Cysts of Orofacial Region
Classification of Cysts of Orofacial Region
Theories of Cyst Expansion
Malcolm Harris (1975) summarized various theories that explain cyst expansion. Mural growth theory, hydrostatic enlargement, and role of bone resorbing factors are the theories that have been proposed by various authors to explain enlargement of cysts.
Mural Growth Theory
The mural growth theory is explained by two propositions.
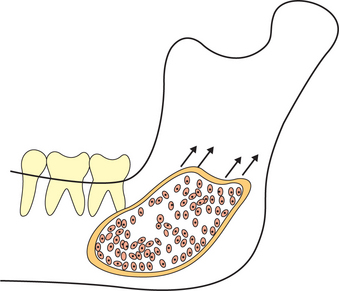
1. Peripheral cell division: It is proposed that the cyst enlarges at the peripheries because of active division of the cells of the epithelium lining the cyst (Figure 1). It is believed that the division of these cells is a response to any irritating stimulus. The theory further suggests that once the stimulus is withdrawn the cyst regresses in size. This theory has not found many supporters as cyst regression will result in irregular inner surface of the cyst as the bone surrounding the cyst offers resistance. One should remember that the contents of the cyst will support the cystic lining and it can cause rapid resorption of surrounding bone to accommodate the enlarging cyst.
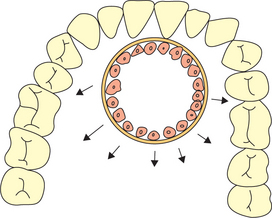
Figure 1 Enlargement of the cyst at the peripheries due to active division of the cells of the epithelium lining the cyst
2. Accumulation of cellular contents: This theory was proposed by Kramer (1974) to explain the enlargement of OKCs. He proposed that as mural squames are shed off the lining epithelium they accumulate, thereby increasing the cyst volume. The sites of expansion and growth are represented by finger-like projections which are zones of active cell division or proliferation (Figure 2).
Kubota et al (2000) studied the role of interleukin-1 alpha (IL-α) and matrix metalloproteinase-9 (MMP-9) in the expansion of odontogenic cysts. They found that an active form of MMP-9 was present in OKC fluids more frequently than dentigerous cyst and radicular cyst fluids. However, proMMP-9 was present in all cyst fluids.
Kubota et al (2002) in their study showed that interleukin (IL)-1 α stimulates enzymatic degradation of the extracellular matrices of the bone around the cysts. This induces expansion of OKC.
Oka et al (2005) studied the effects of positive intra-cystic fluid pressure in OKCs. They proposed that the positive intracystic pressure may play a crucial role in OKC growth via stimulating the expression of IL-1 in epithelial cells.
Role of Bone Resorbing Factors
Harris et al (1973) proposed that cyst tissue (capsule) contains a combination of prostaglandins E2 and E3, which are considered very potent bone resorbing factors. It is believed that the leukocytic and bone resorbing factors aid in bone resorption. It is believed that the keratocyst secretes comparatively lesser amount of bone resorbing factors per unit surface area compared to other cysts (periodontal cyst, radicular cyst). This explains the burrowing nature or intramedullary growth of the keratocyst.
Odontogenic Cysts
Eruption Cyst
The eruption cyst is a type of soft tissue cyst associated with erupting teeth. It surrounds the crown of a tooth that has already erupted through bone but impeded by the overlying soft tissue. Kuczek et al (2003) reported a case where a boy developed an eruption cyst who was administered cyclosporin A (potent immunomodulatory agent) subsequent to a cardiac transplantation. Cyclosporin A was replaced with tacrolimus and there was no new cyst formation. The authors proposed that the formation of an eruption cyst may be an adverse effect of cyclosporin A in children with erupting teeth.
