14
Management of Children’s Distress and Disruptions during Dental Treatment
- It is often the real or perceived unpleasantness of the dental situation that generates a child’s desire to escape; this leads, in turn, to distress and disruptive behavior.
- The key to good behavior management is the creation of a pleasant experience for the child by minimizing fear, anxiety, and discomfort.
- Dentists can control many variables that directly and significantly influence behavior through the use of clear communication, frequent praise, modeling, engaging distractions, and brief breaks.
- These strategies are also effective for children with special needs; however, these children may also benefit from additional preparation, and the dentist should consider physiological, developmental, and/or language differences.
Introduction
The skills required to manage a distressed and disruptive child during dental treatment are as fundamental to successful treatment as are handpiece skills and knowledge of dental materials. These skills are important because the ability to manage distress and disruptive behavior has direct implications for the quality of dental care. In addition, disruptive child behavior increases delivery time and the risk of injury to the child. Not surprisingly, behavior management with children is a topic of considerable interest for dentists.
There have been significant advances in dental technology, materials, and training that have made the dental experience for children more pleasing and enjoyable. Nevertheless, dentists must still be able to perform precise procedures on children who are distressed and disruptive (Sheller, 2004). Indeed, distress and disruptions continue to be prevalent and problematic within the child population (Bo, 2004). Although most children seen in clinical practice comply with the examination and treatment, estimates suggest that 20–25% of all children exhibit disruptive problems at the dental clinic (Raadal, Milgrom, & Weinstein, 1995; Brill, 2000). In addition, these problems are strongly correlated with age, where younger, preschool-aged children are more challenging than school-aged children (Allen, Hutfless, and Larzelere 2003). Furthermore, these problems are compounded when invasive procedures are required. For example, data from private practice suggest that the younger the child and the more threatening or invasive the procedure, the more often negative, disruptive behavior is observed (Brill, 2000).
Due to greater rates of disruptive behavior and noncompliance, some populations present particular behavioral challenges in the dental environment. As one example, preschool children can be so difficult to manage that many general practitioners are not willing to provide care for them when anything more than an examination or prophylaxis is required (Cotton et al., 2001). This is of particular concern, given increasing interest in improving preschool children’s access to dental care (Waldman & Perlman, 1999; Edelstein, 2000; Grembowski & Milgrom, 2000). Children with intellectual and developmental disabilities also have a greater potential for behavior problems in the office setting, causing some dentists to be unwilling to see these patients or to limit their practice (Salama, Kebriaei, & Durham, 2011). Perhaps as a result, children with intellectual and developmental disabilities start receiving dental care later than their typically developing peers (Chi et al., 2011). Unfortunately, these children have a great need for dental care, as they often have poorer overall oral health than typically developing children (Waldman, Perlman, & Swerdloff, 2001), and may have an increased need for dental care due to differences in oral physiology, medication side effects resulting in reduced saliva and increased caries, and potentially reduced compliance with home hygiene (Feigal, Jensen, & Mensing, 1981).
Why Children Are Disruptive
Changing child behavior during dental treatment requires understanding why children might be disruptive and noncompliant during dental treatment and also understanding how to help children learn more cooperative, new behaviors. Many variables have been considered by dentists in trying to understand why children are disruptive. For example, dentists have been concerned that permissive parenting styles have adversely influenced child behavior in the dental clinic (Casamassimo, Wilson, & Gross, 2002). Previous investigations have also explored general maternal anxiety, maternal dental anxiety, child anxiety, and child temperament as predictors of child disruptive behavior during treatment (Johnson & Baldwin, 1969; Radis et al., 1994; Quinonez et al., 1997). However, none of these investigations have identified reliable predictors of disruptive behavior in the dental clinic. Empirical studies have been unable to identify a clear link between parent or child characteristics and disruptive behavior in the clinic. Even when investigators have sought to establish a more direct link between disruptive behavior in the dental clinic and disruptive behavior outside the clinic, none has been found (Dunegan et al., 1994). Finally, Allen et al. (2003) actually looked at parenting style in an effort to predict disruptive behavior in the clinic. They found that the only reliable predictor of disruptive behavior was, not surprisingly, age of the child. Younger children were more disruptive no matter what parenting practices were used. Older children were better, no matter what parenting practices were used. More importantly, no single parenting style was a predictor.
