects of treatment, and can be part of another syndrome such as panic disorder with agoraphobia (although situationally bound panic attacks can occur in the context of a Specific Phobia of dental care). Injection fear is one important and common specific type of dental care-related fear (Milgrom et al., 1997). It can be highly circumscribed and encapsulated, but also is present in many (but not all) forms of dental fear and phobia. It can be restricted to oral injections, although it can be part of fear about injections in any part of the body. Many patients who experience injection fear also suffer from fears about other aspects of dental care. Given the nature of dental care, Blood-Injection-Injury (BII) Phobia can be provoked during oral health care. While there is some overlap clinically, particularly in terms of injection fears, research suggests that dental phobia is best conceptualized as a Situational Type of Specific Phobia, independent of the BII Type (de Jongh et al., 1998). Nevertheless, the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5; American Psychiatric Association [APA], 2013) seems to require the classification of Dental Phobia as a Specific Phobia with a blood-injection-injury code, which the DSM-5 text suggests is uniquely associated with vasovagal syncope, which certainly is not the case for many or most individuals with dental phobia. This change from the earlier edition of the DSM adds confusion to the literature, in that some authors have assumed or suggested individuals with dental phobia all should be classified with the BII Type. There is evidence to the contrary, however, supporting the notion that the Situational Type is the most common form of Specific Dental Care-Related Phobia (de Jongh et al., 1998; Leutgeb, Schäfer, & Schienle, 2011), although some individuals certainly would fit the criteria for BII Phobia.
In general, patients fear aspects of professional oral health care, with a few having anxiety or fear about self-care (e.g., toothbrushing). Evocative aspects of dental care are specific dental stimuli and experiences, such as being supine in the dental chair; pain, anticipation of pain, or memory of pain; sight and sound of the drill; and receiving injections, along with environmental factors, such as the lack of predictability and control, inability to easily “escape” or leave the dental setting, and (largely perceived) potential for infection.
Though dental patients may report both fear and anxiety about dental treatment, it is important to note that the two are phenomena that indeed are distinct from one another, although there likely is some overlap between them (McNeil et al., 1993; Poulton et al., 2001). This distinction between dental care-related fears and anxieties, as noted by Poulton et al. (2001) and Thomson et al. (2009), is one in need of further clarification and investigation. Many of the titles of current dental fear and anxiety instruments, as well as those evaluating fears and anxieties about pain, are misnomers, in that they purport to assess anxiety or fear, but in reality likely reflect some combination of both states.
Broadly speaking, dental care-related fear is a distressing emotional response to treatment-related stimuli, typically characterized by physiological responsivity, feelings and reports of apprehension and/or dismay, and avoidance. The fear literature suggests that it is a robust emotion, almost always defined by immediate onset, which usually involves a salient physiological component (e.g., Craske, 2003). A severe fear response may involve panic symptoms or even a panic attack in the dental clinic. Components that predispose a patient to panic attack are (a) an inability to escape easily; (b) a reduction in controllability; and (c) a reduction in predictability.
Dental care-related anxiety, though akin to dental care-related fear, is a more cognitively involved emotional response to stimuli or experiences associated with dental treatment. Generally, anxiety entails negative thoughts and worries, and with respect to exposure to evocative stimuli, often occurs distally in time (Craske, 2003). That is, dental patients are most likely to experience anxiety well prior to their dental visit as they consider elements of the dental visit that have caused or could cause discomfort, and this anxiety may wax and wane between appointments. Dental patients are most likely to experience fear immediately prior to and during the visit as they are exposed to “threatening” stimuli. At some point, there likely is even a mixture of anxiety and fear for some patients. Understanding the patient’s “nervous” behavior as anxiety, fear, or a combination of the two is a crucial first step in determining strategies for intervention that will be most efficacious for improving the patient experience.