Dentigerous Cyst (Follicular Cyst)
Clinical features
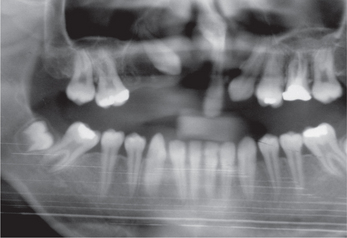
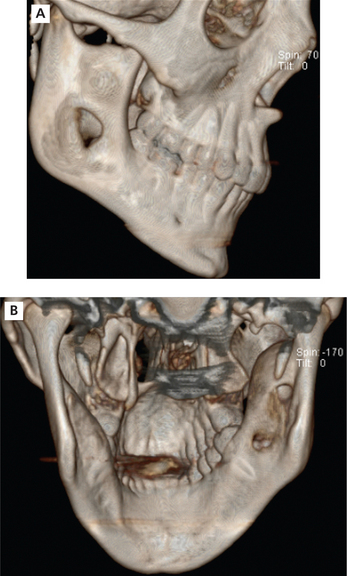
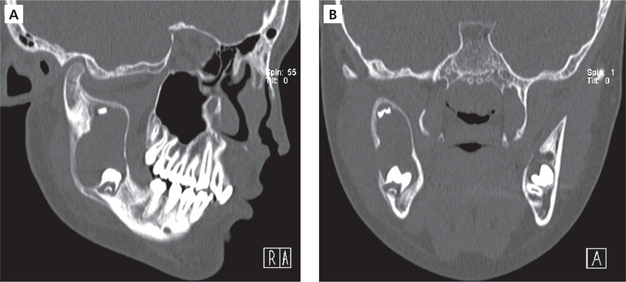
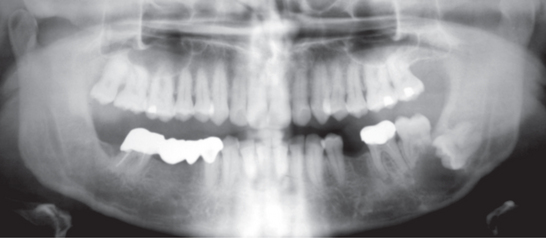
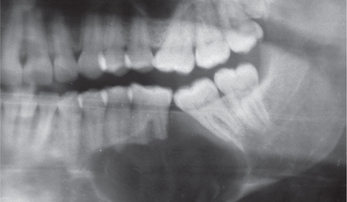
It occurs frequently in association with impacted mandibular (Figure 3), maxillary third molars (Figure 4), and maxillary canines (Figure 5). Dentigerous cyst is commonly seen in the 2nd and 3rd decades of life. Males are relatively more predisposed. It grows aggressively and produces facial asymmetry, bony expansion, displacement and resorption of teeth. Entire ramus might be hollowed if associated with mandibular third molar (Figure 6A, B). In case of maxillary canine, anterior maxilla is expanded. There will be no pain unless secondarily infected. On aspiration, yellow-colored fluid is obtained.

Figure 3 Orthopantomograph (OPG) showing dentigerous cyst (multilocular) associated with impacted right lower third molar and a supernumerary tooth displaced superiorly approximating the sigmoid notch. Courtesy: Dr NVS Sekhar Reddy
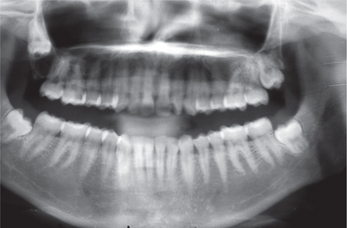
Figure 4 Orthopantomograph (OPG) showing dentigerous cyst (unilocular) associated with the right upper third molar. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
Radiographic features
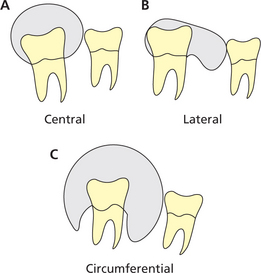
Radiographically, dentigerous cysts exhibit three different presentations, namely, the central, lateral and circumferential types. In central variety, the cyst symmetrically envelops crown. The cyst occurs on lateral aspect of the crown in lateral variety and envelops crown entirely in circumferential variety (Figure 7). Dentigerous cyst may appear as welldefined unilocular or multilocular radiolucency (Figure 8A, B). Occasionally these cysts may cause displacement and resorption of the adjacent teeth (Figure 9). Large cysts often cause expansion of the cortical plates.
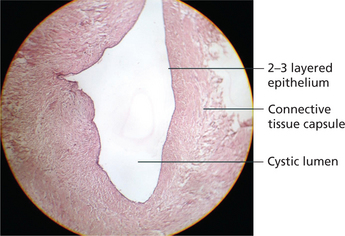
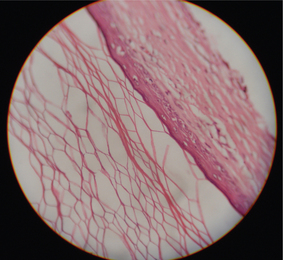
Histologic features
It has no characteristic microscopic features. It has cyst lining and connective tissue wall. The connective tissue wall consists of very loose fibrous connective tissue and sparse collagenized myxomatous tissues. It has presence of odontogenic epithelium (Figure 10). The inflammation leads to presence of Rushton bodies of hematogeneous origin in the lining epithelium. Cholesterol clefts might be present.
Potential complications
The odontogenic cyst has following complications: the development of mural ameloblastoma (Figure 11), squamous cell carcinoma and mucoepidermoid carcinoma.
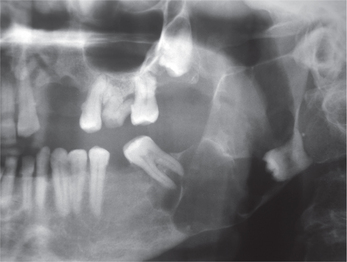
Figure 11 Orthopantomograph (OPG) showing multilocular radiolucency associated with the impacted mandibular third molar. The radiograph showing displacement of the third molar and the lesion extends to involve the entire ramus and apices of the second molar. The lesion was histopathologically diagnosed as mural ameloblastoma. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
Odontogenic Keratocyst
Keratocystic odontogenic tumor is described in Chapter 13 on Tumors of Orofacial Region.