Although years of speculation have continued to suggest that factors outside the clinic are critically important, years of empirical research have indicated that outside influences do not seem to have reliably strong influences on disruptive behavior in the clinic. This should not suggest that outside or past influences have no impact at all; only that the impact is unpredictable. Perhaps more important is the fact that dentists have almost no control over these past or outside influences. One must question whether it is useful to continue to focus efforts on attempts to identify predictors over which dentists have little influence. Furthermore, there is every reason to believe that the variables that have the most direct and significant influence on disruptive behavior lie directly within the dental operatory and are variables over which dentists do have some control.
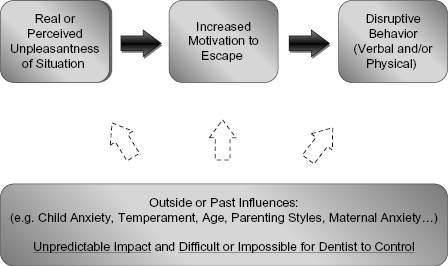
Consider for a moment the experience of a young child undergoing restorative dental work. The child must lie on their back, open their mouth, remain still, and have someone wearing a mask and gloves insert sometimes multiple instruments that make unusual noises, create unfamiliar sensations, and sometimes inflict discomfort or pain. Fear would be an expected reaction, especially in young children (2–5 years of age) where fear of strangers and strange situations, fear about separation from their caregiver, and fear about noises, masks, and novel stimuli are common experiences (Barrios & O’Dell, 1998). But even in older children, there may be anxiety about a potentially unpleasant situation as children tend to overpredict the discomfort they will experience during treatment (Carlsen et al., 1993). That is, merely the anticipation of discomfort can evoke anxiety or fear. Furthermore, whether one appeals to anxiety, fear, pain, or a combination of all three, the fact that some children might be interested in escaping the dental treatment environment is not surprising. Of course, there are some children who are neither fearful nor anxious, but are merely oppositional because they find it unpleasant to be required to do something they wish not to do. Although these distinctions are very difficult to make in a brief dental visit (Harper & D’Alessandro, 2004), the distinction may not be critical to success, since the child’s motivation remains the same: to escape an unpleasant (perceived or real) situation. For most children, efforts to escape involve verbal distress such as crying, moaning, or complaining, and/or behavioral distress such as flinching, blocking, thrashing, or turning away. Nevertheless, it is the real or even perceived unpleasantness of the situation that generates the motivation to escape, and it is the motivation to escape that generates disruptive behavior. It is not surprising then that there is a strong correlation between threatening invasive procedures and negative, disruptive behavior (Brill, 2000), and that these problems are more prevalent in younger children (see Fig. 14.1).
Fig. 14.1. Factors related to disruptive behavior in the dental office.
Of course, not all children view the dental experience as unpleasant. Still others may view the experience as unpleasant, but have learned to accept some unpleasantness in life without attempts to escape. Nevertheless, those who are disruptive are, in effect, communicating via their behavior that they find the experience unpleasant and that they would rather be elsewhere. The task of the dentist interested in behavior management then ultimately becomes one of reducing the unpleasantness of the dental experience. Indeed, were the dental experience devoid of unpleasantness (whether from fear, anxiety, discomfort, or demands), the incidence of disruptive behavior would be markedly less if not nil. The goal then becomes one of reducing the unpleasantness or increasing the pleasantness of the treatment environment. The following approaches represent both time-honored and innovative methods of reducing the unpleasantness of the dental experience.
Positive Approaches to Behavior Management
Inherent in any behavior management approach is the requirement of time. Regardless of the approach, dentists who wish to learn and implement strategies designed to increase the pleasantness of the dental experience for a child must take time. Unfortunately, dentists are not reimbursed for time spent engaged in behavior management, nor are they reimbursed for learning those skills (Sheller, 2004; Glassman et al., 2009), so procedures must be easy to teach, learn, and implement in a busy clinical practice. Although some leaders in the field have challenged dentists who would be unwilling to spend “a few minutes shaping the behavior” of a disruptive child just because that time is not reimbursable (Sheller, 2004), it is clear that interventions must be cost-effective. That is, dentists are most likely to use procedures that produce the most amount of benefit (i.e., improved behavior) with the least amount of time and effort (i.e., time and effort not associated with actual restorative dentistry).
More recently, dentists have also had to consider the risks associated with behavior management as part of the benefit analysis. Changing standards with respect to what constitutes “reasonable care” means dentists must be increasingly cautious about using behavior management procedures that parents might find objectionable (e.g., Bross, 2004; Oueis et al., 2010). Guidance from professional organizations also reflects this change, as the American Academy of Pediatric Dentistry has removed “hand-over-mouth” from its clinical guidelines, and clearly states that options such as protective stabilization, sedation, and general anesthesia only be implemented after consideration or failure of less invasive strategies (American Academy of Pediatric Dentistry, 2011). These views have largely been reflected in the educational and practice culture of pediatric dentists for some time; for example, most advanced programs no longer teach the hand-over-mouth procedure, viewing it as an unacceptable behavior management technique (Adair et al., 2004), and most pediatric dentists do not employ the technique at all (Adair et al., 2004). As a result, this chapter will focus on techniques that appear reasonably benign, have some empirical support, and appear to be cost-effective.
Reduction of Discomfort
Certainly one way to reduce management difficulties in children is to explore strategies for reducing the pain and discomfort associated with invasive restorative dental procedures themselves. For example, numerous studies have been conducted in an effort to achieve a painless injection (e.g., Houpt et al., 1997), including the use of topical anesthesia and prolonged injection time (e.g., Maragakis & Musselman, 1996; Matthews et al., 1997). Prolonged injection time has been pursued as a means of reducing the pain associated with an injection, because it is understood that pain is created, at least in part, by the volume pressure changes exerted by the injected solution on small nerve fibers (e.g., Travell, 1955). Slowing the rate of administration may be one means of controlling the volume pressure. However, it can be technically difficult to achieve when done manually (e.g., Chan, 2001).
Several controlled investigations by Allen and colleagues with school-aged children explored the efficacy of a computerized local anesthetic delivery system, designed to reduce the pain of the injection by delivering anesthetic at a constant rate, pressure, and volume. Three well-controlled investigations demonstrated that, when used properly, a computerized system for slowing the rate of anesthesia administration and thereby controlling the volume pressure did result in children who were significantly less disruptive and who required less restraint to manage when compared with a traditional manual injection method (Asarch et al., 1999; Gibson et al., 2000; Allen et al., 2002). However, the computerized system took four times longer to administer an injection, and preschool-aged children became restless with the lengthy injection duration. Some dentists may become restless too. Nevertheless, even though restless, the younger children were still significantly less disruptive. Although the computerized system clearly requires an investment in time at the beginning of the session, it may be well worth the time for some dentists, given the reduction of child disruptive behavior.
Parent Presence in Operatory
Dentists have long questioned whether having a parent present in the operatory is a reasonable approach to behavior management. Over 40 years ago, Frankl put the question to the test. In a nicely controlled scientific investigation, Frankl and colleagues demonstrated that preschool-aged children (3–6) were less distressed and disruptive when their parent remained in the operatory as a passive observer (Frankl, Shiere, & Fogels, 1962). Not surprisingly, this effect was strongest for the youngest children. Separating young children from their parents may introduce separation anxiety and thereby increase the unpleasantness of the visit. Subsequent studies of parental presence during dental procedures have repeatedly shown that parental presence has either no impact or a positive impact (e.g., Venham, Bengston, & Cripes, 1978; Pfefferle et al., 1982) on child behavior. Yet, surveys have demonstrated that many dentists are concerned that parental presence will disrupt the child (e.g., Marcum, Turner, & Courts, 1995). This concern is not entirely unfounded. Research has demonstrated that parents can negatively impact child behavior during injections if the parent frequently draws attention to and offers reassurance about the procedures. However, parents can actually be of help if they are instructed to talk with their child about nonprocedure-related topics (Gonzalez, Routh, & Armstrong, 1993). This might include talking about plans for an upcoming vacation, describing a recent experience with a pet or friend, or discussing favorite toys or activities. Results from these types of studies have led to recommendations that dentists simply need to be sure to tell parents exactly what is expected of them (Harper & D’Alessandro, 2004). Research to date would suggest that parents be instructed to either remain silent or to talk about things unrelated to the ongoing procedures. These recommendations are important because significant numbers of parents want to be with their children, especially young children (e.g., Kamp, 1992; Peretz & Zadik, 1998).
Of course, dentists are concerned not only with the impact of the parent on the child, but also with the impact of the parent on the dentist. A parent in the operatory can create distractions and discomfort for the dentist (Marcum et al., 1995), who may feel more relaxed and comfortable when parents remain in the waiting room. Because dentists who are more relaxed and comfortable are more likely to perform better, many dentists allow parents in the operatory for the initial visits with a young, preschool-aged child, but subsequently ask that parents remain in the waiting room. This would appear to be a reasonable approach.
Modeling
Allowing a child to view other children who are undergoing dental treatment can both prepare them for what to expect, and provide a demonstration of appropriate behavior during the treatment (Kuhn & Allen, 1994). A number of studies have utilized videotaped models of children demonstrating good behavior and coping while experiencing dental treatment. Results have generally been quite positive, showing significant benefits, including reduction in disruptive behavior and anxiety-related behavior for children who viewed the tapes (e.g., Melamed et al., 1975, 1978). However, the use of video models has not been widely adopted by practicing dentists (Allen, Stanley, & McPherson, 1990; Wright, Giebartowski, & McMurray, 1991), perhaps due to financial or logistic challenges (Kuhn & Allen, 1994).
Another option is the use of live models, for example, via a clinic schedule that allows children to first observe another child receiving dental treatment, and then serve as a model for the next child (e.g., Stokes & Kennedy, 1980). Interestingly, this line of research suggests that even for more invasive procedures, this strategy improves behavior for both the observer and for the model (Williams, Hurst, & Stokes, 1983). Overall, the empirical evidence suggests that school-aged children can benefit from observing peers and/or older siblings undergoing dental treatment showing “how it’s done.” Some dentists accomplish this through an “open bay” concept, in which children entering the treatment area readily see peers participating in dental exams. Other dentists schedule visits for entire preschool classes, where children can not only explore the environment, but also observe peer models who volunteer to sit in the chair, lie back, and allow the dentist to look in their mouths (Allen & Hosterman, 2011). So far, these techniques have not been routinely integrated into dental practices, perhaps due to financial, privacy, and/or logistic challenges. Nevertheless, there is evidence that video or live modeling contributes to improved behavior.
Effective Communication
The manner in which a dentist communicates with a child can certainly impact the pleasantness of the dental environment. This requires recognizing that children understand best when language is kept simple and concrete. This has commonly led to recommendations that dentists replace dental terminology with more easily understood words such as “raincoat” for rubber dam, “vacuum cleaner” for suction, and “tooth paint” for sealant (Wright, 2000). Table 14.1 includes a more comprehensive list of child-friendly terms for standard dental tools. Perhaps more important is to recognize that children learn best through experience. That is, children are active learners who learn best through direct interaction with the world. Indeed, the most effective educational programs for young children are ones that communicate concepts and ideas through experience (e.g., Weikart, 2002). Not surprisingly then, dentists have also traditionally valued communication that incorporates direct interaction and experience. Originally called the Tell-Show-Do (Addelston, 1959), this experiential technique involves describing for children, in simple terms, what is about to occur (Tell) and then allowing them to see, feel, explore, and manipulate the tools or instruments (Show), before beginning any procedure (Do). This might involve allowing the child to operate the chair, to squirt the water syringe, to feel the high speed on the back of their hand, or to use the suction to clean up a puddle of water. Although neither of these approaches (i.e., simplifying language, tell-show-do) has been empirically evaluated, each could reasonably be expected to increase the pleasantness of dental experience and both approaches are sensitive to children’s developmental communication needs.
Table 14.1 Child-Friendly Terms for Standard Dental Tools
| Dental tool | Child-friendly term |
|---|---|
| Mirror | Princess mirror, Tooth counter |
| Explorer | Tooth counter, checker, or toucher |
| Prophy angle | Tickly toothbrush, Princess toothbrush |
| Suction | Mr. Thirsty |
| Air/water | Mr. Windy, Squirt gun |
| High-speed handpiece |
Stay updated, free dental videos. Join our Telegram channel
VIDEdental - Online dental courses
 Get VIDEdental app for watching clinical videos
Get VIDEdental app for watching clinical videos

|