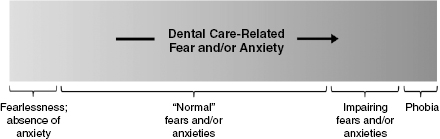
Fear and anxiety no longer are considered binary phenomena, as people do not fit neatly into “fearful” or “nonfearful” groups. Instead, fear and anxiety can be more accurately conceptualized as dimensional in nature. Contemporary models of both fear and anxiety suggest that each construct exists on a continuum (McNeil et al., 2012b). At one end of the continua, a patient may essentially have complete lack of treatment-related fear or anxiety. At the other end, a patient may have such extreme fear or anxiety that his or her symptoms are consistent with DSM criteria (e.g., APA, 2013) for Specific Phobia or another (likely anxiety) disorder. Between the two ends of the continua, there exists a range of situation-specific dental care-related fear or anxiety experiences, including those that are “normal,” those that involve only seldom and insignificant fear/anxiety behaviors, and those that involve more frequent or impairing fear/anxiety behaviors or complete avoidance. Along these spectra are patients who hate visiting the dentist, but nonetheless are able to attend appointments; that is, they experience and report fear, but do not avoid (entirely). A model of the dental fear/anxiety continua is illustrated in Figure 12.1. Considering the dental care-related fear and/or anxiety experience in this way allows clinicians to interact with patients in an individualized manner, tailoring patient management approaches to be appropriate and effective for reducing the situation-specific, idiosyncratic, and dynamic fear or anxiety experience.
Fig. 12.1. Model of the continua of dental care-related anxiety and dental care-related fear across the general population.
Etiology of Dental Care-Related Fear and Anxiety
A number of mechanisms have been proposed in order to describe the development, maintenance, and life-course of dental care-related fear and anxiety. Once thought to have direct antecedents almost always in childhood, dental care-related anxiety and fear can appear at various stages across the life span (Milgrom et al., 1988; Locker et al., 1999b; Thomson et al., 2009), although childhood onset nevertheless is the most common. While a full review of each of these hypotheses is beyond the scope of this chapter, a basic examination of the major ideas will shed some light on the complex phenomena. In trying to discern the determinants of dental fear and anxiety, it is important to be cognizant that human behavior is multidetermined; it is unlikely that there is “one” factor that predisposes or produces dental anxiety or fear. It also is critical to consider whether one is trying to predict dental anxiety/fear across an entire population as a whole (including the entire continua of dental anxiety and dental fear) or for a subpopulation (e.g., persons with high dental anxiety and/or fear, people who are dental avoidant); the larger the constituent group, the more likely that factors which affect only particular subgroups will be submerged in statistical analyses and that individual difference factors will be overlooked.
Conditioning
Dental care-related fear and anxiety may, for many patients, be conditioned via prior exposure to painful or traumatic dental experiences (Weiner & Sheehan, 1990). Fear or anxiety responses may, through classical conditioning, form and be strengthened when an association is made between dental treatment-related stimuli and aversive experiences such as pain, discomfort, or lack of control (Kent, 1985; Davey, 1989). A classic example reveals how a patient may develop a fear of the dentist or dental care-related stimuli: A tooth restoration that involves pain, accompanied by the sound of a dental drill and the smell of the dental clinic, reinforces an association between negative physical and emotional states and treatment-related stimuli, making future anxiety or fear responses more likely. When the individual returns to the dental clinic, the drill sound and smells of the office (now “conditioned stimuli”) alone provoke fear.
Dental care-related fear or anxiety responses also can be learned and perpetuated through operant conditioning, in which fear or anxiety behaviors (e.g., panic symptoms, crying, squirming, and avoidance) are reinforced, either through positive reinforcement, negative reinforcement, or both. Parents, for example, may inadvertently use positive reinforcement (essentially encouraging a behavior by doing something that is at least immediately rewarding) by being overly solicitous in response to their child’s expressed fears about an upcoming dental appointment, or even agreeing with the child’s prediction that it will be “terrible,” instead of using distraction, focusing on the child’s coping abilities, or other more positive responses. Negative reinforcement (essentially actions that remove some ongoing unpleasant situation) also can promote dental fear. For example, an already highly fearful patient who is in a dental chair, with a procedure about to be performed may squirm, complain of “nervousness,” and may have high cardiovascular reactivity. The compassionate dentist might interrupt treatment and suggest the patient come back another day when the patient is feeling “up to” having the procedure. While well intentioned, the dentist’s behavior actually negatively reinforces fear by removing the immediate “threat” of the procedure, delaying it until some indeterminate future time. (What might be a better strategy would be to complete at least part of the treatment, to avoid reinforcing fear behavior, and to give the patient the sense of self-efficacy in completing some dental treatment. Alternately, preventing or reducing the fear through behavioral and/or pharmacological means also might be ideal.)
This latter example not only portrays negative reinforcement, but exemplifies how Mowrer’s (1939) two-factor theory of learning extends the conditioning hypotheses of the development of dental care-related fear and anxiety to explain the maintenance of the phenomena and the related treatment avoidance behavior. First, fear is conditioned to environmental cues, such as the sights, sounds, and smells of the dental office, and that conditioned fear motivates the person to leave the office (i.e., “escape”). Second, if the patient does indeed leave the office, perhaps with the encouragement of the dentist, then getting away from the cues of the dental environment counterintuitively reinforces dental fear, which will make it more difficult for the patient to return in the future. According to this theory, conditioned fear and anxiety are maintained as a result of subsequent avoidance of treatment since avoidance permits the learned association between dental treatment-related stimuli and negative physical and emotional states to remain strong, as no opportunities to learn otherwise (i.e., that not all dental experiences are negative) are afforded to the patient. With treatment avoidance added to the mix, a “vicious cycle of dental fear” only exacerbates the learned fearful and anxious responses to dental treatment. Patients in such a cycle suffer from dental care-related anxiety and fear, which results in delayed dental visit attendance patterns, which yield more dental problems, thus producing symptom-driven treatment-seeking patterns (and, as a result, more painful dental treatment experiences), ultimately reinforcing the conditioned dental care-related fear or anxiety (see Weinstein, 1990; Armfield, Stewart, & Spencer, 2007).
The conditioned or learned association between previous dental trauma and dental care-related fear and anxiety may be rather specific. That is, dental care-related fear and anxiety may be unrelated to most other types of trauma. With regard to previous traumatic experiences that are not dentally related (e.g., tragic death of a loved one, violent crime, natural disaster, war), no definitive association has been found between trauma and dental care-related fear and/or anxiety (Oosterink, de Jongh, & Aartman, 2009a; Humphris & King, 2011). Nevertheless, an association has been found between previous sexual trauma (i.e., sexual assault) and dental care-related anxiety (Humphris & King, 2011).
Traumatic conditioning is regarded as neither necessary nor sufficient to describe the etiology of all fears and phobias (Mineka & Sutton, 2006). Instead, observational/vicarious learning and verbal/instructional learning also can play a role as pathways in the development and maintenance of a fear or phobia (Rachman, 1977, 1990). There is strong evidence that such a contemporary conditioning model can be applied to dental phobias and dental care-related anxiety (see Davey, 1989). Through experience and association, patients learn to be fearful of dental treatment, dental professionals, and the dental situation. Individual differences in dental fear or anxiety conditioning are the result of both differences in experience and, quite importantly, genetic/biological differences that differentially predispose individuals to develop and maintain the fears or anxieties. Notably, patients may not be able to recall a traumatic dental visit that played some role in the development of dental care-related fear and/or anxiety even if it occurred; it is well known that accuracy of recall of events, even some salient ones, is sometimes poor (see Mineka & Sutton, 2006). Just because a patient does not remember a traumatic dental visit does not mean there has not been fear conditioning as a result of a painful or uncomfortable previous experience. Some patients with a history of traumatic dental visits and associated dental care-related fear and/or anxiety simply may not be able to remember such visits, as the memories may be forgotten, repressed, or otherwise so emotionally laden that trying to recall them is cognitively blocked.
Social Learning
Some dental patients are fearful of dental treatment, the dental clinic, or oral healthcare providers even though they never have encountered a painful or negative experience (Milgrom, Weinstein, & Heaton, 2009). Perhaps their fears and anxieties about the dental situation have been transmitted to them via social or observational learning, or directly shared information. In such routes of anxiety/fear acquisition, people learn that dental treatment is uncomfortable, distressing, or painful via witnessing emotional arousal in others, information sharing (e.g., “Getting your wisdom teeth out really hurts!”), and/or otherwise hearing stories from parents, friends, others, or mass entertainment or media outlets. While such patients may never have had a negative dental experience themselves, they may learn from others that dental care is threatening; therefore, the experience, or anticipation of it, may become fear- or anxiety-inducing. For example, a patient may be informed that she needs root canal therapy and, in response, demonstrates a strong fear reaction and perhaps even a desire to instead get an extraction, due to her negative perceptions of endodontic care, learned from the popular media (to which she has been exposed from an early age).
Vicarious dental care-related anxiety and fear has been documented in children, who likely learn to be fearful or anxious from parents or siblings (Melamed & Williamson, 1991). There is, in fact, evidence that parents’ dental care-related fear and fear-driven dental avoidance behavior is predictive of their adolescents’ fear and avoidance behavior (McNeil et al., 2013a). Intergenerational transmission of dental care-related fear and anxiety likely is, at least in part, the result of observational learning. Dental professionals, when assessing dental care-related fear and anxiety and treating fearful or anxious patients, should not assume that previous, personally experienced dental trauma exists or that socially learned fears and anxieties are any less intense or impairing than fears and anxieties that developed by way of other mechanisms. Social and observational learning can have a great impact, and in some patients, may be the primary etiological factor in the development and maintenance of dental care-related anxiety and fear.
Biological Influences
It is important to note that biological factors can have a part in the development and maintenance of dental care-related fear and anxiety in some individuals, or may be protective factors in others. Consistent with contemporary thought in psychology and behavioral neuroscience, individual biological and genetic factors can be seen as predisposing certain patients to be more or less likely to develop dental care-related fear and/or anxiety and/or other forms of psychopathology. Essentially, genetic differences make some patients more susceptible than others to develop fears and/or anxieties through the learning-, cognitive-, personality-, and/or pain-based etiological mechanisms. Though there is a limited literature on the role of genetics and other biological factors in the etiology of dental care-related fear and anxiety, initial work suggests that they may serve as a diathesis (or vulnerability) for the development and/or maintenance of high levels of fear and anxiety.
The vulnerability may be more general, such as with neuroticism, which is a fairly heritable trait, and one that is associated with dental care-related anxiety (Vassend, Roysamb, & Nielsen, 2011). Or, the risk may be more specific, such as a predisposition to pain sensitivity and/or local anesthetic insensitivity, which is related to a genetic variation (Binkley et al., 2009). At present, this preliminary literature suggests that dental care-related fear is heritable (e.g., Ray et al., 2010; Randall et al., 2012), with the suggestion that biologically, dental care-related fear is intimately tied to fear of pain (Randall et al., 2012).
Cognitive Factors
For many fearful or anxious dental patients, cognitions play a key part in their experience; misperceptions, negative thoughts, and patterns of thinking that include worries about danger or lack of control are common in individuals with anxiety disorders. Patients with greater levels of dental care-related fear and anxiety often engage in catastrophizing or misappraising dental treatment as more dangerous than it is, overestimating the likelihood of negative outcomes that may result from dental treatment. Such cognitions, if frequent and severe enough, produce a particularly negative response to dental treatment. Some categories of misperceptions which often predict patient anxiety/fear include uncontrollability, unpredictability, dangerousness, and disgustingness (Armfield, 2010c). In general, catastrophizing and lack of cognitive control are critical moderators of dental care-related anxiety and fear (de Jongh et al., 1994). Current cognitive models of dental care-related fear suggest that abnormal fear may be acquired through a cognitive vulnerability, whereby a pattern of thinking that involves consistent misperceptions of stimuli as overly threatening yields the development of clinically significant levels of dental care-related fear and anxiety (Armfield, 2006). This cognitive vulnerability likely is the result of previous experiences and a genetic/biological predisposition that interacts with the environment. Understanding how a patient perceives all aspects of the dental treatment experience, encouraging realistic and appropriate appraisals, and correcting misperceptions when necessary, may be a critical aspect of anxiety/fear reduction for some patients. If these individuals view the dental treatment experience more accurately, they may be less likely to perceive relatively neutral stimuli or occurrences as threatening or traumatic and therefore will be less likely to develop fears or anxieties related to dental treatment.
Beliefs about dental treatment generally, and providers specifically, are important in understanding the development and maintenance of dental care-related fear and anxiety for some dental patients (Milgrom et al., 2009). Cognitions related to the appraisal of dental professionals and the dental profession may make an individual patient more or less likely to be fearful of or anxious about dental treatment; negative beliefs about dental treatment and unfavorable attitudes toward dental professionals are strongly correlated with dental care-related anxiety/fear (Doerr et al., 1998). Beliefs that affect dental care-related fear and anxiety and impact treatment-seeking patterns generally center on attitudes of trust/distrust, judgments about dentist–patient communication, and desire for control (Abrahamsson, Ohrn, & Hakeberg, 2009).
Beliefs about predictability and control in the dental situation can be important elements of dental care-related fear and anxiety. For some patients in particular, perceived lack of control may be an especially critical variable when considering the etiology of the fear and/or anxiety. For example, patients who have a high desire for control and low perceived control in the dental situation report the highest degrees of dental care-related anxiety and distress, a finding that is observed when patients anticipate dental care that is either imminent or not immediate (Logan et al., 1991). Women, as a group, have a greater desire for control as well as a more profound perception of lack-of-control in dental settings, relative to men, who have less desire for control and sense less lack-of-control in that setting (Liddell & Locker, 1997). Similarly, younger adults desire more control and perceive a lesser degree of control during dental treatment than do older adults (Liddell & Locker, 1997). The desire for control and the perception of lack of control, then, are cognitions that can partially account for dental care-related fear and anxiety in some people.
Personality
Many decades ago, mental health professionals utilizing a psychodynamic framework suggested that dental care-related fear and anxiety was the manifestation of specific unconscious drives/motivations and unresolved internal conflicts. Without significant evidence for those claims, the approach changed, to postulate that personality factors (i.e., stable, consistent, and predictable behavior patterns), broadly, were important to understanding the etiology of dental care-related fear and anxiety. Nevertheless, early work in approaching these problems from a personality perspective was not particularly useful in terms of understanding the specific etiologies of dental care-related fear and anxiety, or in devising efficient assessment and treatment strategies. The focus in the field then shifted to behavior. More recent work utilizing personality assessment in the dental care-related anxiety and fear arena, however, has been more productive. Certain personality traits, such as neuroticism, can predispose individuals to develop and maintain fears or anxieties in general, and/or about dental treatment in particular (Vassend et al., 2011). Contemporary approaches to conceptualizing and assessing personality in this area have yielded important findings, such as that individuals with stable, long-standing dental care-related anxiety and fear seem to have a mixture of etiological factors, including personality features, such as being easily stressed, experiencing strong negative emotions, and being less sociable with others (Thomson et al., 2009).
Pain-Related Factors
For many patients, dental care-related fear and anxiety has some basis in either pain (i.e., orofacial pain sensitivity) and/or perceptions of or fears about pain. Heightened pain sensitivity may be responsible for the development of dental care-related fear or anxiety in patients who experience objectively similarly painful procedures as other, nonfearful or nonanxious patients (Bernstein, Kleinknecht, & Alexander, 1979; Wardle, 1982). Patients with a lower dental pain threshold and/or tolerance may, through behavioral or conditioning mechanisms, develop impairing dental care-related fear or anxiety as a result of exposure to what would be considered by others to be relatively painless procedures. It may be important for the dental practitioner to identify such patients and to pay particular attention to their comfort level as to limit the opportunities for fear/anxiety conditioning. Interestingly, a number of studies suggest that the experience of dental pain is, to some extent, also dependent on dental care-related fear and/or anxiety; patients with higher levels of fear and/or anxiety report more intense and long-lasting pain during dental injections (e.g., van Wijk & Makkes, 2008; van Wijk & Hoogstraten, 2009) and routine procedures, including scaling (e.g., Sanikop, Agrawal, & Patil, 2011; Tickle et al., 2012). Differential pain sensitivity can be both a precursor to, and the product of, dental care-related fear and anxiety. Relatedly, fear of pain has been found to be an important component of dental care-related anxiety (McNeil & Berryman, 1989; McNeil et al., 2001), and as already noted, these constructs are biologically linked in heritability analyses (Randall et al., 2012). Additionally, fear of dental pain, specifically, is an important element of dental care-related fear/anxiety (van Wijk & Hoogstraten, 2003). That is, fearing the pain associated with dental treatment (and not necessarily even experiencing painful procedures), may predispose or reinforce fears or anxieties about dental professionals and dental treatment. Being particularly fearful of the pain associated with dental treatment, and not the actual treatment per se, can result in avoidance of clinic visits. The interplay of fear of pain, pain sensitivity, and anxiety is complex and important (see Chapter 7, Environmental, Emotional, and Cognitive Determinants of Dental Pain) and should be considered when assessing and treating dental care-related fears and anxieties.
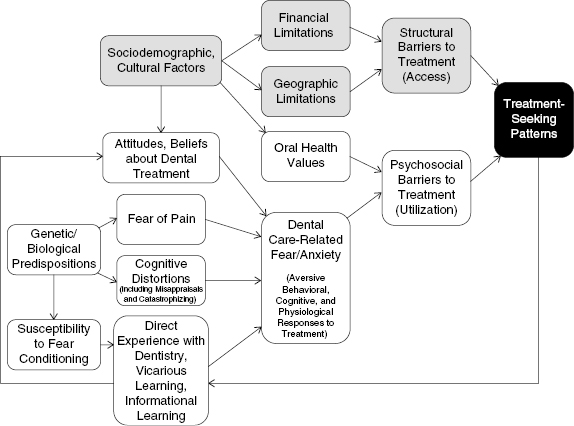
Taken together, these etiological hypotheses highlight the complex nature of dental care-related fear and anxiety. To complicate the situation further, dental care-related fear and anxiety are not necessarily stable traits, as they can fluctuate with time as a result of shorter-term emotional states (i.e., depression), psychosocial factors (e.g., divorce, work-related stress), or as a result of new experiences and/or intervention. Paired with other psychosocial factors, as well as sociodemographic factors, the impact of dental care-related fear and anxiety on patient treatment-seeking behavior can be extreme, even life-threatening, in relation to avoidance of necessary dental care. Figure 12.2 presents a model that accounts for many of the concepts discussed here and provides some organizational context through which to better understand dental care-related fear and anxiety and their relation to utilization of oral health care. There are other models of dental anxiety/fear that focus on the vicious cycle (Weinstein, 1990; Armfield et al., 2007) or on cognitive aspects (Armfield, Slade, & Spencer, 2008). Dental care-related fear and anxiety generally are static, although they can change across the life span, but apparently only in some individuals (Thomson et al., 2009). The variables depicted in the conceptual model may change via dental experience, other life events, or psychosocial intervention.
Fig. 12.2. Conceptual model of the impact of dental care-related fear and anxiety on treatment-seeking patterns, and relation to associated variables.
Classification of Patients with Dental Care-Related Fear and Anxiety
Efforts have been made to produce categories based on the etiology and/or manifestation of dental care-related fear and anxiety. One method of classifying people with dental care-related anxiety involves placing the anxious/fearful individual into one of two etiological categories: exogenous or endogenous (Weiner & Sheehan, 1990). Individuals characterized as having exogenous dental care-related anxiety are thought to have developed anxiety/fear as a result of conditioning through traumatic experiences or observational learning, while individuals characterized as having endogenous dental care-related anxiety/fear are thought to have developed dental-specific distress as a result of some other underlying mood or anxiety disorder. Considering typical ages of onset of dental care-related anxiety/fear, groups with distinct characteristics seem to surface, providing support for an exogenous versus endogenous classification system (Locker et al., 1999b). Across groups, individuals with child-, adolescent-, and adult-onset dental care-related anxiety and fear show similar psychological, behavioral, and cognitive reactions to dental treatment. Nevertheless, a family history of dental care-related distress and traumatic dental experiences (characteristic of exogenous anxiety) is predictive of child-onset dental care-related anxiety/fear, while trait anxiety, multiple fears, and a general hostility and mistrust toward dentists (characteristic of endogenous anxiety) is predictive of adolescent- and adult-onset dental care-related anxiety/fear (Locker et al., 1999b).
Another classification system, one with strong clinical applicability, has been forwarded by Milgrom et al. (1985). Known as the “Seattle System,” this method of categorizing patients with dental care-related anxiety and fear places individuals into one of four categories based on the etiology and experienced symptoms of their fear or anxiety: (a) conditioned fear of dental treatment; (b) fear of physiological arousal during dental treatment (e.g., racing heart, panic, fainting); (c) generalized anxiety and/or multiple phobias; or (d) distrust of dentists. The Seattle System is a classification framework that has been evaluated in several fearful and/or phobic samples, with results demonstrating its clinical utility (e.g., Moore, Brodsgaard, & Birn, 1991; Roy-Byrne et al., 1994; Locker, Liddell, & Shapiro, 1999a).
Yet another approach to classification has involved dental patients across the continuum of anxiety and fear. Focusing on fear of pain and its relation to dental care-related anxiety and fear (e.g., McNeil & Berryman, 1989), cluster analytic techniques identified three subgroups of oral surgery patients: (a) high fears of both pain and dental care, (b) high fear of pain but low fear of dental care, and (c) low fears of both pain and dental care (McNeil et al., 2013c).
Finally, using a longitudinal approach, Thomson et al. (2009; Poulton et al., 2001) have identified various trajectories of dental care-related anxiety across three decades of life. Included in this conceptualization are individuals comprising the following trajectories (with percent of the total sample noted in parentheses): (a) stable nonanxious low anxiety (39%), (b) stable nonanxious medium anxiety (38%), (c) adult-onset anxious (8%), (d) recovered (2%), (e) stable anxious (7%), and (f) late-adolescent-onset anxious (6%). Of note is how well this approach maps onto the various child-, adolescent-, and adult-onset types determined by Locker et al. (1999b). Also noteworthy is the very small proportion of individuals who have recovered from problem levels of dental anxiety/fear. This work on the natural history of dental anxiety is of vital importance to the field, as it is not mired in cutoff scores, and allows a view of the development, as well as maintenance or recovery from, varying levels of dental anxiety across the life span.
Epidemiological Considerations
Both dental care-related fear and anxiety are prevalent phenomena with far-reaching and clinically relevant implications. In the USA, approximately 45% of adults report at least moderate levels of dental care-related fear (Dionne et al., 1998). Between 5% and 10% of the same population indicates that they avoid necessary and accessible dental treatment as a result of this dental care-related anxiety/fear (Milgrom et al., 2009). Similar statistics have been observed in other parts of the world, including Australia (Armfield, Spencer, & Stewart, 2006), Denmark (Moore et al., 1993), India (Kumar et al., 2009), Japan (Domoto et al., 1988), the Netherlands (ten Berge et al., 2002), Singapore (Chellappah et al., 1990), and Sweden (Klingberg, Berggren, & Noren, 1994). Compared to other fears and phobias, dental care-related fear and phobia are common; dental care-related fear ranks the fourth most reported fear, after snakes, heights, and physical injuries, and dental phobia ranks third most prevalent after acrophobia (i.e., fear of heights) and arachnophobia (i.e., fear of spiders; Oosterink, de Jongh, & Hoogstraten, 2009b). When studied in terms of anxiety, versus fear, meta-analysis results suggest that between 10% and 20% of American adults report a high level of dental care-related anxiety (Smith & Heaton, 2003). Though there have been immense improvements in both the quality of and comfort associated with dental treatment, there apparently has been no decrease in the nationwide prevalence of dental care-related anxiety in the USA since the 1950s (Smith & Heaton, 2003).
Dental care-related anxiety/fear is associated with a number of demographic and psychosocial variables. Perhaps most profound are gender differences. There is a consistent findi/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