Orthokeratinized Odontogenic Cyst
Philipsen in 1956, in his study of jaw cysts, described a distinct form of OKC which showed an orthokeratinized pattern. Wright et al (1981) reported 60 cases of orthokeratinized odontogenic cyst (OOC) and compared with OKC and found that the OOC appears to be a distinct clinicopathologic entity. It was suggested that this cyst be called OKC, orthokeratinized variant. Iamaroon et al (2004) compared the proliferation index of the epithelial cells between OKC, OOC, dentigerous cyst and ameloblastoma. He concluded that OKC should be considered a benign tumor rather than simply an odontogenic cyst and OOC as a non-aggressive cystic lesion.
Histopathologic features
Orthokeratinized odontogenic cyst has a thin epithelial lining with a luminal surface of orthokeratin. The basal cell layer contains flattened squamous or cuboidal cells and a well-developed granular cell layer (Figure 13).
Radiographic features
Orthokeratinized odontogenic cyst presents either as a well-defined unilocular or multilocular radiolucency. Radiographically, OOC may resemble a dentigerous cyst when it is unilocular and resembles ameloblastoma when it is multilocular. Occasionally, it may cause cortical plate expansion and thinning of the lower border of the mandible. Roots of teeth may be displaced (Figure 14). However, resorption of roots is seldom seen.
Gingival Cysts of Adults
Gingival cysts of adults are rare odontogenic cysts of developmental origin. The epithelial lining of these cysts are thin non-keratinized and are thought to arise from the rests of dental lamina. Some authors suggest that these cysts arise from the traumatic implantation of surface epithelium.
Radiographic findings
Hegde (2004) reported a rare finding (supposedly the first case in literature) calcifications within cystic lumen of the gingival cyst.
Calcifying Epithelial Odontogenic Cyst (Gorlin Cyst)
The calcifying odontogenic cyst can either occur as an intraosseous (central) or extraosseous (peripheral) lesion. The peripheral form is very rare. The incisor and canine regions are the most common sites of involvement. The maxilla is more commonly affected. It can occur at any age. However, most cases are seen in the 2nd decade of life.
Types
Cystic entity
 Type 1: A simple monocystic type of typical Gorlin’s cyst, with or without dentinoid calcified tissue.
Type 1: A simple monocystic type of typical Gorlin’s cyst, with or without dentinoid calcified tissue.
 Type 2: Monocystic odontoma creative type, with all the characteristics of the previous type, except that the hard tissue was complex or compound odontoma, and a presence of ameloblastic fibroma tissue in the cystic wall extending into the surrounding tissue.
Type 2: Monocystic odontoma creative type, with all the characteristics of the previous type, except that the hard tissue was complex or compound odontoma, and a presence of ameloblastic fibroma tissue in the cystic wall extending into the surrounding tissue.
 Type 3: Monocystic ameloblastomatous proliferating type which was marked by ameloblastomatous proliferation both in the walls and in the lumen, and hard dental tissue which consisted of dentinoid formation in connection with islets of epithelia in the connective wall.
Type 3: Monocystic ameloblastomatous proliferating type which was marked by ameloblastomatous proliferation both in the walls and in the lumen, and hard dental tissue which consisted of dentinoid formation in connection with islets of epithelia in the connective wall.
Clinical features
It produces slow growing painless non-tender swelling of jaws (Figures 16 and 17). It occurs more in 2nd decade of life. It is commonly seen in the anterior part of the jaws. In the maxilla, the canine region is the most commonly affected site. In the mandible, the cyst is rarely found posterior to the first molar. Occasionally the cyst may be seen crossing the midline. On aspiration, it yields viscous granular yellow fluid. According to Wood et al, 68% of cases occur in mandibular molar area. At least 52% cases are associated with unerupted tooth, occasionally associated with pain.
Radiographic features
The radiographic features are quite variable. The central lesion may be radiolucent with a variable margin that is smooth and well-defined or, irregular and poorly defined. It might contain small foci of calcified material. It is usually present as a unilocular radiolucency. However, in about 5–13% of the cases, it may present as multilocular radiolucency. Intraosseous lesions may produce expansion of the lingual cortical plate. Resorption of the roots of adjacent teeth is frequently seen (Figure 18).
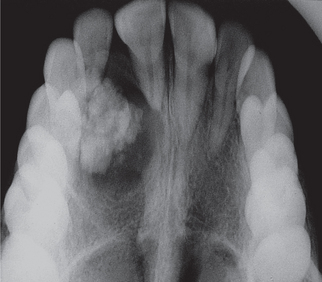
Figure 18 Maxillary occlusal radiograph showing a well-defined unilocular radiolucency in the incisor-canine region containing radiopaque foci of calcification. Resorption of the apex of the right central incisor can be appreciated. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses